Respiratory System
Respiratory System
To Accompany: Anatomy and Physiology Text and
Laboratory Workbook, Stephen G. Davenport, Copyright
2006, All Rights Reserved, no part of this publication can be
used for any commercial purpose. Permission requests
should be addressed to Stephen G. Davenport, Link
Publishing, P.O. Box 15562, San Antonio, TX, 78212
Respiratory System
• The respiratory system consists of the
–
–
–
–
–
–
–
–
–
–
nose,
nasal cavity,
pharynx,
larynx,
trachea,
primary bronchi, and the
lungs, which contain the
smaller bronchi, the
bronchioles, and the
alveoli (air sacs).
• The respiratory system consists of the organs
that are involved in the delivery and exchange of
gases between the air and the blood.
• Functions of the respiratory system include the
–
–
–
–
(1) delivery of air to and from the exchange surfaces,
(2) protection of respiratory surfaces,
(3) sound production, and
(4) providing for the sense of smell (olfaction).
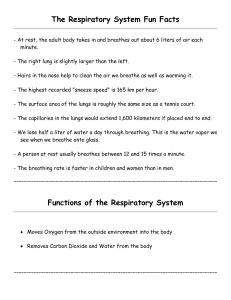
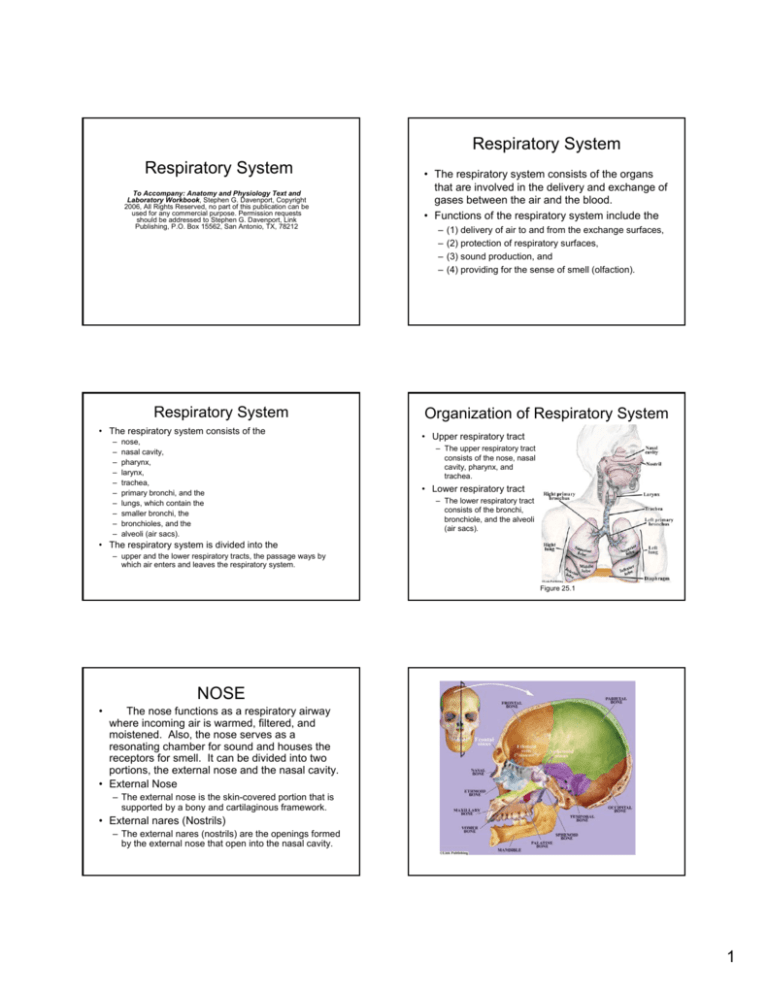
Organization of Respiratory System
• Upper respiratory tract
– The upper respiratory tract
consists of the nose, nasal
cavity, pharynx, and
trachea.
• Lower respiratory tract
– The lower respiratory tract
consists of the bronchi,
bronchiole, and the alveoli
(air sacs).
