duodenal mucosal protection by bicarbonate secretion and its
advertisement

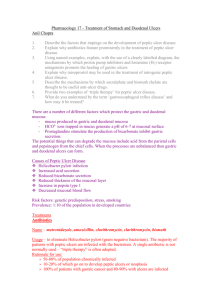
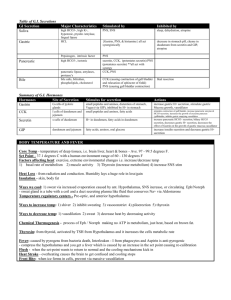
JOURNAL OF PHYSIOLOGY AND PHARMACOLOGY 2004, 55, Suppl 2, 517 www.jpp.krakow.pl S.J. KONTUREK*,P. C. KONTUREK**, T. PAWLIK***, Z. SLIWOWSKI*, W.OCHMAÑSKI***, E. G. HAHN* DUODENAL MUCOSAL PROTECTION BY BICARBONATE SECRETION AND ITS MECHANISMS * Department of Physiology, Jagiellonian University Medical College, Cracow, Poland ** First Department of Medicine, University Erlangen-Nuernberg, Erlangen, Germany *** Department of Internal Medicine and Gerontology, Jagiellonian Medical College Proximal portion of duodenum is exposed to intermittent pulses of gastric H + discharged by the stomach. This review summarizes the mechanisms of duodenal mucosal integrity, mainly the role of mucus-alkaline secretion and the mucous barrier protecting surface epithelium against gastric H . The mucous barrier protects the + leaky duodenal epithelium against each pulse of gastric H , which penetrates this + barrier and diffuses into duodenocytes, but fails to damage them due to; a) an enhanced expression prostaglandins (PG) production of intestimal peptide several NO, of and cyclooxygenase-1 of nitric stimulating neurotransmitters also (VIP), oxide duodenal HCO3 stimulating pituitary (COX-1), (NO) - with synthase release (NOS) of with, protective however, secretion and b) the release of HCO3 secretion such as vasoactive adenylate-cyclase activating polypeptide (PACAP), acetylcholine, melatonin, leptin and ghrelin released by enteric nerves and mucosal cells. At the apical duodenocyte membrane at least two HCO3 /Cl anion + exchangers operate in response to luminal H to provide adequate extrusion of HCO3 into duodenal lumen. In the basolateral portion of duodenocyte membrane, both non+ electrogenic (NBC) and electrogenic (NBCn) Na -HCO3 cotransporters are activated by the exposure to duodenal acidification, causing inward movement of HCO3 from extracellular fluid to duodenocytes. There are also at least three Na /H + amiloride-sensitive exchangers, eliminating H + + (NHE1-3) which diffused into these cells. The Helicobacter pylori (Hp) infection and gastric metaplasia in the duodenum with bacterium inoculating metaplastic mucosa and inhibiting HCO3 secretion by its endogenous inhibitor, asymetric dimethyl arginine (ADMA), may result in duodenal ulcerogenesis. Key w o r d s : Duodenal mucosal barrier, duodenal HCO3 , prostaglandins, CCK, vagal nerves, sodium-bicarbonate cotransport, H /Na + /Cl exchanger - + nitric oxide, exchanger, HCO3 - 6 INTRODUCTION The duodenal cluster unit consists of a group of organs, including duodenum itself, stomach, pancreas, liver and biliary tree. These organs originate embryologically from the closely related structures, whose functions are regulated, at least in part, by the duodenum. The lining of the duodenum is equipped with a variety of receptors sensitive to chemical (pH, osmolarity, and nutrients) and physical factors (pressure and contractility of duodenum) that activate neurohormonal mechanisms maintaining the integrity of the duodenal mucosa and also involved in the control of gastric, pancreatic and hepato-biliary functions. This article is designed to overview the mucoso-protective and anti-ulcer mechanisms of the duodenum, which is intermittently exposed to various irritants emptied by the stomach, especially the aggressive factors such as gastric acid (H ) + and pepsin as well as other irritants present in the ingested food, contaminated by bacteria and their toxins or originating from the stomach or biliary tree. Since its identification in the stomach by Prout in 1823 of HCl (1), its secretory mechanisms have been the subject of extensive investigations during last century leading to discovery of such stimulants as vagal nerves by Pavlov in 1886 (2), gastrin by Edkins in 1906 (3), and histamine by Popielski in 1916 (4). With the synthesis of antagonists of H2-receptors discovered by Black (5) and proton pump inhibitors by Sachs et al. (6), that were found to inhibit all forms of gastric secretion including that induced by