Antiemetic prophylaxis: Pharmacology and therapeutics
advertisement

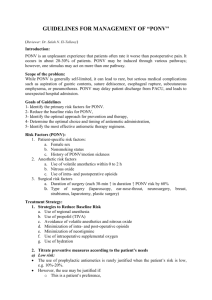
AANA Journal Course Update for nurse anesthetists 1 *6 CE Credits Antiemetic prophylaxis: Pharmacology and therapeutics Carol L. Norred, CRNA, MHS Denver, Colorado Postoperative nausea and vomiting (PONV), a common problem with complex causes, may result in substantial complications. This Journal course discusses the pathogenesis of PONV and reviews antiemetic pharmacology. Corticosteroids, gastrointestinal prokinetics, neuroleptic butyrophenones, phenothiazines, and serotonin receptor antagonists may be prescribed alone or in combination. State-of-the-art anesthetic techniques for prevention of PONV are described. Multimodal therapy with combined low-dose antiemetics affecting multiple receptors is suggested to prevent PONV in high-risk patients such as nonsmokers, females with a previous history of nausea, and patients with high postoperative narcotic requirements. Objectives current pharmacology for antiemetic prophylaxis is followed by a description of therapeutic anesthetic techniques to minimize PONV. At the completion of this course, the reader should be able to: 1. Describe the pathophysiological factors that may precipitate postoperative nausea and vomiting (PONV). 2. Compare and contrast the mechanisms of action of and indications for corticosteroids, gastrointestinal prokinetics, neuroleptic butyrophenones, phenothiazines, and serotonin receptor antagonists for prevention and treatment of PONV. 3. Examine the contraindications, side effects, and drug interactions of these antiemetic drugs. 4. Identify patients, procedures, and anesthetic techniques that may contribute to an increased risk of PONV. 5. Formulate an appropriate anesthetic plan to minimize PONV in high-risk patients. Introduction This Journal course overviews the pathogenesis and physiological mechanisms of postoperative nausea and vomiting (PONV). In addition, an extensive review of Key words: Antiemetics, nausea, vomiting. Pathogenesis and physiological mechanisms of nausea and vomiting Nausea and vomiting pose a substantial postoperative problem that can result in corporeal complications, such as aspiration, wound disruption, impaired healing, and increased surgical bleeding. In addition, intractable nausea and vomiting can minimize patient satisfaction, delay patient discharge, and increase hospital costs.1,2(pp14-15),3(p1395) Several studies report an incidence of PONV as high as 60% to 70% after high-risk procedures, but generally the incidence is around 30%.1 The pathogenesis of PONV is multifactorial. Preoperative (Table 1), intraoperative (Table 2), and postoperative factors (Table 3) may have a role. Physiologically, autonomic stimulation due to nausea and vomiting results in salivation, cutaneous vasoconstriction, tachycardia, mydriasis, inhibition of gastric parietal cell secretion of acid, and altered gastric motility. Triggers of nausea and vomiting may occur from multiple sites such as the pharynx, ear, gut, and brain. An emetic reflex may be elicited from pharyngeal stimula- * The American Association of Nurse Anesthetists is accredited as a provider of continuing education in nursing by the American Nurses Credentialing Center Commission on Accreditation. The AANA Journal course will consist of 6 successive articles, each with objectives for the reader and sources for additional reading. At the conclusion of the 6-part series, a final examination will be printed in the AANA Journal. Successful completion will yield the participant 6 CE credits (6 contact hours), code number: 25468, expiration date: July 31, 2004. AANA Journal/April 2003/Vol. 71, No. 2 133 Table 1. Preoperative factors affecting postoperative nausea and vomiting (PONV)1-6 Factor Effects Age Children and adolescents more likely to have PONV; for people older than 50 y, little association between age and PONV Sex Women more likely, affected by gonadotropin and estrogen; PONV likely during menstrual cycle History Likelihood increased if previous PONV or motion sickness Smoking Decreases risk of PONV Anxiety With high anxiety, increased PONV due to catecholamine release; air swallowing by anxious patients increases gastric volume Obesity Positive correlation due to accumulation of fat-soluble anesthetics; obesity linked with large gastric volume, increased esophageal reflux, increased gallbladder and gastrointestinal disease Oral intake Decreased gastric motility after excessive preoperative intake of fatty foods; vomiting during induction or emergence stimulated by full stomach; history of heavy alcohol intake associated with less nausea Table 2. Intraoperative factors affecting postoperative nausea and vomiting (PONV)1-6 Factor Effects Surgery type Higher PONV incidence in the following