Document
advertisement

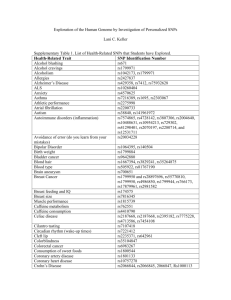
Exenatide for Klinefelter syndrome 125 J. St. Marianna Univ. Vol. 5, pp. 125–129, 2014 Case Report Exenatide Combined with Metformin and Glimepiride Allows Successful Weaning from Insulin in an Obese Diabetic Patient with Klinefelter Syndrome Yoshio Nagai, Yuta Nakamura, Atsushi Hiroishi, Yasuko Abe, Shiko Asai, Hiroyuki Kato, Akio Ohta, and Yasushi Tanaka (Received for Publication: July 14, 2014) Abstract Klinefelter syndrome is the most common numerical sex chromosome disorder. Affected males have an additional X chromosome, resulting in a tall and slender build, hypogonadism, gynecomastia, small testes, sparse body hair, diminished libido, and infertility. It has been reported that patients with Klinefelter syndrome tend to develop diabetes mellitus. Here, we report a 59-year-old man who had Klinefelter syndrome and type 2 diabetes with a body mass index (BMI) of 36.0 kg/m2. Glycemic control was poor despite high-dose insulin therapy (150 units daily). Administration of the GLP-1 analog exenatide together with metformin and glimepiride improved his glycemic control, and allowed weaning from insulin. Interestingly, his weight decreased by 17.5 kg during hospitalization for 39 days, but the patient did not complain of hunger. In conclusion, GLP-1 analog may be a therapeutic option for obese diabetic patients with Klinefelter syndrome. Key words Klinefelter syndrome, Type 2 diabetes mellitus, obesity, insulin resistance, exenatide fects to the incretin hormone glucagon-like peptide 1 (GLP-1). Its actions include glucose-dependent enhancement of insulin secretion, suppression of glucagon secretion, and slowing of gastric emptying. Exenatide also reduces food intake and causes weight loss, thus having an insulin-sensitizing effect7). Here we report on an obese diabetic patient with Klinefelter syndrome, in whom administration of exenatide combined with metformin and glimepiride achieved successful weaning from high-dose insulin therapy at 150 units / day. Introduction Abnormalities of the sex chromosomes can be classified as numerical abnormalities or structural defects. Klinefelter syndrome1) is the most common numerical sex chromosome disorder with a frequency of approximately 1/500 to 1/1000 male births2–4). Affected males have at least one additional X chromosome (47, XXY is the classic form), resulting in a tall and slender build, hypogonadism, gynecomastia, small testes, sparse body hair, diminished libido, and infertility. Hormone replacement therapy with testosterone enanthate is performed to improve libido, bone density, and quality of life5). It has been reported that patients with Klinefelter syndrome tend to develop diabetes mellitus6). Exenatide (exendin-4) is a 39 amino acid incretin analog that exhibits similar glucoregulatory ef- Case Report In September 2012, a 59-year-old man was admitted to our hospital for the management of acute pyelonephritis and poor glycemic control. He had a history of type 2 diabetes that had been diagnosed more than 32 years earlier, and was on insulin thera- Division of Metabolism and Endocrinology, St. Marianna University School of Medicine 89 Nagai Y Nakamura Y et al 126 py. Despite a high daily insulin dose of 150 units, blood glucose was poorly controlled, and the patient had a neurogenic bladder with recurrent urinary tract infections. He showed mental impairment, but his behavior was gentle. He was 175 cm tall and weighed 114 kg (his body mass index (BMI) was 36.0 kg/m2). His temperature was 38.5°C, blood pressure was 113/83 mmHg (on losartan at 50 mg/day), and pulse rate was 68/min. Neither rales nor heart murmurs were audible. Ankle jerk reflexes