meal, a major break-through occurred in gastric physiology (Fig. 1). Gastric acid and pepsin as aggressive factors Gastric acid (and pepsin), is considered as major aggressive factor against the gastro-duodenal mucosa as outlined in 1910 by German surgeon, K. Schwarz (7), who formulated famous dictum "No acid - no ulcer", implying that the presence of acid is the "condition sine qua non" of ulcer formation (see Fig. 1). It is of interest that in the same publication, Schwarz considered "the mucosal resistance" as important factor contributing to the possible ulcerogenesis. Schwarz's dictums related to pathogenesis of peptic ulcer formation was not challenged until Allen and Garner (8) and then Flemstrom and Garner (9) provided direct evidence for the ability of gastro-duodenal mucosa to respond to the action of gastric acid with an immediate and abundant secretion of HCO3 . Apparently, the secretion of HCO3 - was soon found to be an active, metabolism-dependent transport occurring along the entire gastrointestinal tract. Duodenal alkaline secretion As peptic ulcers in humans develop both in the stomach and duodenum, especially in its upper portion, duodenal cup, we used dogs with canulated pouches prepared from the oxyntic and antral portions of the stomach and with 7 Major discoveries and historical figures in gastrology * the presence of HCl in the stomach by W. Prout in 1823 * gastric HCl secretion controlled by vagus by I.P. Pavlov in 1895 * gastric HCl secretagogue - gastrin by J.S. Edkins in 1902 * histamine as gastric HCl secretagogue by L. Popielski in 1916 * H2-receptor antagonists by J. Black in 1972 and proton pump inhibitors by G. Sachs in 1980 showed that they inhibit HCl secretion stimulated by various stimuli (histamine, histamine, vagal excitation & meal) meal) and exbibit antianti-ulcer efficacy * lend support for old K. Schwarz’s (1910) concept that ulcer formation requires gastric acid to attenuate mucosal protection and induce ulcer according to his dictum „NO ACID NO ULCER” Mucosal resistance Parietal cells Acid G Gastrin Fig. 1. Historical background of major discoveries in gastrology supporting the initial concept of Schwarz dated from 1910 that gastric acid is required as an aggressive factor to attenuate mucosal protection and to induce gastric or duodenal peptic ulceration. loops fashioned from the proximal and distal duodenum, a direct evidence was obtained evidence that, indeed, upper GI mucosa possesses the ability to secrete HCO3 , the most effective in this respect being proximal part of the duodenum, though some less impressive alkaline secretion was also noticed in distal duodenum and in the gastric antrum and corpus (10). Another study on the in situ perfused proximal duodenum including duodenal bulb kept between two balloons in conscious dogs, showed higher HCO3 - secretion than that released by the isolated (and externally denervated) proximal duodenal loop of similar length, suggesting an important role of extrinsic autonomic innervation in the maintance of this secretion (11). Interestingly, such denervation of the proximal duodenum resulted also reflexes controlling in the elimination gastric H + of acid-induced secretion (12). duodeno-gastric Actually, the inhibitory balance between protective and aggressive factors acting on the mucosa plays a decisive role in the pathogenesis of mucosal lesion or integrity (Fig. 2). As expected from the concept of Boldyreff's (13), who first recognized at the end of 19 th century the cyclic periodicity of motor and secretory gastrointestinal functions, it was found that also the duodenal alkaline secretion shows periodicity 8 Peptic ulcer Mucosal integrity Aggressive Factors (excessive H+-pepsin, pepsin, NSAIDs, NSAIDs, H. pylori ) Fig. 2. The imbalance between various Protective Factors (mucus-HCO mucus-HCO3secretion mucosal barrier, barrier, mirocirculation, mirocirculation, mucosa restitution ) aggressive and protective factors contribute to ulcerogenesis. in phase with migrating motor complex (MMC), reaching peaks at phases II and III and nadir at phase I of this MMC (10). Feeding interrupts this periodicity and induces more