• The respiratory system is divided into the
– upper and the lower respiratory tracts, the passage ways by
which air enters and leaves the respiratory system.
Figure 25.1
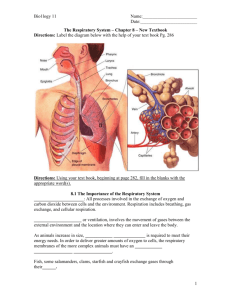
NOSE
•
The nose functions as a respiratory airway
where incoming air is warmed, filtered, and
moistened. Also, the nose serves as a
resonating chamber for sound and houses the
receptors for smell. It can be divided into two
portions, the external nose and the nasal cavity.
• External Nose
– The external nose is the skin-covered portion that is
supported by a bony and cartilaginous framework.
• External nares (Nostrils)
– The external nares (nostrils) are the openings formed
by the external nose that open into the nasal cavity.
1
NASAL CAVITY
NASAL CAVITY
• Conchae
•
The nasal cavity is the space within and posterior to
the external nose. It is lined with a mucous membrane.
The external nares (nostrils) are the anterior entrances
to the nasal cavity. The posterior openings of the nasal
cavity, the internal nares, enter the nasal portion of the
pharynx (nasopharynx).
• Vestibule
– The conchae are thin bony projections that extend inward from
each side of the nasal cavity to almost reach the nasal septum.
Each side of the nasal cavity has a superior, middle, and inferior
concha. The conchae function to increase the surface area of
the cavity. They form air passages called the meatuses.
• Meatuses
– The meatuses are the air passageways formed beneath the
conchae. Each meatus is named in relation to its corresponding
concha: the superior, the middle, and the inferior meatus. As air
passes through the meatuses, it is moistened, warmed, and
filtered.
– A nasal vestibule is the short chamber that originates at each
nostril and leads into the nasal cavity.
• Nasal septum
– The nasal septum is the vertical partition that divides the nasal
cavity into right and left sides. The anterior portion is formed by
cartilage and the posterior portion is formed by the perpendicular
plate of the ethmoid bone and the vomer bone.
• Internal nares
– The internal nares are the posterior openings of each side of the
nasal cavity into the nasopharynx.
PHARYNX
•
•
The pharynx is the tube that
extends inferiorly from behind the nose
to the base of the larynx (voice box).
Nasopharynx
– The nasopharynx is the uppermost
portion of the pharynx. It communicates
with the nasal cavity by the internal nares
and the oropharynx at the level of the
soft palate. Located in each of its lateral
walls is the opening into the
pharyngotympanic tube (also called
auditory, or eustachian tube). The
pharyngeal tonsil is located at its
superior, posterior border.
•
Oropharynx
– The oropharynx extends from the level of
the soft palate to the level of the hyoid
bone. Anteriorly, the oropharynx opens
into the oral cavity. The uvula is a small Figure 25.2
process which hangs downward from the
posterior border of the soft palate.
Figure 25.2
PHARYNX
LARYNX
•
The larynx (voice box) is
positioned at the superior aspect
of the trachea and consists of
cartilages, extrinsic ligaments,
muscles, and associated tissues.
•
Thyroid cartilage
• Laryngopharynx
– The laryngeal part of the pharynx
extends from the level of the hyoid
bone downward to the cricoid
cartilage of the larynx and to the
origin of the esophagus.
– The thyroid cartilage is the upper
and largest cartilage of the
trachea. Its right and left anterior
borders fuse to form the projection
known as the Adam’s apple.
•
Cricoid cartilage
– The cricoid cartilage is inferior to
the thyroid cartilage and forms the
lower part of the larynx.
•
Figure 25.2
Figure 25.2
Epiglottis
– The epiglottis is a flap of elastic
cartilage that is attached to the
thyroid cartilage and projects
upward. It closes the glottis, the
opening of the larynx, during
swallowing.
2
TRACHEA
LARYNX
•
Vestibular folds (false vocal
cords)
•
The trachea is the airway that originates from the
larynx and extends downward to the level of the fifth
thoracic vertebra where it branches into the right and left
primary bronchi.
