Chapter 18 Functions of the GI Tract Secretion: Functions of the GI
advertisement
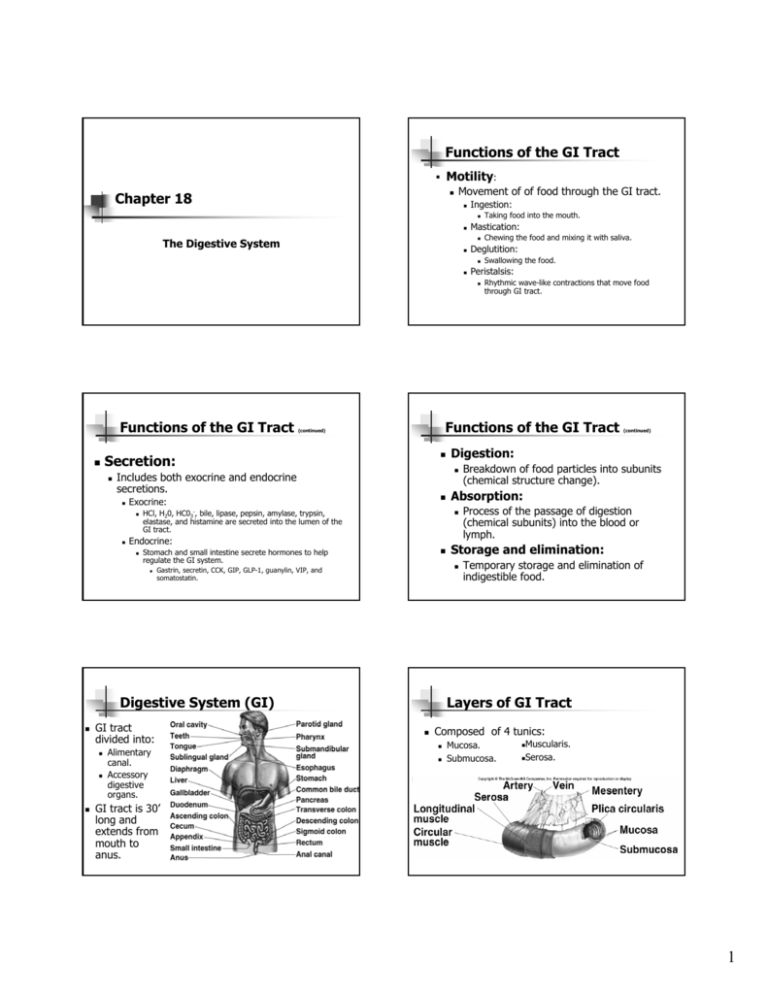
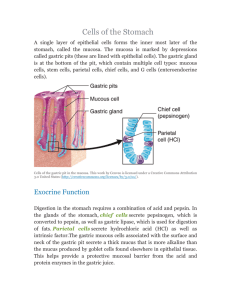
Functions of the GI Tract Motility: Chapter 18 Movement of of food through the GI tract. Ingestion: Mastication: Deglutition: Peristalsis: The Digestive System Functions of the GI Tract Exocrine: HCl, H20, HC03-, bile, lipase, pepsin, amylase, trypsin, elastase, and histamine are secreted into the lumen of the GI tract. Stomach and small intestine secrete hormones to help regulate the GI system. GI tract divided into: Alimentary canal. Accessory digestive organs. (continued) Breakdown of food particles into subunits (chemical structure change). Process of the passage of digestion (chemical subunits) into the blood or lymph. Storage and elimination: Gastrin, secretin, CCK, GIP, GLP-1, guanylin, VIP, and somatostatin. Digestive System (GI) Rhythmic wave-like contractions that move food through GI tract. Absorption: Endocrine: Swallowing the food. Digestion: Includes both exocrine and endocrine secretions. Chewing the food and mixing it with saliva. Functions of the GI Tract (continued) Secretion: Taking food into the mouth. Temporary storage and elimination of indigestible food. Layers of GI Tract Composed of 4 tunics: Mucosa. Submucosa. Muscularis. Serosa. GI tract is 30’ long and extends from mouth to anus. 1 Esophagus From Mouth to Stomach Mastication (chewing): Enzyme that can catalyze the partial digestion of starch. Deglutition (swallowing): Oral phase is voluntary. Pharyngeal and esophageal phases are involuntary. Cannot be stopped. Larynx is raised. Epiglottis covers the entrance to respiratory tract. Most distensible part of GI tract. Functions of the stomach: Stores food. Initiates digestion of proteins. Kills bacteria. Moves food (chyme) into intestine. Gastric Glands Secrete gastric juice: Goblet cells: mucus. Parietal cells: HCl and intrinsic factor (B12). Chief cells: pepsinogen. G cells: gastrin. Several others… Rate of 2-4 cm/sec. Stomach Insert 18.4a Circular smooth muscle contract behind, relaxes in front of the bolus. Followed by longitudinal contraction (shortening) of smooth muscle. Stomach Produced by a series of localized reflexes in response to distention of wall by bolus. Wave-like muscular contractions: Begins as a voluntary activity. Involves 3 phases: Peristalsis: Mixes food with saliva which contains salivary amylase. Contractions of the stomach churn chyme. (continued) Insert fig. 18.5 Mix chyme with gastric secretions. Push food into intestine. Digestion and Absorption in the Stomach Proteins partially digested by pepsin. Carbohydrate digestion by salivary amylase is soon inactivated by acidity. Alcohol and aspirin are the only commonly ingested substances absorbed. 2 Protective Mechanisms of Stomach Parietal and chief cells impermeable to HCl. Alkaline mucus contains HC03-. Tight junctions between adjacent epithelial cells. Rapid rate of cell division (entire epithelium replaced in 3 days). Small Intestine Each villus is a fold in the mucosa. Covered with columnar epithelial cells interspersed with goblet cells. Lamina propria contain lymphocytes, capillaries, and central lacteal. Intestinal Contractions and Motility Absorption in Small Intestine Majority of absorption (90%) takes place here Duodenum and jejunum: 2 major types of contractions occur in the small intestine: Slow movement. Pressure at the pyloric end of small intestine is greater than at the distal end. Segmentation: Bile salts, vitamin B12, electrolytes, and H20. Major contractile activity of the small intestine. Contraction of circular smooth muscle. Large