Chapter 21
advertisement

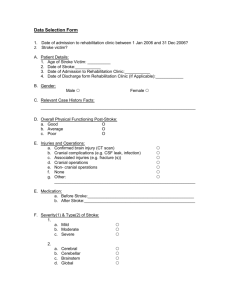
Chapter 23 CHAPTER 23 – NUTRITION AND DISORDERS OF THE UPPER GASTROINTESTINAL TRACT CHAPTER SUMMARY Disorders of the upper gastrointestinal tract involve conditions affecting the esophagus and stomach. The nutrition needs of patients with these conditions are altered as a result of the increased risk for nutrient malabsorption and deficiency, and discomfort related to their condition. Conditions affecting the esophagus include dysphagia and gastroesophageal reflux disease. Dysphagia can include oropharyngeal dysphagia and esophageal dysphagia. Complications of dysphagia include risk of aspiration, reduced food consumption leading to malnutrition and weight loss and increased risk of dehydration. Dysphagia can be diagnosed via barium swallow studies, endoscopy and neurological exams. Dietary intervention for dysphagia includes diet modifications following the National Dysphagia Diet guidelines, which should be done with client acceptance of mechanically altered foods in mind. The cause of gastroesophageal reflux disease (GERD) is inappropriate weakening or relaxing of the lower esophageal sphincter related to various medical conditions. GERD can have severe consequences, if left untreated, including reflux esophagitis, esophageal ulcers, esophageal stricture and Barrett’s esophagus. Treatment of GERD includes drug therapy, dietary modifications and lifestyle modifications including elevating the head of the bed six-inches, avoiding lying down after eating, limiting foods that weaken the lower esophageal sphincter pressure or increase gastric acid secretion and avoidance of cigarettes and alcohol. Surgical intervention may be indicated in severe cases of GERD. Conditions affecting the stomach include dyspepsia, nausea and vomiting, gastritis, peptic ulcer disease, and gastric surgery. Abdominal pain can be difficult to diagnose and the cause can be evasive even with a thorough physical exam. Dyspepsia refers to the general symptoms of indigestion in the upper abdominal area including stomach pain, heartburn, fullness, nausea, and bloating. Causes of dyspepsia include peptic ulcers, GERD, motility or malabsorptive disorders, gall bladder disease, some medication and dietary supplements, and systemic disorders such as diabetes mellitus, renal disease and heart failure. Controlled research studies have been unable to find associations between specific foods and dyspepsia. Nausea and vomiting can accompany multiple medical conditions, be a side effect of medications or be triggered by a variety of environmental conditions. Treatment of nausea and vomiting involves finding and correcting the underlying disorder. Gastritis, inflammation of the stomach mucosa that can be acute or chronic, has multiple causes including Helicobacter pylori infection and use of non-steroidal antiinflammatory drugs (NSAIDs). Treatment for gastritis is individualized to the patient’s symptoms. Peptic ulcer disease (PUD) is primarily caused by Helicobacter pylori infection, and secondarily by NSAID use. The physiological effects of emotional stress are an important consideration in understanding the etiology of PUD. Treatment of PUD includes drug therapy and individualized dietary modifications. Gastric surgery includes treatment for severe PUD (rarely used), stomach cancer and obesity (bariatric surgery). Dietary modifications following gastric surgery, regardless of the reason for the surgery, share the common objective of avoiding the symptoms of dumping syndrome. Post-surgical complications and the effects on nutrition status include unintended substantial weight loss, steatorrhea, malabsorption of vitamin D and calcium thus increasing the risk for bone disease and increased risk for the development of anemia related to impaired absorption of iron and vitamin B 12. Bariatric surgery involves long-term diet and lifestyle modifications and careful follow-up to avoid nutrient deficiencies. Highlight 23 discusses dental health and its relationship with chronic illness. 356 Chapter 23 357