• Mucosa
– The vestibular folds (false
vocal cords) are the upper pair
of vocal folds. They are not
used in the production of
sound. They provide a
protective function for the true
focal folds.
•
– The vocal folds (true vocal
cords) are the lower pair of
vocal folds. Each is formed
from an epithelial covered
ligament that consists mostly
of elastic tissue. The vocal
cords function in the
production of sound and are
located inferior to the
vestibular folds (false vocal
cords).
•
– The mucosa is the innermost region of the trachea. Its lining is
pseudostratified ciliated columnar epithelium. The epithelium
contains numerous goblet cells that produce abundant mucus.
The cilia function to move mucus to the pharynx.
Vocal folds (vocal cords)
Figure 25.2
Glottis
• Submucosa
– The outer region to the mucosa is the submucosa. The
submucosa consists of a layer of connective tissue that contains
numerous seromucous glands and blood vessels. The
seromucous glands produce a combination of serous fluid and
mucus that is emptied though ducts to the surface of the
mucosa.
– The glottis is the passageway
between the vocal cords.
TRACHEA
Trachea – Lab Activity 2
• Adventitia
– The adventitia is the outer region of the trachea. The
adventitia consists of fibrous connective tissue and is
supported by incomplete rings of hyaline cartilage.
The cartilage rings are open at the posterior surface
of the trachea and are described as shaped like the
letter “C” (C-rings). The C-rings function to support
and increase the flexibility of the trachea. A small
band of smooth muscle, the trachealis muscle
connects the posterior portions of the C-rings.
Contraction of the trachealis muscle functions to
Figure 25.3
Trachea – Lab Activity 2
Trachea – Lab Activity 2
Figure 25.5
Figure 25.4
3
LUNGS
LUNGS
• The lungs are located within the thoracic
cavity on each side of the region called the
mediastinum.
• Each lung is surrounded by a microscopic
cavity, the pleural cavity, which contains
serous fluid produced by the serous
membrane surrounding each lung. The
portion of the serous membrane on the
surface of the lungs is called the visceral
pleura. The portion of the serous
membrane external to the visceral pleura
and surrounding each lung is called the
parietal pleura.
– The right lung consists of three lobes: the
superior, middle, and inferior lobes.
– The left lung consists of two lobes, the
superior and inferior lobes.
– The cardiac notch of the left lung is an
indentation occupied by a portion of the heart.
LUNGS
LUNGS
ELASTICITY AND PRESSURES
• The elasticity of the lungs allows expansion and
recoil during breathing.
– Expansion of the lungs results because of decreased
thoracic pressure produced by contraction of muscles
external to the lungs, such as the diaphragm and
external intercostal muscles.
– Lung recoil is a passive event that results because of
the recoil of the lung’s elastic fibers and the surface
tension of alveolar fluid. Recoil tension from the lungs
is transferred from the lung’s visceral pleura through
the surrounding serous fluid to the parietal pleura and
supporting tissues.
Figure 25.6
LUNGS
ELASTICITY AND PRESSURES
• Thus, the pleural cavities (serous fluid) have an
intrapleural pressure, a negative pressure
produced by the tendency of the lungs to recoil.
Intrapleural pressure is slightly less than
atmospheric pressure and alveolar pressures
(alveolar, or intrapulmonary pressure, varies
with each inspiration and expiration).
• Equalization of the intrapleural pressure and the
intrapulmonary or the atmospheric pressure
results in the recoil of the lung away from the
parietal pleura, and the lung collapses.
TRACHEA AND BRONCHIAL
TREE
Tracheobronchial Tree
The branching pattern of the bronchi is
often described as the bronchial or
respiratory tree.
4
Tracheobronchial Tree
•
The trachea divides into the right and left primary
bronchi, which begins the branching pattern called the
bronchial tree.
• Right Bronchus
– The shorter, wider, and more vertical right bronchus branches
into three secondary (lobar) bronchi. Each supplies one lobe of
the right lung (three lobes).