uniform alkaline secretion. The rise in HCO3 - at the phase II and III has been attributed to the alkaline stimulation by increments in plasma motilin and ghrelin and activation of cholinergic neurons of enteric nervous system (ENS) as this alkaline secretion can be suppressed by atropine (11). Since at phase II/III, there is also an increase in gastric acid secretion and enhanced gastric emptying with progressive motor activity, it is possible that gastric H + into the duodenum acts on luminal duodenal HCO3 - partial pressure, pCO2, stimulating additionally HCO3 - discharged to release CO2, raising its secretion (11). Vagal excitation, such as achieved with sham-feeding in dogs, was found to result in a dramatic stimulation of proximal duodenal alkaline secretion that could be partly attenuated using atropine (11), suggesting that vagal-cholinergic innervation plays an important role in the regulation of sham-feeding-induced secretion, that was duodenal HCO3 . Unlike vagally-induced duodenal HCO3 relatively little affected by suppression of prostaglandin (PG) biosynthesis with indomethacin (11), basal and HCl- or arachidonic acid-induced duodenal alkaline secretion was found to be PG-dependent. These acidic stimulants applied on the 9 duodenal mucosa caused concentration-dependent increase in the HCO3 - as well as in mucus glycoprotein secretion (14). The increase in duodenal HCO 3 brought about by arachidonic acid were prevented by the pre-treatment with indomethacin similarly as those induced by HCl. As mucus layer covering the epithelial surface of the duodeum is the first line of mucosal defense against chemical, predominantly acidic irritant, as well as the mechanical, bacterial or enzymatic insults, the components responsible for these protective functions appear to be highly glycosylated mucus glycoproteins. Following arachidonate application, mucus glycoproteins were significantly enriched in phospholipids and this certainly enhanced the protective qualities of the mucus gel. Using similar to our technique of duodenal perfusion technique in humans, Isenberg and his colleagues (15) found that in normal subjects, the proximal duodenal HCO 3 secretion reached higher values than that in distal duodenum and that it was greatly enhanced by mucosal acidification or administration of exogenous PGE2. In contrast, duodenal ulcer (DU) patients show reduced HCO3 - response to luminal acid, despite of higher endogenous PGE2 release by proximal duodenum due to overexpression of COX-2 and this deficiency of alkaline secretion has been attributed to mucosal infection with Hp, inflammation and scarring (16). The eradication of Hp was found to increase duodenal alkaline secretion and this could be attributed to the recovery of duodenal mucosa from the inflammation induced by Hp infecting the gastric metaplastic areas in the duodenum (16). These and other studies seem to confirm that both in humans and animals, PGE2 is a potent stimulant of duodenal HCO3 - secretion and appears to be responsible, at least in part, for basal and acid-induced alkaline secretion (12, 13, 16, 17). The mucus-alkaline secretion occurs in the mucosa of the entire gastrointestinal tract, the most extensive being that of duodenum, where mucous cells exhibit high activity of carbonic anhydrase and active exchanger HCO3 extruding HCO3 - - /Cl - into the duodenal lumen (Fig. 3). Neuro-hormonal mechanisms of alkaline secretion In addition to PG, numerous other substances both naturally occurring or used therapeutically, have been reported to contribute to the stimulation of duodenal alkaline secretion. We reported that sucralfate and colloidal bismuth citrate (DeNol), administered in humans in peptic ulcer therapy, increased significantly duodenal HCO3 - secretion and this has been attributed to PG-dependent stimulation, but as bismuth is known to suppress H. pylori (Hp) activity, this effect could be also explained by the eradication or, at least, suppression of this bacterium infection in these subjects though testing for Hp was not available at this time (20). Since administration of L-nitro-arginine derivatives, such as L-NNA, was reported