types of surgery or anatomic areas: intra-abdominal, craniotomy, gynecological, laparoscopic, orthopedic, to treat strabismus or ear-nose-throat disorders, plastic, breast augmentation, or orthopedic shoulder surgery Duration of surgery Increased chance of PONV in longer procedures Anesthetic technique Greater likelihood with general anesthesia; no effect of gastric emptying during general anesthesia on the incidence of PONV; spinal associated with less PONV than general anesthesia; peripheral regional anesthesia least emetogenic Anesthetic drugs Occurrence of PONV increased with balanced anesthesia combined with opioids; each drug is very emetogenic: morphine, meperidine, fentanyl, etomidate, ketamine, thiopental, nitrous oxide, and neostigmine Table 3. Postoperative factors affecting postoperative nausea and vomiting (PONV)1-6 Factor Effects Pain Nausea substantially reduced by adequate pain relief Opioids Increases PONV by causing direct stimulation of chemoreceptor trigger zone Movement May induce PONV through a vestibular component Orthostatic hypotension or dehydration May contribute to PONV Hypoglycemia May contribute to PONV from prolonged fasting Hypoxemia May contribute to PONV Oral intake Premature intake of food or fluid may contribute to PONV tion. The labyrinthine or vestibular apparatus and auricular branch of the tympanum of the ear may detect motion stimuli from histamine or acetylcholine receptors. Mechanoreceptors of the bladder, gallbladder, or uterus may detect overdistention and disordered 134 AANA Journal/April 2003/Vol. 71, No. 2 gastric motility due to disease or surgical trauma. Hepatic portal vein detectors sense chemical stimuli in the venous drainage of the gut. Gastric and duodenal chemoreceptors detect irritation from toxins such as serotonin (also known as 5-HT).2(pp16-23),7(pp316-317) Table 4. Antiemetic drugs1-8 Class Generic name Trade name Corticosteroids Dexamethasone Decadron 4-10 mg IV on induction Butyrophenones Droperidol Inapsine 0.625-1.25 mg IV preoperatively or treatment Gastrointestinal prokinetics Metoclopramide Reglan 10-20 mg IV or PO preoperatively Serotonin antagonists Ondansetron Zofran 4 or 8 mg IV before induction or as treatment; 8 mg PO 1-2 h preoperatively Dolasetron Anzemet 12.5 mg IV 15 min before emergence or as treatment; 100 mg PO 1-2 h preoperatively Granisetron Kytril 1 mg IV on induction or as treatment Promethazine Phenergan 12.5-25 mg IV or rectal every 4-6 h Prochlorperazine Compazine 5-25 mg PO, rectal, or IV every 4-6 h Phenothiazines Dose and timing* * IV indicates intravenous; PO, by mouth. From the vagus nerve of the gut, transmitted signals reach the histamine, cholinergic, or enkephalin receptors in the nucleus tractus solitarius or other centers in the area postrema and area subpostrema. The chemoreceptor trigger zone (CTZ) located in the area postrema on the floor of the fourth ventricle of the brain may identify absorbed toxins or disturbances such as hypotension or metabolic acid-base changes. The higher brain centers in the cortex and limbic system may be affected by emotions, smells, sights, or thoughts. Afferent stimuli detect the need to vomit and coordinate the response in the vomiting center located in lateral reticular formation of the brainstem close to the fourth ventricle. This area is rich in receptors that have an important role in the transmission of impulses to emetic centers such as serotonin, opioid, histamine, and muscarinic and dopamine receptors. Other dopamine receptors in the nucleus tractus solitarius and CTZ may be implicated in the vomiting reflex and are involved in the control of gastric motility.2(pp16-23),7(pp316-317) Thus, many physiological and pathological foci contribute to the cause of PONV. The clinician can use this information in the administration of the varied pharmacological treatments for prophylaxis of this complex and recalcitrant problem. Literature review: Antiemetic pharmacology The purpose of this course is to discuss the clinically relevant pharmacology of common antiemetic drugs such as corticosteroids, gastrointestinal prokinetics, neuroleptic butyrophenones, phenothiazines, and serotonin receptor antagonists. Table 4 presents the doses and trade names of pharmaceuticals in each of these antiemetic classes. • Corticosteroids. Corticosteroids inhibit prostaglandin synthesis and prevent the inflammatory release of serotonin in the gut, or they sensitize the antiemetic pharmacotherapy receptors. Dexamethasone has been found to enhance the effects of other antiemetic drugs. Alone or combined with serotonin receptor antagonists, dexamethasone is especially useful for late PONV efficacy.9 For example, in a randomized study of Taiwanese patients undergoing laparoscopic cholecystectomy, 5 mg of prophylactic intravenous (IV) dexamethasone was as effective as 2 mg of IV tropisetron, and significantly more effective than placebo to reduce the incidence of PONV (P < .01).10 A study of patients who had undergone hysterectomy and were treated for nausea due to epidural morphine found that 5 mg of IV dexamethasone effectively reduced nausea and vomiting (P < .01) and reduced the use of rescue antiemetics (P < .05), but 5 mg of IV tropisetron was not significantly more effective.11 In a randomized, placebo-controlled, doubleblind trial, researchers found that 4 mg of IV dexamethasone combined with 12.5 mg of IV dolasetron, administered just after induction for laparoscopic cholecystectomy, was associated with significantly shorter day surgery stay, more rapid discharge, improved patient satisfaction, and improved quality of recovery, as well as decreased PONV after discharge (P < .05). However, no difference in early nausea and vomiting was noted compared with patients who received only 12.5 mg of IV dolasetron. Administration of dexamethasone at induction may improve antiemetic efficacy.12 Long-term use or large doses of glucocorticoids may cause considerable adverse effects,13(pp420-422) but studies do not suggest the occurrence of toxic effects with low doses.9-12 However, glucocorticoids may exacerbate AANA Journal/April 2003/Vol. 71, No. 2 135 hypokalemia, metabolic acidosis, edema, myopathy, peptic ulcer, infections, psychosis, diabetes, or osteoporosis.13(pp420-422) Phenytoin, phenobarbital, ephedrine, and rifampin speed the clearance of dexamethasone. Concomitant use of diuretics with glucocorticoids may result in hypokalemia.14(p2082) • Gastrointestinal prokinetics. Gastrointestinal prokinetics are often administered preoperatively. Antiemetic gastrointestinal prokinetic drugs classified as benzamides include metoclopramide, domperidone, and cisapride.13(pp447-450) However, cisapride does not prevent postoperative vomiting in children and may intensify the problem.15 Metoclopramide does not alter gastric hydrogen ion secretion or pH, but speeds gastric emptying and shortens the small intestinal transit time of ingested substances by cholinergic stimulation of the postganglionic nerves of the gastrointestinal tract. It increases smooth muscle tension of the lower esophagus and stomach, increases gastrointestinal motility, causes relaxation of the pylorus and duodenum, and increases prolactin and aldosterone secretion. It centrally antagonizes dopamine receptors of the CTZ. In high doses, this drug acts as a serotonin receptor antagonist and stimulates cholinergic effects on the gastrointestinal smooth muscle.13(pp447-448) However, a systematic review found that 10 mg of IV metoclopramide was no more effective than placebo for prevention of PONV in adults and children.16 While the antiemetic efficacy is controversial, combined with an H2 receptor antagonist, metoclopramide effectively reduces both gastric pH and volume.17(p559) Metoclopramide is indicated to decrease preoperative gastric volume and to treat heartburn, gastrointestinal reflux, and gastroparesis. Preoperative metoclopramide may be beneficial for patients who have fasted for an insufficient time before surgery or have a full stomach or after trauma. In addition, maternity patients or patients who are obese, have diabetes with autonomic neuropathy, or are at risk for aspiration pneumonia also may benefit from the administration of metoclopramide.9(p448),17(p559) Although it is prescribed frequently, metoclopramide should be used cautiously. Metoclopramide may cause increased intracranial pressure in head-injured patients.18 Metoclopramide is contraindicated in patients with breast cancer, intestinal obstruction, or pheochromocytoma, and for patients taking medication for Parkinson disease, seizure disorders, or depression. Pediatric and geriatric patients and patients with renal failure or insufficiency may be more prone to adverse effects; the dose should be decreased in these populations. While it does not cause substantial sedation, metoclopramide may cause intestinal cramping. It 136 AANA Journal/April 2003/Vol. 71, No. 2 may cause analgesia in patients with gastrointestinal spasm, biliary or renal colic, uterine cramping, or prostaglandin-induced pregnancy termination. Metoclopramide is rarely linked with hypotension, dysrhythmia, or extrapyramidal side effects such as dysphoria or agitation.4(p246),13(pp448-450) Interactions may occur with other antiemetics or anesthetic drugs. Due to potential extrapyramidal effects, metoclopramide should not be administered with phenothiazines or butyrophenones such as droperidol. Metoclopramide has been linked with dysrhythmia when combined with ondansetron. It may decrease the induction dose of thiopental and also may increase the sedative effect of central nervous