• Left Bronchus
– The left bronchus branches into two secondary (lobar) bronchi.
Each secondary bronchus supplies a lobe of the left lung (two
lobes).
– Secondary (lobar) bronchi
– Tertiary (secondary) bronchi
– Bronchioles
– Respiratory bronchioles (with alveoli)
– Alveolar ducts
– Alveoli
Structure of Trachea and Bronchial
Tree
• Trachea
The trachea, the large respiratory airway that
leads to the bronchial tree,
– supported by cartilage C-rings,
– has a limited amount of smooth muscle (the
posterior trachealis muscle) and
– is lined internally with pseudostratified ciliated
columnar epithelium.
Structure of Bronchial Tree
• Bronchi
show variations in structure as their size
decreases.
– Their supporting cartilage is formed by cartilaginous
plates, which decrease in thickness and number as
the bronchi become smaller. In the bronchiole
cartilage is completely lacking.
– The amount of smooth muscle increases as the
bronchi become smaller. In the bronchiole, smooth
muscle is abundant and functions in regulation of the
diameter of the bronchiole.
– The pseudostratified ciliated columnar epithelium
lining the trachea and bronchi changes to ciliated
cuboidal epithelium in the terminal and respiratory
bronchiole. Simple squamous epithelium is present in
the alveolar ducts and alveoli.
Figure 25.7
Lab Activity 3 – Lung Tissue
Figure 25.8
Bronchography is the x-ray examination of the tracheobronchial tree
after exposure to a radiopaque substance. The image produced is called a
bronchogram. bronchiole and alveoli are not shown in bronchograms because
the radiopaque material is filtered out of the air before it reaches their locations.
Figure 25.9
A scanning power photograph of a section of lung. The lung is extremely
porous because of the presence of air sacs, the alveoli.
5
Lab Activity 3 – Lung Tissue
Lab Activity 3 – Lung Tissue
• Bronchi
– The bronchi are the airways of the lungs. Bronchi are
lined with pseudostratified ciliated columnar
epithelium and their walls contain plates of supporting
hyaline cartilage.
• Bronchioles
Figure 25.10
Low power photograph of a section of lung. This photograph shows several
alveolar sacs associated with a bronchiole.
Lab Activity 3 – Lung Tissue
• Alveoli
•
The alveoli are the sites of gas exchange.
Alveoli organized into groups are called alveolar
sacs. Alveolar ducts connect alveolar sacs to
bronchiole. The wall of an alveolus consists of
alveolar epithelium and surrounded by a network
of capillaries and elastic fibers. The alveolar
epithelium and the capillaries function as sites of
gas exchange between the air and the blood.
Elastic fibers function in providing elasticity for
alveoli expansion during inhalation and providing
elastic recoil during the passive exhalation of air.
Lab Activity 3 – Lung Tissue
Alveolar epithelium
• Simple cuboidal cells
(type II cells)
– The simple cuboidal cells,
also called type II cells,
function in the production
of surfactant. Surfactant
reduces the surface
tension of water on the
alveolar surfaces, thus,
Fig 25.11
increasing lung
compliance. Lung
compliance refers to ability
of the lungs to expansion.
Having lung compliance
means that the lungs can
expand easily.
– Bronchioles are the thin wall extensions of the
bronchi. They contain abundant smooth muscle and
are called the airways of resistance regulation
because of their ability to undergo
bronchoconstriction and bronchodilation.
Lab Activity 3 – Lung Tissue
Alveolar epithelium
• Simple squamous cells
(type I cells).
– The simple squamous
cells, also called type I
cells, function in (1) gas
diffusion between air in the
alveolus and the capillaries
that cover the alveoli and
(2) produce the enzyme
called angiotensin
converting enzyme (ACE),
which converts angiotensin Fig 25.11
I to angiotensin II.
Angiotensin II is a powerful
vasoconstrictor and
functions in blood pressure
regulation.
