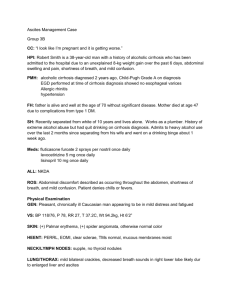
Chronic Liver Disease
advertisement

Chronic Liver Disease Burden • • • • Markedly decreased life expectancy 12th leading cause of death in US 25,000 deaths annually in US High morbidity and mortality due to complications Autoimmune hepatitis Alcoholic liver disease Chronic hepatitis C Primary sclerosing cholangitis Chronic hepatitis B Alpha1-antitrypsin deficiency Wilson’s disease Primary biliary cirrhosis Hereditary hemochromatosis Hepatic Fibrosis Cirrhosis Hepatic fibrosis • Fibrosis is a wound healing response in which damaged regions are encapsulated by an extracellular matrix or scar • Develops in almost all patients with chronic liver injury Cirrhosis • Late stage of progressive hepatic fibrosis • Generally irreversible in advanced stages LFT’s • LFT is a misleading term – Does not reflect how well the liver is functioning – Abnormal values can be caused by non-hepatic diseases LFT’s • Enzyme tests: AST, ALT, Alk Phos and GGT • Hepatic Function: Albumin and PT and Indirect bilirubin • Hepatic transport ability (biliary system): Direct Bilirubin Patterns • Disproportionate elevation of transaminases seen with hepatocellular processes • Disproportionate elevation of Alk Phos seen in cholestatic process • Serum Bilirubin can be elevated in both processes, so need to look at direct vs indirect bilirubin to differentiate Patterns • Low albumin suggests chronic process • Normal albumin suggests acute process • Elevated PT/INR is either Vit K deficiency (due to malabsorption of Vit K) or significant hepatocellular dysfunction (inability to make coagulation factors) • Failure of parenteral Vit K to correct PT indicates significant hepatocellular dysfunction (inability to make coagulation factors). • Patients who lack an apparent cause for cirrhosis should be questioned about lifetime body weight because nonalcoholic steatohepatitis (NASH) has been concluded to be causative in many patients. •Ascites • What do we do when a patient presents with ascites for the first time? • The cause of new ascites should be evaluated by doing a paracentesis. • What does a bloody ascitic fluid suggest? • Tumor • What does a cloudy ascitic fluid suggest? • Infection • What does a milky ascitic fluid suggest? • Lymphatic obstruction • Approximately 1,500cc of fluid must be present in the abdomen before flank dullness is detected on percussion. • The fluid wave is not a useful sign but shifting dullness is. • What is the most common cause of ascites in United States? • 85% of patients with ascites in the United States have cirrhosis • What are the tests that we order on the ascites fluid obtained by paracentesis? • IF uncomplicated cirrhosis ascites is suspected, only cell count and differential, albumin, and total protein concentration are performed on the initial specimen. • If ascitic fluid infection is suspected (fever, abdominal pain, elevated cell count or unexplained encephalopathy), bacterial culture in blood culture bottles should be performed. • What can we do to determine the cause of ascites after the ascitic fluid labs are back? Serum-to ascites albumin gradient (SAAG) • SAAG= (serum albumin)-(ascitic fluid albumin) • SAAG > 1.1 indicates portal HTN • SAAG < 1.1 indicates pt does not have portal HTN • - SAAG >1.1 (portal HTN): Cirrhosis Right heart failure Fulminant liver failure (which also includes “massive hepatic metastasis”) - Budd-Chiari syndrome - myxedema • - SAAG<1.1: TB peritonitis Nephrotic syndrome Pancreatitis Peritoneal carcinomatosis • Elevated ascites protein level >=2.5 is seen in all cases of SAAG<1.1 but also in right heart failure. • Ascites PMN count >250 is infection until proven otherwise. - Do bacterial culture in “blood culture bottles” - Is considered to be spontaneous bacterial peritonitis (SBP) if there is no evidence of intra-abdominal, surgical treatable source of infection (secondary bacterial peritonitis). • Most of the bacterial cultures of ascitic fluids with PMN>250 will grow bacteria if: 1) The fluid is cultured in two blood culture bottles 2) There has been no prior antibiotic treatment and 3) There is no other explanation for an elevated PMN count (e.g. hemorrhagic ascites, peritoneal carcinomatosis, pancreatitis, or peritoneal TB). • Patients who meet the criteria explained on the previous slide but have negative cultures have been labeled with diagnosis of “culturenegative neutrocytic ascites and should be treated as if they have SBP due to similar mortality as SBP if not treated as such. Diagnosis of SBP • Definition: ascitic fluid infection w/o intraabdominal source of infection • Positive ascitic fluid culture and/or PMN>250 • Consider secondary bacterial peritonitis if at least two of the following: – TP >1.0 – Glucose <50 – LDH > upper limit for serum AND multiple organisms growing on gram stain or culture. AND PMN >250 (sometimes in thousands). Antibiotic choice • Need to cover gut flora as well as Strep and Staph • 3rd generation cephalosporin such as cefotaxime 2g IV q8hrs • Treat for 5 days and reassess patient – If has had good response, d/c antibiotics – If still has fever or abd pain, re-tap • PMN <250, stop antibiotics • PMN > pre-treatment level, look for surgical cause • PMN >250 but < pre-treatment level, give 48 hrs antibiotocs and repeat tap SBP Prophylaxis • Indicated for patients with h/o SBP or variceal bleed • Proven to decrease mortality, to prevent bacterial infections, and to be cost effective SBP Prophylaxis Regimens • If h/o SBP, Norfloxacin 400 mg qweek or Bactrim DS qday • If recent variceal bleed, Norfloxacin 400 mg BID or Bactrim DS BID for 7 days Treatment of ascites of liver disease • Goal is to minimize edema and ascites w/o intravascular volume depletion • No evidence that treatment of ascites improves survival, but pt’s feel better • Treat underlying disorder (eg: Alcohol cessation for alcoholic cirrhosis) • Avoid NSAID’s • Limit Na to 2g/day Treatment of ascites of liver disease (continued) • It is Na restriction and not fluid restriction that results in weight loss • Fluid restriction is not necessary in treating most patients with cirrhosis or ascites • Do not attempt to correct the chronic hyponatremia (which is seen often in cirrhotic patients with ascites) unless <120-125 since attempts to rapidly correct hyponatremia with saline can lead to more complications than the hyponatremia itself. Treatment of ascites of liver disease (continued) • Start with combination of spironolactone and furosemide (100 mg and 40mg) or spironolactone alone • Max required doses: spironolactone 400mg/d and furosemide 160 mg/d • If using combination of spironolactone and furosemide, keep spironolactone to furosemide ratio at 100mg/40mg • Required wt loss is 300-500g/day without massive edema and 800-1000g/day or more with massive edema • Oral furosemide is preferred over iv furosemide. Treatment of ascites of liver disease (continued) • Do fluid restriction if sodium <120. • Any of the following should lead to cessation of diuretics: - Encephalopathy - Serum NA <120 despite fluid restriction - Serum creatinine >2.0. Treatment of large volume ascites • Treatment of choice is large volume paracentesis: - Faster, more effective and fewer adverse effects than diuresis - Diuretics should be given as maintenance therapy to prevent recurrence Refractory Ascites in liver disease • <10% of ascites • Defined as fluid overload that: 1) Is unresponsive to Na-restricted diet and high-dose diuretic treatment (400mg/day of spironolactone and 160mg/day of furosemide) OR 2) Recurs rapidly after therapeutic paracentesis. Treatment of refractory ascites in liver disease • Options: 1) Serial therapeutic paracentesis 2) Liver transplantation 3) Transjugular intrahepatic portasystemic stent-shunt (TIPS) 4) Peritoneovenous shunt (rarely done) • Referal for liver transplant should not be delayed. Complications of cirrhosis • • • • • • • Variceal hemorrhage Ascites Spontaneous bacterial peritonitis Hepatorenal syndrome Hepatic encephalopahty Hepatopulmonary syndrome Hepatocellular carcinoma • All patients with chronic liver disease should be checked for hepatitis viral panel, especially for hepatits B and C. • Vaccination should be given for hepatitis A and B vaccination if they are negative for these types of hepatitis. • The liver is commonly imaged (usually with Ultrasound) in a patient with cirrhosis with or without ascites. Why? • - To screen for: Hepatocellular carcinoma Portal vein thrombosis Hepatic vein thrombosis Case • 55 yo man with h/o heavy ETOH use presents with abdominal swelling and pain • What other questions would you ask the patient? • What are you looking for on your exam? Case • • • • • • • AST 150, ALT 73, alk phos 153, GGT 320 Bilirubin 4.3, Indirect bilirubin 3.1 TP 8.3 Albumin 2.2 INR 1.9 WBC 2.2, H/H 11/33. Plt 78K Na 130 What would you do first in the evaluation of this patient?? Paracentesis • What information do you get from peritoneal fluid analysis? • What studies do you want to perform on the ascites fluid? Ascitic fluid • • • • • Cloudy fluid Albumin 0.5 TP 0.7 Cell count: 425 WBC, 90% PMN’s Gram stain: many PMN’s, no bacteria How do you interpret the results from your tap? How will you treat the ascites?