to inhibit gastric and duodenal alkaline secretion and these effects were reversed by the addition of L-arginine to L-NNA, endogenous nitric oxide (NO) 10 Duodenum (HCO3- secretion) Lumen 3Na+ Saliva 1500 ml/day ATP 2K+ ClHCO3+ Gastric H+ Na+ HCO3- H+ CA Ingest 2000 ml H2O/day H2O +CO2 H2CO3 H2O + CO2 2.25 nM/30 min 2.20 nM/30 min 1500 ml/day HCO3- Duodenal HCO3- Gastric H+ Gastric juice 2000 ml/day Bile 500 ml/day Fig. 3. The mucosa of the duodenum is capable of producing and secreting into the lumen of HCO3 through various mechanisms, out of which the most efficient mechanisms operate in the duodenum. The volume of ingested fluids and secreted juices from various GI organs are also shown. has been also implicated in the regulation of duodenal HCO3 secretion (21). This is in keeping with the observation that exogenous donors of NO, such as glycerine trinitrate, or stimulants of sensory nerves releasing CGRP such as capsacin (at lower doses) were also effective stimulants of gastro-duodenal alkaline secretion (21). This has been confirmed recently by Takeuchi et al. (22), who documented that NO, like PG, is involved in acid-induced duodenal HCO3 secretion and could be attributed to the upregulation of constitutive NO synthase (cNOS) (Fig. 4). Yao et al. (23) identified in in vitro preparation of rabbit duodenal mucosa the HCO 3 - secretory pathways related to vasoactive intestinal peptide (VIP) and cyclic AMP. Glad et al. (24) confirmed in anesthetized pigs that VIP and its chemical (PACAP), Sjoblom analog, stimulate and pituitary duodenal Flemstrom adenylate as (25) well as reported cyclase-activating hepatobiliary recently polypeptide HCO 3 that - secretion. melatonin, a neurotransmitter released by neurons of the enteric nervous system of the gut, is also an effective stimulant of duodenal alkaline secretion in anesthetized rats and suggested that this indole is involved in H -induced alkaline secretion + acting via MT 2 receptors. Furthermore, sensory nerves in the duodenal 11 mucosa, activated by acid or small doses of topical capsaicin, have been proposed to be involved in the stimulation of alkaline secretion ether by axonreflex with the release of sensory neuropeptides such CGRP that in turn activates the release and action of NO (21). The overall mechanisms operating in the duodenum in response to topical application of H NOS-NO and sensory nerves-CGRP-NO systems. + involve COX-PG, Furthermore, novel hormones such as PYY, ghrelin, melatonin VIP, orexins or CCK have been proposed to contribute to duodenal HCO 3 Quantitatively, the amounts of HCO3 - - secretin (Fig. 4). secreted by canine proximal duodenum are only a small portion of the amounts of maximally stimulated gastric H + secreted in the stomach (11). Jarbur et al. (26) who quatitated gastric acid and duodenal alkaline secretion in fasting humans reported that the amounts of HCO3 - produced in the duodenum under basal conditions were similar to duodenal loads of gastric H + and this production may be mediated, at least in part, by increased pCO2 generated in the duodenal lumen from the HCO3 - hydrolysis by gastric H + during phase III of MMC (see Fig. 4). Mucus-alkaline secretion and formation of protective mucosal barrier in the stomach differ from those in the duodenum. In the stomach, gastric mucosa is covered by tight epithelial cells with continuous surface mucus layer to which HCO3 - is secreted by goblet cells, creating the pH gradient across mucus layer that neutralizes any H diffusing from the gastric lumen towards the surface + epithelial cells and thus preventing their acidification and damage (Fig. 5). The total amount of HCO3 - secreted by the gastric mucosa is relatively small when pCO2, COX-1 -PG & cNOS-NO cNOS-NO system Luminal H+1 Neurohumorals: Melatonin, VIP, PACAP, CGRP, Motilin, PYY, OX-A & -B GHRELIN, CCK HCO3transport Cholinergic pathway (Ach) Fig. 4. Involvement of various factors activated by duodenal acid in the mechanisms of HCO3 secretion in duodenal mucosa. 