Alveolar macrophages
• Alveolar macrophages defend the alveoli from
pathogens and other foreign substances. The
alveoli lack ciliated epithelium and are not a part
of the mucus escalator of the bronchiole,
bronchi, and trachea. The mucus escalator
continually moves inhaled substances to the
thorax where they are swallowed.
6
Lab Activity 4
Alveolar Macrophages in Smoker’s
Lung or Emphysema
Figure 25.12 The alveoli are enlarged
with thick fibrous (nonelastic) walls. The
slide also shows abundant carbon in the
tissue, which accumulated after years of
inhalation of small carbon particles
(probably from smoking).
Figure 25.13 High power photograph of
a macrophage from a pathology slide of
emphysema and smoker’s lung. This
macrophage is packed with small
particulate matter, especially carbon
particles.
Respiratory membrane
• The walls of the alveoli and the capillaries
consist of simple squamous epithelia and their
under lying basement membranes (basal
lamina).
– The two squamous epithelia (alveolar and capillary)
are fused by their underlying basement membranes
(basal lamina) to form the extremely thin respiratory
membrane. The respiratory membrane forms the
barrier between the air and the blood and functions in
allowing gas exchange by diffusion. Oxygen diffuses
into and carbon dioxide diffuses out of the blood.
Respiratory membrane
Pulmonary Ventilation
Figure 25.14
Illustrations and high power photograph of an alveolus showing the
structure of the respiratory membrane.
Pulmonary (respiratory) ventilation is
the exchange of air between the lungs
and the atmosphere.
Air Pressure
(Driving Force for Ventilation)
Air Pressure
(Driving Force for Ventilation)
• Air moves from an area of high pressure
to an area of low pressure. The pressure
of a gas is a result of the interaction
between the molecules of air. Air pressure,
or atmospheric pressure, is the pressure
produced by the weight of the atmosphere.
• At sea level atmospheric pressure is
expressed as one atmosphere, or 760
millimeters (mm) of mercury (Hg.).
• Boyle’s law states that the pressure and volume
of a gas are inversely proportional. Decreasing
the volume of a gas increases its pressure, and
increasing the volume of a gas decreases its
pressure.
• Thus, pulmonary ventilation, or breathing, is
based upon changing the pressure inside of the
lungs, the intrapulmonary pressure, in reference
to the pressure outside of the lungs.
7
Normal Quiet Breathing
• Normal quiet breathing means that
breathing is not forced.
• In normal quiet breathing both
diaphragmatic and costal breathing occur,
with exhalation being passive by relaxation
of the contracting muscles.
• Diaphragmatic breathing accounts for
most of the air exchange of normal quiet
breathing.
Diaphragmatic Breathing
•
In diaphragmatic breathing, contraction
of the diaphragm moves the diaphragm
downward, away from the thorax. This
results in an increase in the vertical
volume of the thorax. As volume
increases, intrapulmonary pressure
decreases and air flows into the lungs.
Relaxation of the diaphragm results in the
diaphragm moving upward decreasing the
volume of the thorax.
Costal Breathing
In costal breathing, contraction of the
external intercostal muscles moves the
ribs upward and outward. This movement
produces a horizontal increase in the
volume of the thorax. Increased thoracic
volume results in decreased
intrapulmonary pressure and air flows into
the lungs.
Figure 25.15
Illustration showing normal quiet breathing involving diaphragm and
intercostal muscles.
Forced Breathing
• Forced Inspiration
Forced inspiration involves contraction of
the
– external intercostal muscles,
– contraction of the diaphragm, and
– contraction of the inspiratory accessory
muscles, resulting in the maximal increased
volume of the thorax.
Forced Breathing
• Forced Expiration
Forced expiration involves contraction of
the muscles of expiration, which include
the
– internal intercostal muscles and
– abdominal muscles (such as the rectus
abdominus), resulting in the maximal
decreased volume of the thorax.
8
RESPIRATORY VOLUMES
Air exchange must be adequate to
maintain oxygen delivery to and carbon
dioxide removal from the body.
Figure 25.16
Forced inspiration and forced expiration involve maximal changes to
the volume of the thorax.