Intestine Outer surface bulges outward to form haustra. Little absorptive function. Mix chyme. Defecation Absorbs H20, electrolytes, several vitamin B complexes, vitamin K, and folic acid. Intestinal microbiota (bacteria) produce significant amounts of folic acid and vitamin K. Bacteria ferment indigestible molecules to produce short-chain fatty acids. Insert fig. 18.14 Peristalsis: Carbohydrates, amino acids, lipids, iron, and Ca2+. Ileum: Insert fig. 18.12 Waste material passes to the rectum. Occurs when rectal pressure rises and external anal sphincter relaxes. Defecation reflex: Does not contain villi. Longitudinal rectal muscles contract to increase rectal pressure. Relaxation of internal anal sphincter. Excretion is aided by contractions of abdominal and pelvic skeletal muscles. Push feces from the rectum. 3 Major Categories of Liver Function Accessory Organs of Digestion Bile Production and Secretion The liver produces and secretes 250–1500 ml of bile/day. Bile pigment (bilirubin) is produced in spleen, bone marrow, and liver. Derivative of the heme groups (without iron) from hemoglobin. Gallbladder Converted by bacteria in intestine to urobilinogen. Urobilogen is absorbed by intestine and enters the hepatic vein. Recycled, or filtered by kidneys and excreted in urine. Pancreas Pancreatic Juice Exocrine: Acini: Sac-like organ attached to the liver. Stores and concentrates bile. Contraction of the gallbladder ejects bile into the common bile duct into duodenum. Contains H20, HC03- and digestive enzymes. Insert fig. 18.26 Secrete pancreatic juice. Endocrine: Islets of Langerhans: Secrete insulin and glucagon. 4 Regulation of Gastric Function Cephalic Phase Stimulated by sight, smell, and taste of food. Activation of vagus: Stimulates chief cells to secrete pepsinogen. Directly stimulates G cells to secrete gastrin. Directly stimulates ECL cells to secrete histamine. Indirectly stimulates parietal cells to secrete HCl. Gastric motility and secretion are automatic. Extrinsic control of gastric function is divided into 3 phases: Cephalic phase. Gastric phase. Intestinal phase. Continues into the 1st 30 min. of a meal. Gastric Phase Intestinal Phase Arrival of food in stomach stimulates the gastric phase. Gastric secretion stimulated by: Distension. Chemical nature of chyme (amino acids and short polypeptides). Stimulates G cells to secrete gastrin. Stimulates chief cells to secrete pepsinogen. Stimulates ECL cells to secrete histamine. Histamine stimulates secretin of HCl. Inhibits gastric activity when chyme enters the small intestine. Arrival of chyme increases osmolality and distension. Activates sensory neurons of vagus and produces an inhibitory neural reflex: Hormone secretion: Inhibit gastric activity: Intestinal Reflexes Gastroileal reflex: Ileogastric reflex: Increased gastric activity causes increased motility of ileum and movement of chyme through ileocecal sphincter. Distension of ileum, decreases gastric motility. Intestino-intestinal reflex: Overdistension in 1 segment, causes relaxation throughout the rest of intestine. Inhibits gastric motility and secretion. In the presence of fat, enterogasterone inhibits gastric motility and secretion. Somatostatin, CCK, and GLP-1. Secretion of Pancreatic Juice Secretion of pancreatic juice and bile is stimulated by: Secretin: Occurs in response to duodenal pH < 4.5. Stimulates production of HC03 by pancreas. Stimulates the liver to secrete HC03 into the bile. CCK: Occurs in response to fat and protein content of chyme in duodenum. Stimulates the production of pancreatic enzymes. Enhances secretin. Stimulates contraction of the sphincter of Oddi. 5