12 Gastric lumen Mucosal defence mechanism H+ pH 1.5 Pepsin MucusBicarbonate Barrier Mucosal defence mechanism H+ Mucus Pepsinogen HCO3H+ Mucus H+ H2O + CO2 Neutralization Epithelial Tigh Junctions HCO3- pH 2.0 HCO3- + pH 7.0 HCO3- HCO3 H+ Fig. 5. In the stomach luminal gastric H + does not reach the mucosal cells because of its neutralization by HCO3 secreted continuously by surface epithelial cells. Pepsin molecules infuse - only into the upper portion of the mucus layer, causing its degradation but do not reach the surface of gastric epithelium. compared to maximal gastric H + secretion, but due to the fact that HCO3 secreted into the thin layer of adherent mucus gel, this HCO3 - - is secretion is highly effective in neutralizing the penetrating luminal H . By contrast the duodenum is + covered, however, by a leaky epithelium and has thicker mucus gel with more abundant secretion mechanism against of HCO3 , gastric H + which is thought discharged to to the duodenum is supplied with large amounts of HCO3 - be the primary duodenum. defence Although, the originating from the pancreas and biliary tree and secreted in response to duodenal acidification due to release of secretin, the major "chemical battlefield" with gastric H + entering the duodenum is the duodenal bulb. The bulb is located just distal to gastric antrum and proximal to the pancreatico-biliary ducts and uniquely exposed to a highly variable pH environment due to peristaltically conveyed pulses of concentrated gastric H discharged by the stomach to duodenum. Since the duodenum does not have inherent + the acid protective structural properties of the stomach with intercellular tight junctions, it evolved very efficient means for defence against gastric H . The proximal duodenum could be compared to the titration chamber + with gastric H + neutralized mostly by the HCO3 - originating from the bulbar 13 mucosa and secreted due to local action on duodenocytes of numerous mediators including already mentioned PG, NO, Ach, melatonin, VIP, PACAP and probably also motilin-like peptide, ghrelin PYY leptin, as well as CCK, all secreted by intestinal mucosal cells and released into the duodenal lumen (see Fig. 4). Duodenocyte membrane transport systems It should be emphasized that HCO3 does not increase immediately upon the start of acid perfusion of duodenal bulb but rather somewhat later after acid challenge when H ions + already diffused into duodenocytes and reduce their intracellular pH (pHi). To understand the sequence of events following duodenal acid challenge, it is necessary to identify the apical and basolateral transport mechanisms in duodenocytes. It has been proposed (26, 27), the apical duodenocyte membrane is equipped with active exchangers HCO3 /Cl , extruding HCO3 to duodenal lumen in exchange for Cl (AE - anion exchanger) and several types of Na /H + + exchangers (NHE1-3) eliminating the H + from the duodenocytes back to duodenal lumen (Fig. 6). The AE has been related to cystic fibrosis transmembrane conductance regulator (CFTR) protein and found to be expressed predominantly in a pical membrane of duodenocytes in duodenal crypts (28, 29). At the baso-lateral + duodenocyte membrane both electroneutral Na -HCO3 cotransport (NBC1) and electrogenic cotransport NBC (NBCn1) as well as N /H + NHE1 pNBC1 Fig. 6. Duodenocytes membrane. are equipped ? HCO3H+ CO2 (HCO3-)n Apical SLC26Ax Cl- exchanger (NHE) are HCO3- ClCFTR + Na+ with numerous AE2 Cltransporters at Basolateral the apical and basolateral 14 Fig. 7. Hipothetical events leading to duodenal ulcerogenesis related to H. infection, pylori increased acid load, duodenitis and ADMA production. present (30). Kaunitz and Akiba (31) summarizing the protective duodenal response to gastric acid challenge in humans pointed out that luminal H diffusing + into the duodenocytes, lowers pHi and initially decreases the buffer power of these cells but subsequently decrease HCO3 secretion due to the decrease of CFTR conductance. Lowering pHi immediately increases, however, the activity of baso- lateral NBC1 and promotes an inward movement of HCO3 from extracellular fluid to increase the cellular content of HCO3 and its secretion to duodenal lumen through CFTR-related HCO3 /Cl exchanger. Furthermore, acidic intracellular pHi increases the activity