Heart Rate and Physical Fitness - H

Heart Rate and Physical Fitness
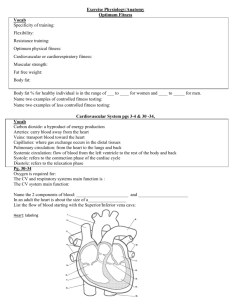
The circulatory system is responsible for the internal transport of many vital substances in humans, including oxygen, carbon dioxide, and nutrients. The components of the circulatory system include the heart, blood vessels, and blood.
Heartbeats result from electrical stimulation of the heart cells by the pacemaker, located in the heart’s inner wall of the right atrium. Although the electrical activity of the pacemaker originates from within the heart, the rhythmic sequence of impulses produced by the pacemaker is influenced by nerves outside the heart. Many things might affect heart rate, including the physical fitness of the individual, the presence of drugs such as caffeine or nicotine in the blood, and the age of the person.
As a rule, the maximum heart rate of all individuals of the same age and sex is about the same. However, the time it takes individuals to reach that maximum level while exercising varies greatly. Since physically fit people can deliver a greater volume of blood in a single cardiac cycle ( stroke volume ) than unfit individuals, they can usually sustain a greater work level before reaching the maximum heart rate. Physically fit people not only have less of an increase in their heart rate during exercise, but their heart rate recovers ( recovery rate ) to the resting rate more rapidly than unfit people.
In this experiment, you will evaluate your physical fitness. An arbitrary rating system will be used to “score” fitness during a variety of situations. Tests will be made while in a resting position, in a prone position, as well as during and after physical exercise.
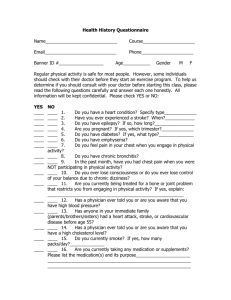
Important: Do not attempt this experiment if physical exertion will aggravate a health problem. Inform your instructor of any possible health problems that might be affected if you participate in this exercise.
PROCEDURE
Each person in a lab group will take turns being the subject and the tester. When it is your turn to be the subject, your partner will be responsible for recording the data on your lab sheet.
Set up the Heart Rate Monitor. Open up Logger Pro,go to File, then Open. From the menu choose the
Human Physiology folder, then exercise lab template.
Follow the directions for your type of Heart Rate
Monitor.
Using a Hand-Grip Heart Rate Monitor a.
Grasp the handles of the Hand-Grip Heart Rate
Monitor. Place the fingertips of each hand on the reference areas of the handles (see Figure 1). b.
The left hand grip and the receiver are both marked with an alignment arrow. When collecting data, be sure that the arrow labels on each of these devices are in alignment and that they are not too far apart. c. Make sure the receiver module of the Heart Rate
Monitor is within 80 cm (3 feet) of the transmitter in the hand grips. It often helps if your lab partner holds it close to your hands. Make sure there are at least 8 feet between you and anyone using a monitor AND that all cell phones are OFF.
Stand quietly facing your table or lab bench.
Click to begin data collection. There will be a 15 second delay while data are collected before the first point is plotted on the heart rate graph. Thereafter, a point will be plotted every 5 s.
Determine that the Heart Rate Monitor is functioning correctly. The readings should be consistent and within the normal range of the individual, usually between 55 and 100 beats per minute. If readings are stable, click and continue to the next step.
A. Standing heart rate
1. Stand upright for 2 minutes. When the 2 minutes have passed, record your heart rate in Table 6.
2. Locate your heart rate in Table 1 and record the corresponding fitness point value in Table 6.
Beats/min
60–70
71–80
81–90
Points
Table 1
Beats/min
12
11
10
101–110
111–120
121–130
Points
8
7
6
91–100
B. Reclining heart rate
1. Recline on a clean surface or table.
9 131–140 4
1b Make sure that the time interval (the icon just to the left of the green and begin recording.
1c. Record your heart rate at 1 minute has passed and record in Table 6.
button) is set to 200 seconds
2. Locate your heart rate in Table 2 and record the corresponding fitness point value in Table 6.
Beats/min
50–60
61–70
Points
Table 2
Beats/min
12
11
81–90
91–100
Points
8
6
71–80 10
Continue to remain reclining and start a new recording
C. Baroreceptor reflex
101–110 4
Orthostatic hypotension occurs when one stands quickly. Blood pressure drops as gravity pulls blood into the legs.
Baroreceptors in the carotid relay this to the cardiac control center, which then activates the baroreceptor reflex which activates the sympathetic system, thereby increasing heart rate and causing constriction of the arterioles. Thus the flow of blood from the brain is counteracted and normal standing blood pressure and heart rate return.
