Document

( (
مﯾﺣرﻟا نﻣﺣرﻟا ﷲ مﺳﺑ
) )
Members of the Scientific Council of Arab Board of Family Medicine /Iraq:
Dr. Ban Abdul RidhaAl-Hashimi (Chairman)
Dr. Ali Abdul Ridha Abutaheen (Co-Chairman)
Assistant Professor Dr. Wafaa faiq Tawfeeq (Member)
Assistant Professor Dr. Maral fathalla Thabit ( Member)
Dr. Lujain Anwar Alkhazrajy (Member)
A C K N O W L E D G M E N T
First we praise Allah for assisting us in completing this work.
The Scientific Council of Arab Board of Family Medicine would like to express a deep gratitude to the Higher Committee of the Arab board of Medical Specializations and it
’ s Council for their great support, in establishing and maintenance of our council.
The council Department would like to show an ultimate thankfulness to :
Dr. Hani Musa Bader ,the vise president of the higher committee of the Arab board of Medical Specializations.
Dr.Safaa Kadhum Diaa, The council of the higher committee of the Arab board of
Medical Specializations.
For their scientific & administrative support for the council.
For their academic experiences that reinforced the council.
Also we would like to express our great appreciation to Professor Dr.Thamir
Khadum yousif for his precious advices in writing this curriculum.
Special thanks to the pioneers:
Professor Dr. Amjad Niazi
Professor Dr. Abd alhussein Alhadi
Assistant Professor Dr.Abdul munim Aldabagh
Deepest respect and appreciation to the following supervisors specialists family physicians for their great effort in establishing this curriculum and their enthusiasm in supervising and training the residents involved in our program:
Dr. Hassan Hadi Bakir Dr. Wafaa faiq Tawfeeq
Dr. Ban Abdul Ridha Al-Hashimi Dr. Maral fathalla Thabit
Dr. Raed Ghanim Matti Dr. Jamal Rasheed Abdul Hameed
Dr. Sahar Abdul Hassan Dr. Sundus Shawqi Ibrahim
Dr. Manal Ibrahim Muslim. Dr. Ali Abdul Ridah Abutaheen
Dr.Zena Adnan Kaduhum Dr.Sanaa Jafar Alkaisi
Dr. Wasan Jasim Mohammed Dr. Ban Jumaa Abd
Sincere respect for the managers of the training centers established in Ninavah(Mousil) &
Basrah governorates for their help to complete the family medicine training programme.
Last but not least our great appreciation to the secretary council Miss Noor Saheb For her fine commitment with her duty and for making life easier in the council department.
Dr.Lujain Anwar Alkhazrajy
Member of Scientific Council of Arab Board
Of Family Medicine
TABLE OF CONTENTS
NO. SUBJECT
12
13
14
15
8
9
10
11
4
5
6
7
1
2
3
INTRODUCTON
DOMAINS OF TRAINING 0F FAMILY MEDICINE
SPECIALITY ADMISSION REQUIREMETS
STRUCTURE OF THE PROGRAM
PARTICIPATING TRAINING CENTERS
TYPES OF TRAINING ROTATIONS
1-THEOROTICAL TRAINING ROTATIONS
2- CLINICAL TRAINING ROTATIONS
THE CONTENT OF THE CLINICAL ROTATIONS
INTERNAL MEDICINE ROTATION
EMERGENCY ROTATION
GENERAL SURGERY ROTATION
ORTHOPEDIC ROTATION
PEDIATRIC ROTATION
OBSTETRICS & GYNECOLOGY ROTATION
20
21
22
23
16
17
18
19
PSYCHIATRY ROTATION
E.N.T. (OTOLARYNGOLOGY) ROTATION
DERMATOLOGY ROTATION
OPHTHALMOLOGY ROTATION
LABORATOTY MEDICINE ROTATION
DIAGNOSTIC RADIOLOGY ROTATION
ELECTIVES ROTATION
3. PHC CENTER TRAINING CURRICULUM
24
25
IN-TRAINING EVALUATION OF THE RESIDENTS
LEARNING SITUATIONS
26 REQUIREMENTS TO FILFULL THE RESIDENCY TRANING
PROGRAM
27 ADMINSTRATIVE INSTRUCTIONS OF THE RESIDENCY TRANING
PROGRAM
28 ADMINSTRATIVE WARNINGS OF THE RESIDENCY TRANING
PROGRAM
29 DISCONTINUATION OF THE RESIDENCY TRANING PROGRAM
30 APPENDICES
PAGE
NO.
58
60
61
62
50
52
54
56
69
72
73
1
3
3
4
11
13
13
41
43
44
48
23
25
36
40
75
75
76
77
INTRODUCTION
Family Medicine is a very broad-based specialty provides initial, continuing comprehensive and coordinated care for individuals, families and communities. It integrates current biomedical, psychological and social understanding of health in caring for patient using a holistic approach with a great attention to prevention.
The specialty considers an individual as a unit of the community. It takes care of individuals from infancy to the end of life. The family physician plays an important role in promoting health of individuals and communities besides taking care of sickness and disease. Over a period, it has become a major specialty.