system depressants.4(p246),13(pp448450) Anticholinergics4(p246),13(pp448) and opioids4(p449) may offset the beneficial effects of metoclopramide. Metoclopramide may inhibit plasma cholinesterase and the metabolism of drugs such as succinylcholine or ester local anesthetics.13(p450) • Neuroleptic drugs. Also used to treat psychoses, neuroleptic drugs are potent sedatives and antiemetics. Neuroleptic butyrophenones act peripherally on the gastrointestinal tract and block dopamine receptors in the CTZ.13(p373) Although droperidol does not affect histamine receptors and is not effective for motion sickness,13(p376) it inhibits the activation of g -aminobutyric acid, serotonin, norepinephrine, and neuronal nicotinic acetylcholine receptors,19 and it exhibits mild peripheral a -adrenoreceptor antagonism.4(p174),13(p374) Because droperidol does not alter carotid body hypoxic drive, it also is indicated for the sedation of patients with chronic obstructive pulmonary disease and to decrease blood pressure.13(pp373-374) Several studies illustrate the antiemetic efficacy of droperidol. In a randomized, double-blind study of adult general surgery patients, when given 30 minutes before emergence from general anesthesia, low dose 0.625 mg of IV droperidol, was significantly more effective than placebo (P < .001) and as effective as 12.5 mg of IV promethazine and as effective as 4 mg of IV ondansetron, without significant differences in adverse events.20 A meta-analysis found the efficacy and safety for the prevention of PONV to be similar with droperidol (pooled odds ratio [OR], 0.68; 95% confidence interval [CI], 0.54-0.85; P < .001) and ondansetron (pooled OR, 0.43; 95% CI, 0.31-0.61; P < .001), with both drugs being more effective than metoclopramide.21 Similar patient satisfaction and rates of adverse effects were found in adult outpatients (pooled OR, 0.87; P = .45).21 Still, a multicenter, randomized, double-blind, placebo-controlled study found that prophylactic 1.25 mg of IV droperidol was more efficacious than 0.625 mg IV, less costly than 4 mg of IV ondansetron (P = .001), and associated with similar patient satisfaction (P < .05).22 Although droperidol is less expensive,22 it may cause clinically significant adverse effects. High-dose droperidol may be more effective as an antiemetic, but doses greater than 50 to 75 µg/kg may cause extrapyramidal effects.23(p864) When administered preoperatively, droperidol may cause dysphoria and agitation without decreasing anxiety. Sedation without amnesia, lethargy, and dry mouth may occur. Treatable with dyphenhydramine,13(p373) extrapyramidal reactions are more common in middle-aged women and children.24(p51S) Due to a -adrenergic blockade, droperidol may cause hypotension due to vasodilation, but it does not alter myocardial contractility or depress respirations. Droperidol decreases cerebral blood flow and intracranial pressure, which may be an adverse effect for elderly patients but does not affect cerebral metabolic oxygen consumption. Droperidol also is contraindicated in patients with Parkinson disease or pheochromocytoma. The elimination of droperidol is prolonged in patients with diminished hepatic blood flow or liver disease.13(pp373-374) Before a recent warning from the US Food and Drug Administration about the potential for Q-T interval prolongation and torsades de pointes, droperidol commonly was administered as a low-cost antiemetic.25 Drugs that may interact with droperidol by prolonging the Q-T interval include class Ia antiarrhythmics (disopyramide, procainamide, and quinidine), class III antiarrhythmics (amiodarone, dofetilide, ibutilide, and sotalol), antihistamines (terfenadine and astemizole), phenothiazines, tricyclic antidepressants, corticosteroids, chloral hydrate, cisapride, clarithromycin, erythromycin, thiazide diuretics, tamoxifen,26(pp277279,295-296) sevoflurane,4(p145) and dolasetron.27 In addition, droperidol prolongs the duration of action of fentanyl,13(p375) antagonizes the action of levodopa, and interferes with dopamine’s renal effects. Droperidol also may minimize ketamine’s cardiovascular effects or precipitate rebound hypertension with clonidine.4(p175) • Phenothiazines. Similar to butyrophenones, phenothiazine antiemetics block the CTZ dopaminergic receptors and a -adrenergic receptors.7(p318) Phenothiazines also have anti–motion-sickness, antipruritic, and anxiolytic effects because they antagonize H1 and cholinergic receptors.28(p273) Phenothiazine agents include prochlorperazine and promethazine. 