1. As you continue to record heart rate, at 50 seconds quickly stand up and remain standing still.
2. Monitor your heart rate as it drops and then increases, and record the peak heart rate in Table 6. Stop when your rate reaches standing rate. Print your curve, label resting heart rate, orthostatic hypothesion, baroreceptor reflex, normal standing heart rate, and attach to your report
3. Subtract the reclining rate heart rate recorded from the standing heart rate in to find the heart rate increase after standing. Locate the row corresponding to the reclining heart rate in Table 3 and use the heart rate increase value to determine the proper fitness points. In Table 6, record the fitness points. Rest for 2 minutes then proceed to the next section.
Table 3
Reclining heart rate Heart rate increase after standing
0–10 11–17 18–24 25–33 34+
50–60
61–70
12
12
11
10
10
8
8
6
6
4
11 9 6 4 2 71–80
81–90
91–100
101–110
10
8
6
8
6
4
4
2
0
2
0
0
0
0
0
Step test
1. Before performing the step test, record your heart rate (Pre-exercise) in Table 6.
2. Perform a step test using the following procedure: a. Set the time interval for 200 seconds. Begin recording heartrate . b. Once it has stabilized, restart and begin recording. At 50 seconds, place the right foot on the top of the “step”, step up with the left foot, then step down with the right foot, and then the left foot.
This stepping cycle should take 3 seconds to complete.
Repeat, starting with the right foot.
3. When 30 steps have been completed, record the time and heart rate in Table 6.
4. While still recording, you should now remain standing and be relatively quiet during the recovery period.
Continue recording the heart rate until the readings return to the recorded pre-exercise heart rate value. On the graph use the highlight function to indicate WHEN the stepping stopped and WHEN heart rate returned to “normal”. Use these points to determine the recovery time. Record the recovery time in Table 6 and print your curve. Label the exercise and recovery intervals (and times) on the graph. Attach to your report
5. Now locate your recovery time in Table 4 and record the corresponding fitness point value in Table 6. If your heart rate did not return to within 10 beats/min from their pre-exercise heart rate, record a value of 6 points.
Table 4
Time (sec)
0–30
31–60
61–90
Points
14
12
10
91–120 8
Step test: Endurance
21. Subtract your pre-exercise heart rate from their heart rate after 30 steps of exercise. Record this heart rate increase on your graph and in the endurance row of Table 6.
22. Locate the row corresponding to the pre-exercise heart rate in Table 5 and use the heart rate increase value to determine the proper fitness points. In Table 6, record the fitness points.
Pre-exercise heart rate
Table 5
Heart rate increase after exercise
60–70
71–80
81–90
91–100
101–110
111–120
121–130
0–10 11–20 21–30 31–40 41+
12 12 10 8 6
12
12
10
10
8
7
6
4
4
2
10
8
8
6
8
6
4
2
6
4
2
1
2
1
1
0
0
0
0
0
131+ 5 1
Total all the fitness points recorded in Table 6.
Table 6
Condition
Standing heart rate
Reclining heart rate
Rate or time beats/min beats/min
Reclining to standing
Pre-exercise heart rate
After 30 steps
Recovery time beats/min beats/min beats/min seconds
0 0 0
Points
No points
No points
Endurance beats/min
Your Score __________
Total points:
Determine your personal fitness level using the scale below.
Low
Fitness
Average
Fitness
Exceptional
Fitness
20 30
What is your usual form/type of exercise?
Class results
Weekly Exercise
(Hours)
30-35 36-40
0
1-2
2-4
4-8
8+
41-46
40
46-50
50
51-55
60
56-60
QUESTIONS
1. How did your heart rate change after moving from a standing position to a reclining position and then back to a standing? Explain why gravity is involved with this change. What would happen to blood pressure during this action?
2. Predict what your heart rate might be if you had exercised for sixty steps instead of 30. Explain in terms of oxygen and muscles.
3. Smoking causes the blood vessels to constrict. How, and why, does this effect blood pressure? Why is this considered a health hazard for the heart?
4. The graph shows the changes in heart rate and stroke volume as a heart responds to exercise. is known that the stroke volume of a heart increases with training. The subject for this graph was a well-trained marathoner. Using the information discussed in this lab, how would the curves be different for “normal”?
On graph draw in an approximation of stroke volume and heart rate for this new subject, and explain how you determined each curve.
Explain!
170
160
150
140
130
120
110
100
90
0
Stroke Volume
Heartrate
10 20
Cardiac Output (L/min)
30
5. Current research indicates that, especially for individuals with CAD, many heart attacks occur as people get out of bed and stand up after a night of sleep. Given your response to #1, account for this observation.