RESPIRATORY VOLUMES
• Two variables in the exchange of air,
– (1) the amount of air (respiratory volumes and
capacities) and
– (2) the rate of air exchange.
Respiratory Volumes and Capacities
• A respiratory volume is the amount of air
in a single respiratory event.
• A respiratory capacity is the sum of two or
more respiratory volumes.
• Spirometers
– Spirometers are instruments used to measure
the volume of air exchanged by the lungs.
Respiratory Volumes and
Capacities
• Tidal volume, TV
– The amount of air inhaled or exhaled in a normal
quiet breath.
• Inspiratory reserve volume, IRV
– Inspiratory reserve volume is the amount of air
inhaled above a normal quiet inspiration (tidal
volume).
• Expiratory reserve volume, ERV
– Expiratory reserve volume is the amount of air
exhaled after a normal quiet expiration (tidal volume).
Respiratory Volumes and
Capacities
• Residual volume, RV
– Residual volume is the amount of air remaining in the
lungs after complete exhalation. This air remains in
the airways and air spaces of the lungs.
• Inspiratory capacity, IC
– Inspiratory capacity is the amount of air that can be
inhaled after a normal quiet expiration. IC = TV + IRV
• Vital Capacity, VC
– Vital capacity is the maximum amount of air that can
be exhaled after a maximum inhalation.
VC = ERV + TV + IRV or VC = ERV + IC
9
Respiratory Volumes and
Capacities
• Total Lung Capacity, TLC
– Total lung capacity is the maximum amount of
air contained in the lung after a maximum
inhalation. TLC = RV + ERV + TV + IRV or
TLC = RV + VC
• Functional residual capacity, FRC
– Functional residual capacity is the amount of
air in the lungs after a normal quite expiration
(tidal volume). FRC = RV + ERV
Figure 25.17
Spirogram showing respiratory volumes and capacities.
Measuring Respiratory Volumes
Lab Activity 5
Hand-Held Spirometers
•
SAFETY PRECAUTIONS
Measuring Respiratory Volumes
Lab Activity 5
• Forced Expiratory Volume Timed (FEVT)
– A respiratory function test called the Forced
Expiratory Volume Timed (FEVT ) measures
the total air exhalation (vital capacity) as a
function of time intervals.
– Seventy five percent (75%) of the forced vital
capacity should be exhaled in the first one
second interval (FEV1 ).
– Consult the manufacture’s usage instruction
sheets for information on cleaning and
disinfection of equipment.
– Be absolutely sure that your equipment has
been adequately cleaned and disinfected
before usage.
– Insert a new sterile disposable mouthpiece
and disposable bacterial filter before use.
Determination of
vital capacity percentage
Determination of
one second volume percentage
Lab Activity 6
•EXHALE ONLY INTO THE SPIROMETER
Figure 25.18
Spirogram from a recording
spirometer. Determine the one second
percentage by dividing the one second
volume (4,000 ml.) by the vital capacity
(4,600 ml.) and multiply by 100. The
one second percentage is 4,000/4,600 =
.869 X 100 = 87%
•
A person’s vital capacity should be at
least 80% of his predicted vital capacity.
• Consult the tables at the end of this
chapter for the predicted vital capacities
for males and females.
• Determine your vital capacity percentage
by dividing your vital capacity by your
predicted vital capacity, and multiplying by
100.
10
Gas Movement and the Respiratory
Membrane
Gas Movement and the
Respiratory Membrane
Breathing allows air exchange for
the lungs.
• Alveolar air has a slightly higher concentration of
carbon dioxide and a slightly lower concentration
of oxygen than that found in atmospheric air.
• Atmospheric air is a mixture of gases and at sea
level is about 78.6% nitrogen, 20.9% oxygen,
and 0.04% carbon dioxide, and water vapor.
• In a mixture of gases, such as the atmosphere,
each gas has its own partial pressure. The
partial pressure of a gas in a mixture is the
pressure that the single gas exerts, and is
exerted as if it were the only gas in the
container.