and vibration sensations in his feet were decreased due to diabetic neuropathy. Examination of the ocular fundus showed stage A3p diabetic retinopathy according to the modified Fukuda’s classification. His sense of smell was normal. Gynecomastia was evident. His penis was the size of a thumb, and each testis was the size of the tip of the little finger. Pubic hair was very sparse. There was no relevant family history. Laboratory data obtained on admission are shown in Table 1. Biochemistry tests revealed normal liver and renal function, as well as a normal lipid profile. Fasting plasma glucose was 335 mg/dl and hemoglobin A1c (HbA1c) was 9.1%. Fasting serum C-peptide reactivity (CPR) and urine CPR were 0.9 ng/ml and 36.7 µg/ day, respectively, which were moderately low. Serological tests showed slight elevation of C-reactive protein (CRP), while antiglutamic acid decarboxylase (GAD) antibody and IA-2 antibody were negative. Other test results were almost all within the normal range. Urinalysis showed moderate proteinuria, and the sediment contained 10–19 red cells and 20–29 white cells per high-power field. Chromosomal analysis revealed that his karyotype was 47, XXY (Fig. 1). Deletion of chromosome 15q11-q13 was not detected by fluorescence in situ hybridization (FISH) analysis. Hormonal studies showed that both LH and FSH were elevated, while the levels of total and free testosterone were very low (Table 2). These findings were consistent with hypergonadotropic hy- Table 1. Laboratory Findings on Admission Urinalysis Glucose Protein Ketone bodies WBC Occult blood Urine CPR Complete blood count RBC Hb Ht WBC Platelets Biochemistry tests Total protein Albumin AST ALT ALP LDH γGTP CPK BUN Creatinine Uric acid T-chol Triglycerides HDL-C Na K Cl Ca P CRP FPG HbA1c Other tests Ccr 24h Karyotype (2+) (+) 0.4 (-) (2+) 20-29 (2+) 10-19 36.7 6 369㽙10 12.7 37.7 6600 3 9.3×10 7.3 3.7 16 16 203 157 34 90 11.7 0.8 5.9 148 83 41 131 4.2 91 9.0 2.4 3.76 335 9.1 74.3 47, XXY g/day /HPF /HPF μg/day /μl g/dl % /μl /μl g/dl g/dl IU/l IU/l IU/l IU/l IU/l IU/l mg/dl mg/dl mg/dl mg/dl mg/dl mg/dl mEq/l mEq/l mEq/l mg/dl mg/dl mg/dl mg/dl % Table 2. Results of Endocrine Studies LH FSH ACTH PRL GH TSH Free T3 Free T4 Serum cortisol Serum total testosterone Serum free testosterone Serum DHEA-S ml/min 90 19.4 21.2 37.2 28.9 0.03 1.3 2.6 1.2 11.9 0.42 <0.4 126 mIU/ml mIU/ml pg/ml ng/ml ng/ml μU/ml pg/ml ng/dl μg/dl ng/ml pg/ml μg/dl Exenatide for Klinefelter syndrome 127 Fig. 1. Karyotype of the patient shows the 47, XXY pattern. decreased after starting this regimen, and the insulin dose also gradually declined from 150 units. Eventually, insulin was stopped on the 37th day. Klinefelter syndrome was diagnosed from the chromosomal and hormonal findings, although his physical characteristics (e.g. gross obesity) did not fit the classical phenotype of the syndrome. Because he had hypogonadism, 125 mg of testosterone enanthate was injected intramuscularly every 2 weeks (on the 14th and 28th days of the month). At discharge, total %FAT was unchanged (39.8%), even though his weight had decreased by 17.5 kg. pogonadism, suggesting the presence of primary hypogonadism. The chest radiograph and electrocardiogram were normal. The percentage of body fat (%FAT) and the bone mineral density (BMD) were evaluated by dual energy X-ray absorptiometry (DEXA). On admission, the total %FAT was 40% and the BMD was normal at 1.086 g/cm2 (92% of the young adult mean). Clinical course (Fig. 2) After admission, antibiotic therapy was started with intravenous infusion of tazobactam sodium/ piperacillin sodium (TAZ/PIPC) at 9.0 g daily for the first 10 days, followed by oral trimethoprim-sulfamethoxazole (4.0 g/day) for 2 weeks. The patient’s fever and CRP level improved after 7 days. Before admission, he injected 30 units of insulin glulisine before each meal and 30 units of insulin glargine before breakfast and dinner (a total of 150 units/day). In order to decrease his insulin requirement, after initiating diet therapy at 1,800 kcal (26.7 kcal/ideal body weight), we started to administer 5 µg of exenatide twice daily, which was increased to 10 µg twice daily after 2 weeks. He also commenced treatment with metformin (750 mg/day) 10 days after admission, and glimepiride (0.5 mg/day) was added on the 33rd hospital day. His blood glucose level gradually Discussion One characteristic of our patient was gross obesity, although patients with Klinefelter syndrome are typically tall and slender. One of the most common genetic causes of obesity is Prader-Willi syndrome (PWS), which is characterized by hypogonadism, mental retardation, and hyperphagia. The deletion responsible for PWS has been localized to 15q11q13, but FISH did not detect this deletion of chromosome 15 in our patient. Instead, he had Klinefelter syndrome with the 47, XXY karyotype, as shown in Fig. 1. Some patients with Klinefelter syndrome exhibit all of the typical signs of this disorder, whereas others lack many of its features, because of the wide 91 Nagai Y Nakamura Y et al Insulin(U) Exenatide (μg) Metformin(mg) 128 2500 2000 1500 1000 500 0 20 10 0 150 100 50 0 500 BG 8:00 BG 12:00 Blood glucose (mg/dl) Testosterone enanthate (125 mg) ↓ 400 ↓ BG 18:00 BG 21:00 300 200 100 weight: 96.6 kg body fat: 39.8% weight: 114.0 kg body fat: 40.0% 0 0 5 10 15 20 25 30 35 40 Days after admission Fig. 2. Clinical course of the patient after admission. variability in phenotypic expression8). Ota reported that 24% of Japanese Klinefelter syndrome patients with diabetes had a BMI of more than 25.09). The weight gain in our patient may have been caused by overeating due to being overfed by his 90-year-old mother and by low energy expenditure because of his bedridden lifestyle. There was a marked improvement in his weight coupled with reduced food consumption over a 39day period of hospitalization. During the hospital stay, he never complained of hunger, probably due to the effects of exenatide. Interestingly, he never had a positive urine test for ketone bodies, which are produced from excess acetyl-CoA derived from the β-oxidation of fatty acids. These findings suggest that exenatide is well tolerated and is effective for increasing satiety and improving glycemic control in obese diabetic patients with Klinefelter syndrome. Treating hypogonadism with testosterone may also have influenced glycemic control. We have previously reported that the serum testosterone level is negatively associated with metabolic syndrome, which features visceral obesity, insulin resistance, hypertension, glucose intolerance, and dyslipidemia10). Testosterone treatment of middle-aged men with abdominal obesity decreases intra-abdominal fat and increases insulin sensitivity11). In addition, Bojesen et al. reported a reduction of both truncal fat and fasting plasma glucose by testosterone treatment compared to these parameters without treatment in a study of 70 Klinefelter syndrome patients12). However, testosterone did not alter the body composition of our patient (at least, not after one month), suggesting that hormone replacement was not the main reason for his reduced insulin requirement. Longer follow-up will be needed to determine whether testosterone replacement therapy has a beneficial effect on body composition and glycemic control in this patient. It was recently reported that obesity and diabetes could be successfully