6. Based on the class results, is this particular fitness test a somewhat reasonable measurement of fitness? Explain.
200
It
180
160
140
60
40
40
120
100
80
Exercise and the Cardiovascular System
From Martini, F., Fundamentals of Anatomy and
Physiology
At rest, the average heart pumps about 5.8 liters per minute. This parameter is referred to as cardiac output, is equal to the amount of blood pumped per beat ( stroke volume ) times the number of times the heart beats per minute (heart rate ).
Light Exercise
As you begin light exercise the following interrelated changes take place:
A. Extensive dilation of the arteries occurs as the rate of oxygen consumption in skeletal muscles increases, leading to an increase in blood flow through the muscle capillaries and then into the venous system.
B. The flow of venous blood increases as skeletal muscle contraction squeeze blood along the veins.
C. The increase of blood flow into the heart causes the heart muscle to stretch, leading it to pump more blood per beat (stroke volume) and to beat more frequently and greater force. These produce an increase in cardiac output to about double resting levels. The increase produces greater blood flow to skeletal muscles, cardiac muscle, and the skin.
Heavy Exercise
At higher levels of exertion, the demand for oxygen requires the heart to pump significantly more blood.
The cardiac control center in the brain responds to the need for more oxygen by stimulating the release of epinephrine at the SA node. The resulting increase in beats per minute can increase cardiac output to levels as high as 20-25 liters per minute. But that is still not enough to meet the demands of active skeletal muscles, so the flow of blood to “nonessential" organs, such as those of the digestive system, is reduced, making more blood available to the muscles. During exercise at maximal levels, blood essentially races between the skeletal muscles, the lungs and the heart. Only the blood supply to the brain remains unaffected.
Exercise, Cardiovascular Fitness, and Health
Cardiovascular performance improves significantly with training. The table below compares the cardiac performance of athletes with that of nonathletes. Trained athletes have bigger hearts and larger stroke volumes than do nonathletes, and these are important functional differences.
Cardiac output is equal to the stroke volume times the heart rate; thus, for the same cardiac output, the person with a larger stroke volume has a slower heart rate. An athlete at rest can maintain normal blood flow at a heart rate as low as 32 beats per minute, and, when necessary, the athlete's cardiac output can increase to levels 50 percent higher than those of nonathletes. Thus, a trained athlete can tolerate sustained levels of activity that are well beyond the capabilities of nonathletes. This is also evident in an athlete’s response to exercise. Because of the greater stroke volume, the athlete’s heart rate will, when exercising, not increase as fast as a nonathlete’s. It will also return to resting rate much faster once the exercise ends. Both of these are used to determine the cardiac fitness of a person.
Nonathlete (rest)
Nonathlete (maximum)
Heart
Weight (gm)
300
Stroke
Volume
(ml)
60
104
Heart Rate
(BPM)
83
192
Cardiac
Output
(L/min)
5.0
19.9
Blood
Pressure
120/80
187/75
Athlete (rest)
Athlete (maximum) 500
100
167
53
182
5.3
30.4
120/80 ca. 200/90
Exercise and Cardiovascular Disease
Regular exercise has several beneficial effects. Even a moderate exercise routine (jogging 5 miles a week, for example) can lower total blood cholesterol levels. A high cholesterol level is one of the major risk factors for atherosclerosis, which leads to cardiovascular disease and strokes. In addition, a healthy lifestyle
- regular exercise, a balanced diet, weight control, and not smoking – reduces stress, lowers blood pressure, and slows the formation of plaques.
Regular moderate exercise may cut the incidence of heart attacks almost in half. However, only an estimated
8 percent of adults in the United States currently exercise at recommended levels. Exercise is also beneficial in accelerating recovery after a heart attack. Regular light-to moderate exercise (such as walking, jogging, or bicycling), coupled with a low-fat diet and a low-stress lifestyle, not only reduces symptoms of coronary artery disease (such as angina), but also improves one's mood and overall quality of life. However, exercise does not remove any underlying medical problem, and atherosclerotic plaques, do not disappear and seldom grow smaller with exercise.
There is no evidence that intense athletic training lowers the incidence of cardiovascular disease. On the contrary; the strains placed on all physiological systems - including the cardiovascular system - during an ultramarathon, ironman triathlon, or other extreme athletic event can be severe. Individuals with congenital aneurysms (localized weakening of arterial wall), cardiomyopathy (weakness of the heart muscle), or cardiovascular disease risk fatal circulatory problems such as an arrhythmia or heart attack, during severe exercise. Even healthy individuals can develop acute physiological disorders, such as kidney failure, after extreme exercise.