PONV – Risk
Stratification
and Treatment
Jimmy Fu
Importance of PONV
Patient
distress
Morbidity (aspiration, suture tension,
oesophageal rupture, electrolyte
disturbances, dehydration)
Prolonged PACU stay
Unexpected hospital admission/readmission
Physiology
Vomiting Centre: no anatomical site, collection of effector
neurones in medulla, travels down vagus, phrenic nerves, spinal
motor, to abdominal muscles/diaphragm/stomach/gut
VC input from:
Chemoreceptor Trigger Zone: floor of 4th ventricle (functionally
outside BBB)
Vestibular apparatus
Higher centres
Limbic cortex
Peripheral pain pathways
Vagal afferents
CTZ rich in dopamine and serotonin receptors
vestibular apparatus uses ACh to transmit
treatment aimed at afferent supply to VC
Types of agents used in
PONV
1. Dopamine antagonists
Phenothiazine
Chlorpromazine
Thioridazine
Prochlorperazine
less sedation/anticholinergic effects than other
D2 antagonists
more extrapyramidal effects: dystonias and
akathisia
erratic oral bioavailability, marked hepatic firstpass metabolism
1. Dopamine antagonists
Butyrophenones
Droperidol
FDA black box warning: QT prolongation/torsades, based on 10
reported cases. ?validity, nil case-reports in a peer-reviewed
journal of these complications in doses used for PONV
sedation more pronounced, can occur 12hrs after
administration
SE: hyperprolactinaemia, hypotension from alpha-adrenoceptor
blockade
extensively metabolised by liver
Domperidone
no IV formulation secondary to arrhythmias
less likely to have extrapyramidal SE as does not cross BBB
1. Dopamine antagonists
Benzamides
Metoclopramide
D2 antagonist, 5-HT antagonist (some) and
prokinetic for stomach
conflicting studies, some demonstrated
equal efficacy to placebo in PONV
more effective given at end vs induction
variable oral bioavailability (30-90%),
conjugated in liver
2. Anticholinergics
Hyoscine
previously used as pre-med for PONV, sedation
and amnesia
less cardiac effects compared with
atropine/glycopyrrolate
short duration of action, extensively
metabolised by liver, variable oral bioavailability
Atropine: cardiac effects too prominent
Glycopyrrolate: does not cross BBB
3. Antihistamines
Cyclizine
IV/IM painful to inject (pH 3.2)
H1 antagonist, but also anticholinergic
properties
Promethazine
traditional pre-med too
significant anticholinergic/sedative effects
urinary excreted
4. 5-HT3 Antagonists
Ondansetron
very good for chemo/radio or post anaesthetic
nausea (peripheral and central)
Most effective for PONV when given at end of
case
ineffective for motion sickness/dopamine
induced nausea
SE: headache, flushing, constipation, deranged
LFTs, bradycardia (if rapid IV)
conjugated in liver
5. Miscellaneous
Steroids
Dexamethasone
Uncertain mechanism - ?prostaglandin
antagonism ?release of endorphins
More effective at start of anaesthesia
SE of wound infection and adrenal suppression,
but not demonstrated in single bolus dose
Acupuncture – Point P6
Cannabinoids
Use in chemotherapy, not established for PONV
Benzodiazepines
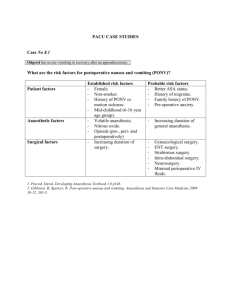
Risk Stratification
Patient factors
Anaesthetic factors
Gender
Non-smoker
History of PONV/motion sickness
Use of volatile agents
Nitrous Oxide
Use of intra/post operative opioids
Surgical factors
Duration of surgery
Type of surgery
(laparoscopy/ENT/neuro/breast/strabismus/laparotomy/plastics)
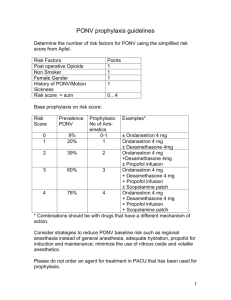
Apfel Score
General anaesthesia (volatiles) with no antiemetic therapy
(age ≥ 18)
Risk Factors
1. Female Gender
2. Non-smoker
3. Post-operative use of opioids
4. Previous PONV or motion sickness
Apfel score
1
10%
2
21%
3
39%
4
79%
Type of Surgery?
Distribution
of risk factors?
Different anaesthetic technique?
Different length of operation?
Operation itself?
Inconclusive,
rating B
conflicting results, evidence
Children
Studies
limited to vomiting
Twice as frequent as adults
Risk increases as child ages! (decrease
after puberty)
No difference in sex before puberty
Stronger correlation with type of surgery
Reducing risk factors
Avoiding
GA (regional)
Avoiding volatiles (propofol)
Intra-operative O2 (FiO2 80%)
Adequate hydration
Avoiding nitrous
Minimising length of operation
Minimising neostigmine
“Consensus Guidelines”
Identify
and stratify risk
Reduce risk factors (previous slide)
Multimodal approach for high risk
Children do better with 5-HT3 antagonists
Rescue therapy should not be same
agent as prophylactic unless > 6hrs since
dose
Dexamethasone works well for prophylaxis
but not rescue
References
Apfel et al: A Simplified Risk Score for Predicting
Postoperative Nausea and Vomiting: Conclusions from
Cross-validations between Two Centers. ANESTHESIOLOGY
1999; 91:693
Gan et al: Consensus Guidelines for Managing
Postoperative Nausea and Vomiting. ANESTHESIA &
ANALGESIA 2003; 97:62-71
Apfel et al: A Factorial Trial of Six Interventions for the
Prevention of Postoperative Nausea and Vomiting. The
New England Journal of Medicine 2004; 350:2441-2451
Henzi et al: Dexamethasone for the Prevention of
Postoperative Nausea and Vomiting: A Quantitative
Systematic Review. ANESTHESIA & ANALGESIA 1999;
90(1):186