The Family Medicine Residency Training Program is committed to develop it to its maximum potential and has designed this program taking into consideration local and international developments.
The family physician is required to understand the principles of Family Medicine, acquire clinical knowledge and skills that will help him/her to practice as an effective family physician in an ideal setting. He/she also needs to develop a person-centered approach oriented to the individual, his/her family and their community. This requires a unique consultation process which establishes a relationship through effective communication process.
MISSION
To graduate caring, competent and collaborative family physicians who are well oriented to the problems and needs of the community in Iraq& are skilled in principle of practice of family medicine. .
VISION
Our program will achieve excellence in training future family physicians with the skills, values and attitudes to practice high quality Family Medicine.
OBJECTIVES
At the end of the training program the physician should:
1) Be able to clinically identify & manage all the medical problems presented by the patients in health center& hospital.
2) Be able to provide effective comprehensive and continuing primary and preventive care to all individuals with respect to the family unit, and meet their needs and fulfill their expectations irrespective of age, sex, or diseased organ.
3) Show the ability of social and environmental factors of families in promoting health and managing.
4) Diagnose and manage medical conditions commonly encountered in primary care and having the ability for priortarizing them.
5) Deal in a balanced way with physical, psychological and social problems of patients.
6) Identify deficits in the environment when the patient is in living or working.
7) Demonstrate the ability to:
•
Use consultation with other medical specialists effectively.
•
Identify & use available community recourses as an integral part of the health care system.
•
Apply the principles and practice of health service planning, organization, administration and evaluation.
8) Be able to build a satisfying physician-patient relationship. Including:
•
Problem identification.
•
Problem solving.
•
Compliance.
•
Patients ’ education.
9) Be able to plan, understand, and evaluate research programs in the area of family medicine and to apply its result to one ’ s medical practice.
10) Teach and learn effectively from colleagues, patients, families and community.
Training in Family Medicine will concentrate on the following domains:
•
Communication skills and doctor-patient relationship.
•
Applied clinical practice.
•
Organizational and management skills.
•
Professional growth, attitudes and ethics.
•
Epidemiology and health of the population.
•
Improvement of health care performance.
DOMAINS OF TRAINING OF FAMILY MEDICINE
SPECIALITY ADMISSION REQUIREMETS
1. Resident must fulfill an ITP- TOFEL examination (of a score of at least 480 degrees) & a basic course of computer sciences from one of the governmental Iraqi universities.
2. Resident must be a holder of Bachelors Degree in Medicine & Surgery.
3. Resident must have completed at least two year of internship.
4. Resident must be of good conduct and medically fit for the specialty.
5. Resident must provide three letters of recommendation from three consultants with whom he/she has worked confirming his/her ability and capability of training.
6. Resident must submit a letter of approval from his/her sponsor confirming permission to join the Specialty Training Program on full time basis for the entire period of training.
7. Resident must submit a competitive examination in family medicine (the bulk of this examination is 70% of the total competitive score).
8. Permanency in family medicine (of at least one year duration or more) has a bulk of 3% of the total score.
9. The degree of Bachelors (which is approved by a written certificate of graduation submitted to the council) & the serial number of graduation have a bulk of 30% of the total competitive score (by a special equation) .
10. Resident must pass the specific interview of the council of family medicine.
STRUCTURE OF THE PROGRAM
1DURATION OF THE PROGRAM :
The Family Medicine training program is a 4-years program.
2CORE STRUCTURE OF FOUR YEARS ROTATION:
Month
Year
1 2 3 4 5 6 7 8 9 10
١ st
year
Introductory Lectures & courses to Family Medicine
Internal Medicine(5days/wk)
11 12
Surgery(5days/wk)
٢ nd
year
Gynecology&
Obstetrics(5days/wk)
+PHC center (1day/wk)
Pediatrics(5days/wk) Psychiatry(5day s/wk)
Ophthalmology
(5days/wk)
+PHC center (1day/wk)
٣ rd
year Introductory
Lectures & courses to Community Medicine
ENT
(Otolaryngology)
Dermatology Diagnostic radiology
Laboratory
Medicine
Complementary course
Electives course
٤ th year PHC center (5days/wk) Vacation Final exam
*Please note that these rotations do not necessarily follow the sequence shown in the table.