Dalton’s Law of partial pressures
Partial pressures at the Alveoli
•
• States that the total pressure of a gas, such as the
atmospheric air, is the sum of the partial pressure of the
individual gases. At sea level, atmospheric pressure is
760 mm Hg.
• The partial pressure of each atmospheric gas at sea
level (in mm Hg.) is determined by multiplying its
percentage times the atmospheric pressure (in mm.
Hg.). At sea level (760 mm Hg.), the partial pressure of
nitrogen is 597 mm Hg. (78.6% X 760 mm Hg. =597 mm
Hg.), oxygen is 159 mm Hg. (20.9% X 760 mm Hg.), and
carbon dioxide is 0.3 mm Hg (0.04% X 760 mm Hg.).
Comparing the partial pressures of air
in the alveolus to the partial pressures of
gases in the alveolar capillaries,
– oxygen diffuses into the blood because the
alveolar partial pressure of oxygen (PO2 is
about 104 mm Hg.) is greater than the blood’s
oxygen partial pressure (about 40 mm Hg.).
– Carbon dioxide diffuses out of the blood
capillaries because its blood partial pressure
(PCO2 is about 45 mm Hg.) is greater than
the carbon dioxide partial pressure (about 40
mm Hg.) of the alveoli.
Partial pressures at the Tissues
•
Comparing the partial pressures of air in the
tissue capillaries to the partial pressures of
gases in the tissues,
– oxygen diffuses into the tissues because the partial
pressure of oxygen (about 104 mm Hg.) is greater
than the tissue’s oxygen partial pressure (less than 40
mm Hg.).
– Carbon dioxide diffuses out of the tissues because its
partial pressure (more than 45 mm Hg.) is greater
than the tissue’s blood capillaries carbon dioxide
partial pressure (about 40 mm Hg.).
Figure 25.19
Partial pressures at the alveoli.
11
Transport of Respiratory
Gases
Figure 25.20
Partial pressures at the tissue level.
Transport of Respiratory Gases
Oxygen Transport
– Henry’s law takes into account the diffusion of gases
into water. Henry’s law states that for a mixture of
gases, more of each gas will diffuse into water as the
partial pressure of the individual gas increases.
– However, how much of the gas diffuses into the water
is not just a function of the partial pressure of the gas,
as the solubility of the gas in water is another
important factor. Comparing the solubilities in water of
the three major gases of atmospheric air, carbon
dioxide is the most soluble, oxygen is much less
soluble, and nitrogen is practically insoluble.
• Oxygen transport by two methods,
– (1) dissolved in plasma, and
– (2) combined with hemoglobin.
• Oxygen is mostly transported by the combination
of oxygen with the heme units (binds with Fe++)
of hemoglobin, forming oxyhemoglobin. About
98.5% of the body’s oxygen is carried as
oxyhemoglobin, with the remaining, about 1.5%,
being dissolved in plasma.
Carbon Dioxide Transport
•
Carbon dioxide transport by three methods,
– (1) dissolved in plasma,
– (2) combined with hemoglobin, and
– (3) bound in bicarbonate ions.
Figure 25.21
The association and dissociation of hemoglobin with oxygen
forming oxyhemoglobin (HbO2) and deoxyhemoglobin (HHb), respectively.
• About 7% of the carbon dioxide is transported
dissolved in the plasma. About 23% is transported
combined with the protein portion of the
hemoglobin molecule as carbaminohemoglobin.
About 70% of the carbon dioxide is transported
combined into bicarbonate ions.
12
Carbon dioxide and Oxygen
Transport at the Tissues
Figure 25.22
The reversible reaction showing the formation and dissociation of carbon
dioxide from a bicarbonate ion.
• Carbon dioxide diffuses into red blood cells
where the enzyme carbonic anhydrase speeds
the reaction between carbon dioxide and water
and forms carbonic acid.