7(p318),13(p370) Promethazine is indicated for the treatment of allergic blood reaction, anaphylaxis, sedation, labor, motion sickness, and PONV and is indicated as an adjunct to analgesics.14(p3553) Phenothiazines are potent sedatives and may delay discharge after day surgery.7(p318) They also may cause blurred vision, dizziness, tremors, nervousness, and extrapyramidal effects. Phenothiazines have minimal effects on the cardiovascular system except potential for hypotension or a prolonged Q-T interval. These drugs may lower the seizure threshold and should be used cautiously in patients with altered cognition, sleep apnea, bone marrow depression, narrow angle glaucoma, prostatic hypertrophy, peptic ulcer, or duodenal or bladder obstruction.13(pp371-372),14(pp15051506,3553-3558) Extrapyramidal effects of prochlorperazine may be exacerbated with monoamine oxidase inhibitor drugs.14(p1506) Like many other antiemetics, phenothiazines augment the sedative effects of central nervous system depressants.13(p372) • Selective serotonin receptor antagonists. Antiemetic serotonin receptor blockers are expensive, but their use is established because they have few side effects such as sedation and respiratory depression and few extrapyramidal effects because they do not affect histamine, dopamine, or cholinergic receptors.7(p319),13(p406) Seven types of serotonin receptors exist; they are found in the central and peripheral nervous systems, smooth muscle, and platelets. Serotonin receptor antagonists block serotonin receptors peripherally in the gastrointestinal tract and centrally in the medulla and area postrema where the vomiting center, nucleus tractus solitarius, and CTZ are located.29 Selective serotonin receptor antagonists include drugs such as ondansetron, dolasetron, and granisetron.1(p1233),2(p78) Selective serotonin receptor antagonists work well to prevent PONV. However, serotonin receptor antagonists do not effectively prevent or treat motion-induced nausea and vomiting.13(p406) Numerous randomized, double-blind studies found that ondansetron and dolasetron were significantly more effective than placebo for prevention of PONV in high-risk groups.5,30 A meta-analysis reported that ondansetron was more effective than droperidol and metoclopramide for preventing PONV in children (pooled OR, 0.49; P = .004).21 However, in a double-blind study of patients undergoing otolaryngologic surgery, 12.5 mg of IV dolasetron administered 30 minutes before emergence was found as effective as 25 mg of IV dolasetron and more cost effective than and similar in efficacy to 4 and 8 mg of IV ondansetron, with no difference in patient satisfaction.31 Metabolism to hydrodolasetron is attributed to the antiemetic effect of dolasetron.5 Serotonin receptor blocker drugs may be associated with a low incidence of headache, diarrhea, light-headedness, warm epigastrium sensations, flushing, and constipation.7(p319),13(p406) But to avoid torsades de pointes arrhythmias, dolasetron should not be administered with drugs that can prolong the Q-T interval. Although it does not significantly alter blood pressure, dolasetron can prolong the P-R and Q-Tc intervals and widen the QRS interval by blocking sodium channels, and it can prolong myocardial depolarization.27 AANA Journal/April 2003/Vol. 71, No. 2 137 Dolasetron and ondansetron do not cause sedative drug interactions,4(p248),7(p319),13(p406) but ondansetron reduces the overall analgesic effect of tramadol.32 A great formulary is available to the clinician for effective management of PONV. To understand the dynamic intricacies of pharmacological treatments, the astute anesthetist also should be cognizant of the impact of anesthetic technique on antiemetic prophylaxis. State-of-the-art anesthetic techniques for PONV prevention Clinicians may debate the best treatment plan for prevention of PONV. No single drug is without inextricable side effects and costs, is completely efficacious for prevention of PONV, or is innocuous. The overall risk of adverse effects may not be different among various drug combinations.33 Arbitrary or global administration of prophylactic antiemetic medications is not recommended. Although PONV is a very unpleasant experience, data suggest little difference in outcomes including time to discharge, unanticipated admission, patient satisfaction, and time to return to normal activities when nausea was treated symptomatically rather than prophylactically.34 Yet, in identified at-risk patients undergoing emetogenic procedures, techniques to prevent PONV are indicated. Anesthetists are encouraged to minimize administration of anesthetic drugs known to stimulate nausea and strategically administer antiemetics before emergence from general anesthesia if indicated. Multimodal antiemetic therapy, total intravenous anesthesia with propofol, adequate hydration, anxiolytics, effective nonopioid analgesia, supplemental oxygen, and nonpharmacological techniques such as acupuncture, acupressure, and hypnosis may improve efficacy. A treatment algorithm for PONV prophylaxis appropriate for