Challenge M123-5 CMPT Clinical Bacteriology Program
advertisement

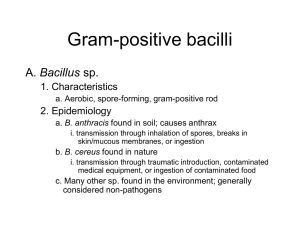
CMPT Clinical Bacteriology Program Innovation, Education, Quality Assessment, Continual Improvement www.cmpt.ca November 2012 201 2 Challenge M123-5 Bone Swab: Co rynebacte rium amyco latum HISTORY MAIN EDUCATIONAL POINTS for M123-5 This challenge, sent to category A laboratories, was a simulated bone swab sample obtained from a 58 year old female diabetic patient with osteomyelitis of the big toe. 1. Identify the potential significance of Corynebacterium species in a normally sterile specimen. Participants were expected to isolate and report Corynebacterium amycolatum or Corynebacterium species and to perform and report results of antimicrobial susceptibility testing for appropriate antibiotics. CMPT QA CMPT control yielded a pure growth of Corynebacterium amycolatum for 9 days. SURVEY RESULTS This survey achieved consensus for identification to the genus level of Corynebacterium species and is suitable for grading for the identification component. The reporting of antimicrobial susceptibility testing did not reach consensus and, therefore, was not graded. Reference Laboratories: Identification Component. Eight laboratories reported C. amycolatum, 5 laboratories reported Corynebacterium species ± refer or Coryne- 2. Identify the need for full identification and susceptibility testing of Corynebacterium species in a normally sterile specimen. 3. Identify the significance of organisms that may normally be considered of low pathogenicity in the pathogenesis of diabetic foot infections. bacterium xerosis (correct to genus 12/14, 86%), 1 laboratory reported diphtheroids/ Corynebacterium as usual skin flora, and 1 laboratory did not submit a report. This component was considered suitable for grading. Antimicrobial Susceptibility Component. Eleven of 14 (79%) laboratories reported results of antimicrobial susceptibility testing for penicillin and vancomycin. All laboratories submitting susceptibility results reported the isolate as susceptible to both of these agents. Grading Maximum grade: 4 Reporting Corynebacterium amycolatum was graded 4. Reporting Corynebacterium species was graded 4. Reporting the wrong species identification was downgraded to 3. 2 laboratories that did not perform susceptibility testing and one laboratory reported skin flora. Consensus was not reached for susceptibility testing and, therefore, was not graded. Laboratories that provided gram stain reaction only with suggestive morphology received a grade of 3. Participating Laboratories Suggesting the isolate was normal flora was graded 0. Table 1. Identification results and grades assigned Reported results Corynebacterium amycolatum (25), Corynebacterium striatum/ amycolatum (4) Corynebacterium species, +refer (2 added “not C. diphtheriae ± not C.jeikeium”) Corynebacterium xerosis gram positive bacilli, resembling Corynebacterium species/coryneform bacteria, diphtheroid – like, refer diphtheroid/Corynebacterium species and called usual skin flora as per Director Corynebacterium amycolatum and Klebsiella pneumoniae Total Grade 29 4 26 4 1 3 12 3 1 0 1 0 mixed bacteria 1 0 no growth after 4 days, snnp 1 0 no report submitted / results submitted after due date 3 0 specimen not normally processed 7 ungraded Total 82 Reporting other organism in addition to the C. amycolatum was graded 0. Not reporting results, reporting past the due date or using the wrong identifiers was graded 0. Page 1 Copyright CMPT 2012 CMPT Clinical Bacteriology Program November 2012 201 2 M 123123 - 5 Identification Component. Component Reported identifications from participating laboratories are detailed in Table 1. “diphtheroid” refers to the gram stain similarity of these organisms to the most well-recognized pathogen in the group, C. diphtheriae. Twenty-nine laboratories identified the isolate to species level as C. amycolatum or C. striatum/amycolatum, 63/82 (77%) of laboratories identified the isolate to genus level as Corynebacterium species, as C. xerosis, or as some variation of “gram-positive bacilli resembling diphtheroids”, all of which indicated the isolate would be referred for further identification. Two laboratories in this latter group added the Corynebacterium isolated was not C. diphtheriae. The 19 remaining laboratories reported a variety of results as seen in Table 1. Recent advances in molecular techniques have led to many taxonomic changes in this group, and many organisms formerly known as Corynebacterium species are now classified in many other genera such as Turicella, Arthrobacter, Brevibacterium, Dermabacter and others, in addition to the Corynebacterium genus. One laboratory reported “mixed bacteria”, and 1 laboratory reported C. amycolatum and Klebsiella pneumoniae. These results indicate contamination of the specimen at the