of basolateral NHE and enhances an extrusion of H + submucosal space with increase of cellular alkali load. Luminal H + into the in the duodenum also increases the mucus secretion from goblet cells, resulting in the increase of the thickness of mucus gel. This increase in mucus secretion is accompanied by an enhancement of mucosal blood flow mediated by the H + stimulation of the sensory nerves releasing CGRP and NO causing vasodilation in the mucosa. H + in duodenum may also release ghrelin and leptin into duodenal lumen from the surface epithelial cells and these peptides, similarly to CCK already reported to stimulate duodenal HCO3 should also be considered as candidate stimulatants of duodenal alkaline secretion of physiological importance. 15 Duodenal ulcer patients may not only exhibit excessive gastric H secretion + and accelerated gastric emptying of H , thus enhancing duodenal acidification + and mucosa damage, but also produce a potent endogenous asymetric dimethylated arginine derivative (ADMA) that reduces duodenal HCO3 to gastric H and + thus favours the damage of duodenal mucosa - response and ulcer formation in these patients (32) (Fig. 7). CONCLUDING REMARKS This overview provides an insight into how duodenal mucosa defends itself against the damage by pulses of concentrated gastric H + entering the duodenum. Unlike in the stomach, where mucosal barrier with tight epithelial cells and covering mucus layer actually prevent luminal H + from entering and damaging the surface epithelium, in the duodenum the epithelial cells are leaky permitting luminal H + to diffuse into the duodenocytes and acidify subsequent activation of the baso-lateral Na -HCO3 + alkali load in these cells and excessive HCO3 apical membrane activates - HCO3 /Cl basolateral duodenocytes and - Na /H + exchangers. + of their interior with cotransporter, leading to secretion due to activation of Acidic exchangers acidification - - pHi causing submucosal of duodenocytes extrusion tissue with of H + also from stimulation of capsaicin receptors on afferent nerves leading to increased mucosal blood flow and increased thickness of mucus-gel layer enhancing duodenal protective activity. In certain conditions such as Hp infection, the inflammatory changes in the mucosa result in decrease in mucus-alkaline secretion, partly due to ADMA effect and mucosal resistance to acid injury leading to the formation of peptic ulcerations. Eradication produce HCO3 - of Hp restores the ability of duodenal mucosa to due to reduction in ADMA formation and the restoration of the integrity of duodenal mucosa. REFERENCES 1. Prout W. On the nature of acid and saline matters usually existing in the stomach of animals. Phil Trans R Soc London 1824; 1: 45-49. 2. Pavlov IP. The Work of the Digestive Glands. Charles Griffin and Co, Ltd, London 1902. 3. Edkins JS. The chemical mechanism of gastric secretion. J Physiol (Lond) 1906; 34: 183. 4. Popielski L. β-inidazolylaethylamin und die Organenextrakte. Einfluss der Saueren auf die Magenssesaftsekretion erregende Wirkung der Organextrakte. Pfueg Arch ges Physiol 1920; 178: 237-259. 5. Black JW, Duncan WAM, Durant CJ, Ganellin CR, Parson ME. Definition and antagonism of H2-receptors. Nature 1972; 236: 385-390 6. Sachs G. Gastritis, Helicobacter pylori and proton pump inhibitors. Gastroenterology 1997; 7. Schwarz K. Ueber Penetrierdende magen- und jejunal geswurw. Breitr Klein chir 1919; 96: 100. 8. Allen A, Garner A. Mucus and bicarbonate secretion in the stomach and their possible role in 112: 1033-1061. mucosal protection. Gut 1980; 21: 249-262. 16 9. Flemstrom G, Garner A. Gastroduodenal HCO3 transport: characteristics and proposed role in regulation and mucosal protection. Am J Physiol 1982; 242: G183-193. 10. Konturek SJ, Tasler J, Bilski J, Kania J. Prostaglandins and alkaline secretion from oxyntic, antral and duodenal mucosa of the dog. Am J Physiol 1983; 245: G539-546. 11. Konturek SJ, Thor P. Relation between duodenal alkaline secretion and motility in fasted and sham-fed dogs. Am J Physiol 1986: 251: G591-G596. 