medium- to high-risk patients is given in the Figure.1 Narcotics, especially morphine, are notorious for precipitating nausea and vomiting.7(p317) Surprisingly, a randomized, double-blind study of outpatients found no statistical difference of PONV in patients given 0.25 mg of IV nalbuphine, 20 µg/kg of IV alfentanil, 2 µg/kg of IV fentanyl, or placebo for induction of general anesthesia.35 But a subsequent randomized, double-blind study of outpatients found that 150 µg/mL of alfentanil caused less nausea and vomiting than 50 µg/mL of fentanyl and 5 µg/mL of sufentanil (12%, 34%, and 35%, respectively; P < .005) when administered in equipotent concentrations for general anesthesia.36 Cyclooxygenase inhibitors and local anesthetics may provide nonopioid analgesia without increasing the risk of PONV.1 Neostigmine may be implicated as a cause of nausea and vomiting.13(p230) Yet, a study of ambulatory surgical patients who received 2.5 mg of IV neostigmine and 0.5 mg of IV glycopyrrolate for reversal of rocuronium or mivacurium muscle relaxant showed no association with an increased incidence of nausea. A total of 18% of patients given reversal with neostigmine and glycopy- Figure. Risk factors for postoperative nausea and vomiting (PONV) and guidelines for prophylactic antiemetic therapy1 Patient factors Female sex History of PONV or motion sickness Nonsmoker Postoperative opioid use Mild to moderate risk 20%-40% 1-2 factors present Moderate to high risk 40%-80% 3-4 factors present Any of the following: Droperidol Dexamethasone Scopolamine Serotonin antagonist Droperidol plus Serotonin antagonist or Dexamethasone plus serotonin antagonist 1 (Reproduced with permission from Gan. ) 138 Surgical factors Laparoscopy Laparotomy Plastic surgery Major breast surgery Craniotomy Otolaryngologic procedures Strabismus surgery AANA Journal/April 2003/Vol. 71, No. 2 Very high risk > 80% > 4 factors present Combination antiemetics plus Total intravenous anesthesia with propofol rrolate had nausea vs 15% of patients who did not. Eight percent of patients who were reversed vomited vs 12% of patients who did not receive reversal. Additionally, no difference was noted for the need for antiemetics (13% in both groups) between patients who received neostigmine and patients who did not.37 Nitrous oxide may contribute to PONV by stimulating the CTZ and vomiting center or by stimulating opioid receptors. Nitrous oxide is 35 times more soluble than nitrogen in the blood; consequently, air-filled cavities such as the gut or middle ear may expand due to nitrous oxide absorption, resulting in increased size and pressure and contributing to PONV.4(p138),13(p26) Due to etherizing airway irritation, desflurane was associated with a higher incidence of PONV than isoflurane in a study using a laryngeal mask airway and standardized anesthetics for outpatient arthroscopy.38 In a study of patients undergoing laparoscopic cholecystectomy, although time to awakening was prolonged, a subhynotic dose of propofol (0.5 mg/kg IV) given before emergence more effectively prevented vomiting and the need for rescue antiemetics after sevoflurane than after desflurane anesthesia.39 Total intravenous anesthesia with propofol is more efficacious than ondansetron for preventing PONV.13(p142) Although it is 3 times more expensive, total intravenous anesthesia with propofol and oxygen, compared with isoflurane–nitrous oxide–oxygen anesthesia, reduced the absolute risk of PONV for 72 hours postoperatively by 15% among inpatients (from 61% to 46%; P < .001) and by 18% among outpatients (from 46% to 28%; P < .001).40 In the postanesthesia care unit, a subhypnotic dose of propofol may be given as antiemetic or antipruritic treatment.4(p940),13(p142) Although the specific antiemetic action of propofol is unknown, it is not due to dopaminergic 13(p142) or prokinetic effects. 41 The antiemetic effect of propofol may be related to a decreased serotonin level in the area postrema.1 Due to the multiplicity of triggering factors for PONV, combination therapy may be useful for high-risk patients.1 A randomized, double-blind study of female outpatients undergoing laparoscopic surgery found that multimodal management was associated with a 98% complete response rate and a 0% incidence of vomiting, compared with 7% in the groups receiving prophylaxis with 4 mg of IV ondansetron (P = .07) or placebo (22%; P = .0003). In the multimodal therapy group, 2% required postoperative antiemetic treatment compared with 24% in the ondansetron group (P < .0001) and 41% in the placebo group (P < .0001). Nevertheless, multimodal therapy was not associated with increased patient satisfaction compared with prophylaxis or rescue treatment for PONV.8 Effective preemptive treatment of PONV may enhance the use of combined treat- ment