• Carbonic acid dissociates into hydrogen ions
and bicarbonate ions. The bicarbonate ions
diffuse out of the red blood cells into the plasma
and are transported to the lungs. The hydrogen
ions bind to hemoglobin, which has released its
oxygen for the oxidation of fuel molecules, and
forms deoxyhemoglobin
Carbon dioxide and Oxygen
Transport at the Lungs
• . At the lungs, bicarbonate ions diffuse into the
RBCs, where they combine with hydrogen ions
released from deoxyhemoglobin, and form
carbonic acid. In the enzyme mediated reaction,
carbonic acid is split into carbon dioxide and
water. Carbon dioxide diffuses into the alveoli for
removal from the lungs.
• As deoxyhemoglobin releases its hydrogen ions,
oxygen diffuses into the RBCs and binds to
hemoglobin and forms oxyhemoglobin. Ninety
eight percent of oxygen is transported to the
tissues as oxyhemoglobin, and the remaining
1.5% is transported dissolved in the plasma.
Figure 25.23
Illustration of the transport of carbon dioxide and oxygen at the tissue level.
Mechanisms Controlling
Respiration
Figure 25.24
Illustration of the transport of carbon dioxide and oxygen at the lungs.
13
Mechanisms Controlling
Respiration
•
Neural control of respiration is by
respiratory centers in the medulla
oblongata and pons of the brain stem. The
medulla oblongata contains two
respiratory centers, the dorsal respiratory
group (DRG) and the ventral respiratory
group (VRG).
Mechanisms Controlling
Respiration
• The respiratory center is mostly controlled by input from
chemoreceptors, proprioceptors, and emotional
(hypothalamic) and voluntary (cortical) centers of the
brain.
• Chemoreceptors are sensitive to changes in carbon
dioxide and oxygen concentrations, and pH.
– The peripheral chemoreceptors, includes the aortic bodies (in
the aortic arch) and the carotid bodies (in the carotid sinuses).
The peripheral chemoreceptors mostly monitor blood oxygen
(PO2).
– The central chemoreceptors are located in areas of the brain
stem associated with the medulla and the pons. The central
chemoreceptors are mostly sensitive to changes in pH and
carbon dioxide concentration (PCO2).
Mechanisms Controlling
Respiration
– Proprioceptors are receptors that monitor motion and
are especially abundant in muscles, joints, tendons,
and the inner ear. Increased stimulation of
proprioceptors stimulates the respiratory center to
increase rate of respiration. Brain centers such as
those of the hypothalamus can trigger
hyperventilation (anxiety attacks), and cortical
(voluntary) control allows limited alterations in
breathing rates.
Central chemoreceptors
(continued)
• Hydrogen ions target the central chemoreceptors, which
stimulate the respiratory center to increase the rate of
respiration. The increased rate of respiration increases
the pH (becomes more basic) as more carbon dioxide is
removed from the blood. Carbon dioxide is derived from
carbonic acid. Thus, removing more carbon dioxide,
removes more carbonic acid (hydrogen ions), and
increases pH back to normal levels.
Central chemoreceptors
•
The central chemoreceptors are the
dominate chemoreceptors and respond mostly
to changes in pH of cerebrospinal fluid (CSF).
– An increase of carbon dioxide results in a decreased
pH of cerebrospinal fluid. An increase in carbon
dioxide usually results from increased aerobic
metabolism (oxidation of fuel molecules) or from
hypercapnia, an increase of carbon dioxide caused by
decreased and shallow breathing called
hypoventilation.
– A decreased pH (becomes more acidic) results
because carbon dioxide combines with water and
produces carbonic acid, which dissociates into
hydrogen ions and bicarbonate ions.
Hypocapnia
• a lower than normal concentration of carbon dioxide in
the blood (or CSF) is usually caused by hyperventilation.
Hyperventilation results in a increase of blood pH
(becomes more basic) as increased carbon dioxide
(thus, carbonic acid) is removed from the blood.
• Hypocapnia and increased blood pH is reversed by
hypoventilation, which results in conservation of carbon
dioxide (thus, carbonic acid).
• Medically, reversal of hypocapnia resulting from
hyperventilation (increases pH) caused by anxiety, is
often by conservation of carbon dioxide (decreases pH)
by rebreathing into a bag .
14