12. Konturek SJ, Bilski J, Tasler J, Konturek JW, Bielanski W, Kaminska A. Role of endogenous prostaglandins in duodenal alkaline response to luminal hydrochrolic acid or arachidonic acid in conscious dogs. Digestion 1986; 34: 268-274. 13. Boldyreff W. Einige neue Seited der Tatigkeit des Pankreas. Ergeb Physiol 1911; 11: 121-217. 14. Kosmala M, Carter SR, Konturek SJ, Slomiany A, Slomiany BL. Mucus glycoprotein secretion by duodenal mucosa in response to luminal arachidonic acid. Biochim Biophys Acta 1986; 884: 419-428. 15. Isenberg JI, Hogan DL, Koss MA, Selling JA. Human duodenal mucosal bicarbonate secretion. Evidence for basal secretion and stimulation by hydrochloric acid and a synthetic prostaglandin W1 analogue. Gastroenterology 1986; 91: 370-378. 16. Bukhave K, prostaglandin Rask-Madsen E2 release J, and Hogan mucosal DL, Koss MA, bicarbonate Isenberg secretion are JI. Proximal altered in duodenal patients with duodenal ulcer. Gastroenterology 1990; 99: 951-955. 17. Flemstrom G. Gastroduodenal mucosal secretion of bicarbonate and mucus. Physiologic control and stimulation by prostaglandins. Am J Med 1986; 18: 18-22. 18. Hogan DL, Rapier RC, Dreilinger A, et al. Duodenal bicarbonate secretion: eradication of Helicobacter pylori and duodenal structure and function in humans. Gastroenterology 1996; 110: 705-716. 19. Mertz-Nielsen A, Hillingso J, Bukhave K, Rask-Madsen J. Indomethacin decreases gastroduodenal mucosal bicarbonate secretion in humans. Scand J Gastroenterol 1995; 30: 1160-1165. 20. Konturek SJ, Bilski J, Kwiecieñ N, Obtulowicz W, Kopp B, Oleksy J. De-Nol stimulates gastric and duodenal alkaline secretion through prostaglandin dependent mechanism. Gut 1987; 28: 1557-1563. 21. Bilski J, Konturek SJ. Role of nitric oxide in gastroduodenal alkaline secretion. J Physiol Pharmacol 1994; 45: 541-553. 22. Takeuchi K, Kogawa S, Mimaki H, Aoi M, Kawauchi S. Cox and NOS isoforms involved in acid-induced duodenal bicarbonate secretion in rats. Dig Dis Sci 2002; 47: 2116-2124. 23. Yao B, Hogan DL, Bukhave K, Koss MA, Idenberg JL. Bicarbonate transport by rabbit duodenum in vitro: effect of vasoactive intestinal polypeptide, prostaglandin E2, and cyclic adenosine monophosphate. Gastroenterology 1993; 104: 732-740. 24. Glad H, Ainsworth MA, Svendsen P, Fahrenkrug J, Schaffalitzky de Muckadell OB. Effect of vasoactive intestinal peptide and pituitary adenylat cyclase-activating polypeptide on pancreatic, hepatic and duodenal mucosal bicarbonate secretion in the pig. Digestion 2003; 67: 56-66. 25. Sjoblom M, Felmstrom G. Melatonin in the duodenal lumen is a potent stimulant of mucosal bicarbonate secretion. J Pineal Res 2003; 34: 288-293. 26. Jarbur K, Dalenback J, Sjovall H. Quantitative assessment of motility-associated changes in gastric and duodenal luminal pH in humans. Scand J Gastroenterol 2003; 38: 392-298. 27. Hoogerwerf WA, Tsao SC, Devuyst O, et al. NHE2 and NHE# are human and rabbit intestinal brush-border proteins. Am J Physiol Gastrointest Liver Physiol 1996; 270: G29-41. 28. Hogan DL, Crombie DL, Isenberg JI, et al. Acid-stimulated duodenal bicarbonate secretion involves a CFTR-mediated transport pathway in mice. Gastroenterology 1997;113: 533-541. 17 29. Tsumura T, Hazama A, Miyoshi T, Ueda S, Okada Y. Activation of cAMP-dependent Cl - currents in guinea-pig paneth cells without relevant evidence for CFTR expression. J Physiol (Lond) 1998; 512: 765-777. 30. Praetorius J, Hager H, Nielsen S, et al. Molecular and functional evidence for electrogenic and electroneutral Na -HCO3 cotransporters in murine duodenum. Am J Physiol Gastrointest Liver + Physiol. 2001; 280: G332-343. 31. Kaunitz JD, Akiba Y. Luminal acid elicits a protective duodenal mucosal response. Keio J Med 2002; 51: 29-35. 32. Fandriks L, Bothmer C, Johansson C, Holm M, Bolin I. Water extract of Helicobacter pylori inhibits duodenal mucosal alkaline secretion in anesthetized rats. Gastroenterology 1997; 113: 1570-1575. R e c e i v e d : 27 March 2004 A c c e p t e d : 28 May 2004 Author's address: Prof. Stanislaw J. Konturek, M.D., Department of Physiology Jagiellonian University Medical College 16, Grzegorzecka St., 31-531 Krakow, Poland tel. (+48-12) 4211006 fax (+48-12) 4211578 E-mail: mpkontur@cyf-kr.edu.pl