with antiemetics that affect several receptors such as a serotonin antagonist combined with a corticosteroid or a dopamine antagonist.1 Summary Because PONV has multiple causes, prevention has been problematic. Prophylactic antiemetic therapy must be tailored to the level of risk. Anesthetists should inquire about the patient history of postoperative emesis to design a therapeutic plan to minimize noxious stimuli. Anesthetic drugs that are implicated as emetogenic should be avoided when possible. Simple anesthetic techniques such as preventing hypotension and providing adequate hydration, anxiolysis, nonopioid analgesia, and high inspired oxygen may decrease the incidence of PONV not only in identified high-risk patients but also in other surgical patient populations. Antiemetics should be chosen by considering the mechanism of action, indications, contraindications, side effects, and drug interactions that may preclude administration. Lower cost antiemetic drugs may be associated with potent sedative effects that prolong emergence or have potential adverse drug interactions. Sedative drug interactions may occur with gastrointestinal prokinetics, neuroleptic butyrophenones, and phenothiazines. Although they do not augment the sedative effects of anesthetics, serotonin receptor antagonists are costly. Corticosteroids provide increased antiemetic efficacy, but the potential of toxic effects may impede acceptance of corticosteroids as a therapeutic. Consequently, these drugs may be reserved for highrisk patients. Low-dose therapy may minimize adverse and toxic effects of the drugs. A multimodal approach of combined low-dose antiemetic drugs that affect multiple receptors is a logical and effective strategy to provide a more pleasant emergence for at-risk surgical patients by preventing PONV. REFERENCES 1. Gan TJ. Postoperative nausea and vomiting: can it be eliminated? JAMA. 2002;287:1233-1236. 2. Hawthorn J. Understanding and Management of Nausea and Vomiting. Oxford, England: Blackwell Science; 1995. 3. Mecca RS. Postoperative recovery. In: Barash PG, Cullen BF, Stoelting RK, eds. Clinical Anesthesia. 4th ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 2001:1377-1402. 4. Morgan GE, Mikhail MS, Murray MJ. Clinical Anesthesiology. 3rd ed. New York, NY: Lange Medical Books; 2002. 5. Anzemet (dolasetron mesylate). Summary product monograph. Kansas City, Mo: Hoechst Marrion Roussel, Inc; 2001:1-23. 6. Wattwil M, Thorn SE, Lovqvist A, et al. Perioperative gastric emptying is not a predictor of early postoperative nausea and vomiting in patients undergoing laparoscopic cholecystectomy. Anesth Analg. 2002;95:476-479. 7. Harter RL, Christofi FL. Gastrointestinal pharmacology. In: Bovill JG, Howie MB. eds. Clinical Pharmacology for Anesthetists. London, England: WB Saunders; 1999:309-320. 8. Scuderi PE, James RL, Harris L, Mims GR. Multimodal antiemetic AANA Journal/April 2003/Vol. 71, No. 2 139 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 140 management prevents early postoperative vomiting after outpatient laparoscopy. Anesth Analg. 2000;91:1408-1414. Henzi I, Walder B, Tramèr MR. Dexamethasone for the prevention of postoperative nausea and vomiting: a quantitative systematic review. Anesth Analg. 2000;90:186-194. Wang JJ, Ho ST, Uen YH, et al. Small-dose dexamethasone reduces nausea and vomiting after laparoscopic cholecystectomy: a comparison of tropisetron with saline. Anesth Analg. 2002;95:229-232. Wang JJ, Tzeng JI, Ho ST, Chen JY, Chu CC, So EC. The prophylactic effect of tropisetron on epidural morphine–related nausea and vomiting: a comparison of dexamethasone with saline. Anesth Analg. 2002;94:749-753. Coloma M, White PF, Markowitz SD, et al. Dexamethasone in combination with dolasetron for prophylaxis in the ambulatory setting. Anesthesiology. 2002;96:1346-1350. Stoelting RK. Pharmacology and Physiology in Anesthetic Practice. 3rd ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 1999. Physicians’ Desk Reference. 56th ed. Montvale, NJ: Medical Economics; 2002. Cook-Sather SD, Harris KA, Schreiner MS. Cisapride does not prevent postoperative vomiting in children. Anesth Analg. 2002;94:50-54. Henzi I, Walder B, Tramèr MR. Metoclopramide in the prevention of postoperative nausea and vomiting: a quantitative systematic review of randomized, placebo-controlled studies. Br J Anaesth. 1999;83; 761-771. Moyers JR, Vincent CM. Preoperative medication. In: Barash PG, Cullen BF, Stoelting RK, eds. Clinical Anesthesia. 4th ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 2001:551-565. Deehan S, Dobb GJ. Metoclopramide-induced raised intracranial pressure after head injury. J Neurosurg Anesthesiol. 2002;14:157-160. Flood P, Coates KM. Droperidol inhibits GABAA and neuronal nicotinic receptor activation. Anesthesiology. 