point of processing and these laboratories should review their procedures for sterile technique. Susceptibility Testing Component. Tables 2 and 3 provide the details of the reports of antimicrobial susceptibility testing. All those labs reporting results indicated that the isolate was susceptible to both penicillin/amoxicillin and vancomycin. This component is ungraded since consensus was not obtained. The tables are for information purposes only. TAXONOMY The genus Corynebacterium is a diverse and large group of microorganisms comprised of irregularly shaped small gram positive bacilli that do not form spores, which are commonly referred to as “coryneform” bacteria or “diphtheroids”. Coryneform refers to the “club-shaped” morphology seen on Gram stain, and the term Table 2. Susceptibility results - Penicillin Reported results There are over 80 species in the genus Corynebacterium, 50 of which are of clinical importance.1 ISOLATION AND IDENTIFICATION The very typical club-shaped morphology on Gram stain is only exhibited by true Corynebacterium species. Microscopically the organisms are small gram positive, slightly curved, rods without spores and with slightly wider ends, which gives the club shaped appearance. Bacteria can appear as single cells, in pairs or palisading or as the so-called Chinese letter appearance. Coryneform bacteria are not fastidious, do not require special collection or transport conditions and will readily grow on 5% sheep blood agar-based media. If deemed necessary, selective media are available for the recovery from specimens that may have mixed normal flora. Most will grow readily at 37ºC and will grow best in a CO2 enriched atmosphere. Growth is generally visible within 48 hours. When growth is examined in culture, colony morphology, size, pigment, and hemolysis surrounding colonies can be helpful criteria leading to the identification of coryneform bacteria. Characteristics of this group are too large and varied to discuss in great detail in this survey. Clinically relevant Corynebacterium species are catalase positive, non-motile, and include both Table 3. Susceptibility results - Vancomycin Total Reported results Total Susceptible 37 Susceptible 35 Amoxicillin Susceptible 1 Reported past due date 1 No report 1 no report 1 Reported past due date 1 n/a, refer, snnp 45 n/a, refer, snnp 42 Total 82 Total 82 Page 2 Copyright CMPT 2012 CMPT Clinical Bacteriology Program November 2012 201 2 M 123123 - 5 fermenters and non-fermenters. Most identification schema follow the outline of von Graevenitz and Funke based on catalase, fermentation or oxidation, motility, nitrate reduction, urea hydrolysis, esculin hydrolysis, acid production from certain sugars, the CAMP reaction and lipophilia.1 Commercial systems for identification and speciation of Corynebacterium species are used widely, but the results of these systems should be correlated with simple basic characteristics such as gram stain and culture morphology and often require supplemental tests. C. amycolatum colonies are 1-2 mm in diameter after 24 hours incubation and are typically dry, waxy, and grayish white with irregular edges.1 The strains demonstrate wide variability in biochemical testing and can be misidentified due to overlap with the reactions of other organisms. Biochemically similar species include C. xerosis, C. striatum, and C. minitissimum. In this challenge, 4 laboratories reported C. striatum/ amycolatum. These two species have different colony morphologies: C. striatum is creamy and moist, while C. amycolatum is dry and waxy. One laboratory identified the isolate as C. xerosis, which will grow at 20ºC while C. amycolatum will not. Definitive identification relies on 16S rDNA sequencing. There is limited data on the use of the MALDI-TOF for the identification of this group. ANTIMICROBIAL SUSCEPTIBILITY CLSI document M45-A2 “Methods for Antimicrobial Dilution and Disk Susceptibility Testing of Infrequently Isolated or Fastidious Bacteria” recommends penicillin, vancomycin, erythromycin and gentamicin for primary testing of Corynebacterium species.2 Broth microdilution is the recommended method when testing is warranted, often requiring blood supplemented media to ensure adequate growth. Standardized MIC interpretative criteria for Corynebacterium species is also provided in this document. Disk diffusion methods such as Kirby-Bauer are not standardized and CLSI guidelines do not give breakpoints for interpretation of disk diffusion methods. E-test methodology has been reported in the literature to provide MIC results comparable to those of broth dilution methods.3 Laboratories using Kirby-Bauer testing should review their protocols to insure that MIC-based methods are used or refer isolates to a reference laboratory for reliable results. Antibiotic susceptibility pattern of Corynebacterium species is not predictable and isolates from normally sterile sites should be tested. Penicillin resistance is now common, and variable patterns of susceptibility are seen with erythromycin, clindamycin, tetracycline and ciprofloxacin. The susceptibility of isolates to vancomycin is predictable and this should be the drug of choice until susceptibility patterns are known. Corynebacterium species are also usually susceptible to linezolid. Speciation and determination of antibiotic susceptibility patterns should be performed from sterile sites as some species (C. jeikeium, C. urealyticum, and C. amycolatum) may be resistant to many of the commonly used antibiotics including β-lactams, macrolides, and fluoroquinolones. 