treated by using exenatide in patients with PWS13)14). A single dose of exenatide increases satiety separately from appetite hormones, and exerts glucose-lowering and insulinotropic effects on PWS15). A similar mechanism might explain the association between exenatide treatment and in92 Exenatide for Klinefelter syndrome creased satiety in our case, but this remains speculative because we did not measure ghrelin or other appetite hormones. Delayed gastric emptying could also possibly have made a contribution. Nevertheless, it is noteworthy that our patient required no insulin for glycemic control following the administration of exenatide. In conclusion, GLP-1 analog may be a therapeutic option for obese diabetic patients with Klinefelter syndrome due to appetite suppression and weight reduction that decrease insulin resistance and improve overall glycemic control. 7) 8) 9) Disclosure 10) None of the authors have any potential conflicts of interest associated with this research. References 11) 1) Klinefelter HF Jr, Reifenstein EC Jr, Albright F. Syndrome characterized by gynecomastia, aspermatogenesis without a-Leydigism and increased excretion of follicle-stimulating hormone. J Clin Endocrinol 1942; 2: 615–627. 2) Maeda T, Ohno M, Matsunobu A, Yoshihara K, Yabe N. A cytogenetic survey of 14,835 consecutive liveborns. Jinrui Idengaku Zasshi 1991; 36: 117–129. 3) Nielsen J, Wohlert M. Chromosome abnormalities found among 34,910 newborn children: results from a 13-year incidence study in Arhus, Denmark. Hum Genet 1991; 87: 81–83. 4) Herlihy AS, Halliday JL, Cock ML, McLachlan RI. The prevalence and diagnosis rates of Klinefelter syndrome: an Australian comparison. Med J Aust 2011; 194: 24–28. 5) Nielsen J, Pelsen B, Sørensen K. Follow-up of 30 Klinefelter males treated with testosterone. Clin Genet 1988; 33: 262–269. 6) Nielsen J, Johansen K, Yde H. Frequency of diabetes mellitus in patients with Klinefelter’s syndrome of different chromosome constitutions and the XYY syndrome. Plasma insulin and 12) 13) 14) 15) 93 129 growth hormone level after a glucose load. J Clin Endocrinol Metab 1969; 29: 1062–1073. Schnabel CA, Wintle M, Kolterman O. Metabolic effects of the incretin mimetic exenatide in the treatment of type 2 diabetes. Vasc Health Risk Manag 2006; 2: 69–77. Groth KA, Skakkebæk A, Høst C, Gravholt CH, Bojesen A. Clinical review: Klinefelter syndrome a clinical update. J Clin Endocrinol Metab 2013; 98: 20–30. Ota K, Suehiro T, Ikeda Y, Arii K, Kumon Y, Hashimoto K. Diabetes mellitus associated with Klinefelter’s syndrome: a case report and review in Japan. Intern Med 2002; 41: 842–847. Katabami T, Kato H, Asahina T, et al. Serum free testosterone and metabolic syndrome in Japanese men. Endocr J 2010; 57: 533–539. Mårin P, Holmäng S, Jönsson L, et al. The effects of testosterone treatment on body composition and metabolism in middle-aged obese men. Int J Obes Relat Metab Disord 1992; 16: 991– 997. Bojesen A, Kristensen K, Birkebaek NH, et al. The metabolic syndrome is frequent in Klinefelter’s syndrome and is associated with abdominal obesity and hypogonadism. Diabetes Care 2006; 29: 1591–1598. Seetho IW, Jones G, Thomson GA, Fernando DJ. Treating diabetes mellitus in Prader-Willi syndrome with exenatide. Diabetes Res Clin Pract. 2011; 92: e1-e2. Paisey RB, Bower L, Rosindale S, Lawrence, C. Successful treatment of obesity and diabetes with incretin analogue over four years in an adult with Prader-Willi syndrome. Practical Diabetes 2011; 28: 306–307. Sze L, Purtell L, Jenkins A, et al. Effects of a single dose of exenatide on appetite, gut hormones, and glucose homeostasis in adults with Prader-Willi syndrome. J Clin Endocrinol Metab 2011; 96: E1314-E1319.