2002;96:987-995. Kreisler NS, Burkhard F, Spiekermann BF, et al. Small dose droperidol effectively reduces nausea in a general surgical adult patient population. Anesth Analg. 2000;91:1256-1261. Domino KB, Anderson EA, Polissar NL, Posner KL. Comparative efficacy and safety of ondansetron, droperidol, and metoclopramide for preventing postoperative nausea and vomiting: A meta-analysis. Anesth Analg. 1999;88:1370-1379. Hill RP, Lubarsky DA, Phillips-Bute B, et al. Cost-effectiveness of prophylactic antiemetic therapy with ondansetron, droperidol, or placebo. Anesthesiology. 2000;92:958-967. Marley RA. Outpatient anesthesia. In: Naglehout J, Zaglaniczny KL, eds. Nurse Anesthesia. 2nd ed. Philadelphia, Pa: WB Saunders; 2001:848-876. Rowbotham DJ. Current management of postoperative nausea and vomiting. Br J Anaesth. 1992;69(7 suppl 1):46S-59S. US Food and Drug Administration. FDA strengthens warnings for droperidol. FDA Talk Paper T01-62, December 5, 2001. Available at: http://www.fda.gov/bbs/topics/ANSWERS/2001/ANS01123.html. Accessed July 16, 2002. Bauman JL, Dekker Schoen M. Arrhythmias. In: Dipro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey LM, eds. Pharmacotherapy: A Pathophysiologic Approach. 5th ed. New York, NY: McGraw-Hill; 2002:273-304. Benedict CR, Arbogast R, Martin L, Patton L, Morrill V, Hahne W. Single blind study of the effects of intravenous dolasetron mesylate versus ondansetron on electrocardiographic parameters in normal volunteers. J Cardiovasc Pharmacol. 1995;28:53-59. Bovill JG. Histamine and histamine antagonists. In: Bovill JG, Howie AANA Journal/April 2003/Vol. 71, No. 2 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. MB. eds. Clinical Pharmacology for Anesthetists. London, England: WB Saunders; 1999:269-278. Gyermek L. Pharmacology of serotonin as related to anesthesia. J Clin Anesth. 1996;8:402-425. Heiman SA. Zofran injection: adult use in postoperative nausea and vomiting (pivotal trials). Research Triangle, NC: GlaxoWellcome; 2000. Zarate E, Watcha MF, White PF, Klein KW, Sa Rego M, Stewart DG. A comparison of the costs and efficacy of ondansetron versus dolasetron for antiemetic prophylaxis. Anesth Analg. 2000;90:13521358. Arcioni R, della Rocca M, Romano S, Romano R, Pietropaoli P, Gasparetto A. Ondansetron inhibits the analgesic effects of tramadol: a possible 5-HT(3) spinal receptor involvement in acute pain in humans. Anesth Analg. 2002:94;1553-1557. White PF, Watcha MF. Has the use of meta-analysis enhanced our understanding of therapies for postoperative nausea and vomiting? Anesth Analg. 1999;88:1200-1202. Scuderi PE, James RL, Harris L, Mims GR. Antiemetic prophylaxis does not improve outcomes after outpatient surgery when compared to symptomatic treatment. Anesthesiology. 1999;90:360-371. Cepeda MS, Gonzales R, Granados V, Cuervo R, Carr DB. Incidence of nausea and vomiting in outpatients undergoing general anesthesia in relation to selection of intraoperative opioid. J Clin Anesth. 1996;8:324-328. Langevin S, Lessard MR, Trepanier CA, Baribault JP. Alfentanil causes less postoperative nausea and vomiting than equipotent doses of fentanyl or sufentanil in outpatients. Anesthesiology. 1999;91: 1666-1673. Joshi GP, Garg SA, Hailey A, Yu SY. The effects of antagonizing residual neuromuscular blockade by neostigmine and glycopyrrolate on nausea and vomiting after ambulatory surgery. Anesth Analg. 1999;89:628-631. Hough MB, Sweeney B. Postoperative nausea and vomiting in arthroscopic day-case surgery: a comparison between desflurane and isoflurane. Anaesthesia. 1998;53:910-924. Song D, Whitten CW, White PF, Song YU, Zarate E. Antiemetic activity of propofol after sevoflurane and desflurane anesthesia for outpatient laparoscopic cholecystectomy. Anesthesiology. 1998;89:838843. Visser K, Hassink EA, Bonsel GJ, Moen J, Kalkman CJ. Randomized controlled trial of total intravenous anesthesia with propofol versus inhalation anesthesia with isoflurane–nitrous oxide: Postoperative nausea with vomiting and economic analysis. Anesthesiology. 2001;95:616-626. Chassard D, Lansiaux S, Duflo F, et al. Effects of subhypnotic doses of propofol on gastric emptying in volunteers. Anesthesiology. 2002;97:96-101. AUTHOR Carol L. Norred, CRNA, MHS, is a nurse anesthetist researcher and clinical instructor in the Department of Anesthesiology at the University of Colorado Health Sciences Center (UCHSC), Denver, Colo. She also is a doctoral student in the UCSHC School of Nursing. Norred works clinically as a locum tenens nurse anesthetist licensed in Virginia, Kentucky, and Colorado. ACKNOWLEDGMENTS Carol Norred’s institutional predoctoral training is provided through a National Research Service Award funded by the National Center for Complementary and Alternative Medicine and the National Heart, Lung, and Blood Institute (HL T32 07085).