4,5 CLINICAL RELEVANCE Corynebacterium species are part of the normal flora, primarily of the skin and mucous membranes. With the exception of C. diphtheriae, they are low virulence pathogens. However, they can be associated with a variety of infections, particularly in patients whose defences are compromised, either by disease, breaks in barrier defenses, lowered immune status, or medical interventions such as vascular access lines or prosthetic devices. Probably one of the hardest things to do in the laboratory is to determine the clinical significance of coryneform bacteria isolated from clinical specimens. The clinical relevance of isolating these organisms in culture is strengthened when multiple specimens are positive for the same Corynebacterium species and when coryneform bacteria are seen in direct Gram stains. 1,6 Further, coryneform bacteria warrant full identification if they are isolated from normally sterile body sites from adequately collected specimens if they are the predominant organisms. When isolated from non-sterile sites with other normal flora in similar quantities, coryneform bacteria should be reported as normal flora. Page 3 Copyright CMPT 2012 CMPT Clinical Bacteriology Program November 2012 201 2 M 123123 - 5 The patient history given in this survey indicated that the patient had diabetes and an osteomyelitis of the big toe. Most of these infections are poly-microbial with the most common organisms being gram positive cocci, particularly staphylococci. The Infectious Diseases Society of America (IDSA) has recently published guidelines on diabetic foot infections.8 It is recommended that physicians include the possibility of osteomyelitis in the presence of infected, deep, or extensive foot ulcers particularly if they overlie a bony prominence. These experts believe that the most definitive way to diagnose diabetic foot osteomyelitis is by both bone culture and histopathology. An appropriately collected bone sample, taking steps to minimize contamination from potentially infected surrounding soft tissue, should be sent for culture. A bone sample for culture and histopathology is warranted when the diagnosis is not certain despite other investigations and cultures from tissue specimens are not definitive. C. amycolatum is part of the normal human skin flora and is the most frequently encountered Corynebacterium species in human clinical material. 1 This organism has been reported in association with a wide variety of infections including wounds, prosthetic and catheterassociated blood stream infections, urinary tract infections, pneumonia, bacteremia and endocarditis. 4,7 REFERENCES 1. Funke G, Bernard K. A. Coryneform grampositive rods. In: Versalovic ea, ed. Manual of Clinical Microbiology. Vol 1. 10th ed. ed. Washington, DC.: ASM; 2011:413. 2. Clinical Laboratory Standards Institute. Methods for Antimicrobial Dilution and Disk susceptibility Testing of Infrequently Isolated or Fastidious Bacteria; Approved GuidelineSecond Edition. Wayne, PA.: CLSI; 2010;30: M45-A2 CLSI Wayne, PA. 3. Martinez-Martinez L, Ortega MC, Suarez AI. Comparison of Etest with broth microdilution and disk diffusion for susceptibility testing of coryneform bacteria. J Clin Microbiol 1995;33:1318-1321. 4. Reddy BS, Chaudhury A, Kalawat U, Jayaprada R, Reddy G, Ramana BV. Isolation, speciation, and antibiogram of clinically relevant non-diphtherial Corynebacteria (Diphtheroids). Indian J Med Microbiol. 2012;30:52-57. 5. Funke G, Punter V, vonGraevenitz A. Antimicrobial susceptibility patterns of some recently established corynefrom bacteria. Antimicrob Agents Chemother 1996;40:2874-2878. 6. Bernard K. The Genus Corynebacterium and Other Medically Relevant Coryneform-Like Bacteria. J Clin Microbiol. 2012;50:31523158. 7. Coyle MB, Lipsky BA. Coryneform bacteria in infectious diseases: clinical and laboratoryoratory aspects. Clin Microbiol Rev. 1990;3:227 -246. 8. Lipsky BA, Berendt AR, Cornia PB, Pile JC, Peters EJG, et al. 2012 Infectious Diseases Society of America Clinical Practice Guideline for the Diagnosis and Treatment of Diabetic Foot Infections. Clin Infect Dis 2012;54:132173. Page 4 Copyright CMPT 2012