3 OUTLINES OF ALL THEOROTICAL ROTATIONS:
SUBJECT
Introductory Lectures & courses to Family
Medicine
Introductory Lectures & courses to
Community Medicine
No.OF MONTHS
2 MONTHS
2 MONTHS
TOTAL
4-OUTLINES OF ALL CLINICAL ROTATIONS:
SUBJECT
MAJOR CLINICAL ROTATIONS
INTERNAL MEDICINE
GENERAL SURGERY
OBSTETRICS & GYNECOLOGY
PEDIATRICS
MINOR CLINICAL ROTATIONS
PSYCHIATRY
OPHTHALMOLOGY
E.N.T. (OTOLARYNGOLOGY)
DERMATOLOGY
DIAGNOSTIC RADIOLOGY
LABORATORY MEDICINE
ELECTIVES
COMPLEMENTARY COURSE
TOTAL
6MONTS
No. OF MONTHS
6MONTS
4MONTS
4MONTS
4MONTS
2 MONTHS
2 MONTHS
2 MONTHS
2 MONTHS
1 MONTH
1 MONTH
2 MONTHS
2 MONTHS
32 M0NTHS
5OUTLINES OF INTERNAL MEDICINE ROTATION:
SUBJECT No. OF WEEKS
GENERAL MEDICINE
NEPHROLOGY
EMERGENCY MEDICINE
ENDOCRINE CLINIC
CCU
RESPIRATORY CLINIC
RHEUMATOLOGY CLINIC
NEUROLOGY
HEMATOLOGY
ENDOSCOPY CLINIC
GIT
TOTAL
4
4
2
1
1
6 M0NTHS
2
1
2
3
2
2
6 OUTLINE OF SURGERY ROTATION:
SUBJECT
GENERAL SURGERY
UROSURGERY
GIT
EARLY DIAGNOSIS OF BREAST DISEASES
No. OF WEEKS
3
2
2
2
ORTHOPEDIC
SURGICAL EMERGENY UNIT
MINOR SURGERIES
TOTAL
4
2
1
4 M0NTHS
7OUTLINES OF GYNECOLOGY & OBESTETRICS ROTATION:
SUBJECT
OBESTETRIC CLINIC
INFERTILITY CLINIC
FAMILY PLANING CLINIC
LABOR ROOM
PHC(ANC)
TOTAL
DAY/WEEKS (FOR4 MONTHES)
1
1
1
1
1
5 DAYS /WEEKS (FOR 4 MONTHES)
8OUTLINE OF PEDIATRICS ROTATION:
SUBJECT
NEONATE WORD
ENDOCRINE CLINIC
BLOOD DISEASES CLINIC
PSYCHIATRIC CLINIC
PEDIATRIC SURGERY
COMMUNICABLE DISEASES CLINIC
NUTRITION CLINIC
HANDICAP CLINIC
CHRONIC DISEASES CLINIC
PEDIATRIC SURGERY EMERGENCY CLINIC
PEDIATRIC MEDICAL EMERGENCY CLINIC
TOTAL
2
1
1
2
1
3
1
1
2
1
1
4 MONTHES
9- OUTLINES OF LABORATORY MEDICINE ROTATION:
SUBJECT No. OF DAYS
BACTERIOLOGY 5
No. OF WEEKS
PARASITOLOGY
HEAMATOLOGY
CHEMISTRY
SEROLOGY
BLOOD BANK
TOTAL
2
3
5
3
2
One Month (30 days)
10- OUTLINES OF ELECTIVES ROTATION :
( TOTAL DURATION OF THIS ROTATION IS TWO MONTHS)
SUBJECT
NUTRITION
HEALTH EDUCATION
PHYSIOTHERAPY
REHABIITATION
PSYCHOTHERAPY
COMMUNAL PSYCHOTHERAPY
MENTAL HEALTH OF CHILDREN
SPORT MEDICINE
SCHOOL HEALTH
ADOLESENT HEALTH CARE
TRAVELERS HEALTH
OCCUPATIONAL MEDICINE
ANTENATAL CARE
PERIODIC PAEDIATRIC EXAMINATION
NON COMMUNICABLE DISEASES
ENDEMIC DISEASES
DIABETICS CARE
GERIATRICS CARE
HOME CARE
MEDICAL VISIT
CARE OF HANDICAPED
EVALUATIONS
Year
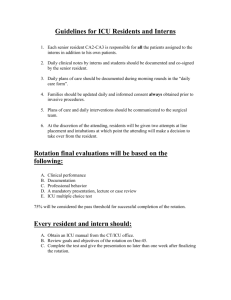
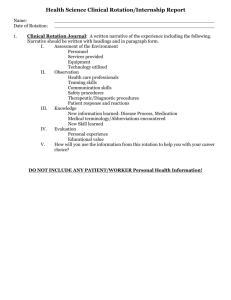
IN-TRAINING EVALUATIONS (BEFORE FINAL EXAMINATION)
OUTLINES
END THEOROTICAL
COURSES EVALUATIONS
(THE SUCCESS IN EACH ONE
IS ≥ 60%)
END CLINICAL COURSES EVALUATIONS
(THE SUCCESS IN EACH ONE IS ≥ 60%)
PHC CENTER
EVALUATION TOTAL
(20%)
١ st
Year
10%
Introductory Lectures & courses to Family Medicine
( with 3trials)
MCQ
50% short answer questions50%
Internal Medicine
( with 3trials)
OSCE
50%
MCQ
40%
EVALUATON
FORM
10%
OSCE
50%
General Surgery
( with 3trials)
MCQ
40%
EVALUATON
FORM
10%
EVALUATON
FORM
100%
٢ nd
year
20%
٣ rd.
year
30%
GYNECOLOGY & OBESTETRICS
( with 3trials)
PEDIATRICS
( with 3trials)
EVALUATON
FORM 100%
OSCE
50%
MCQ
40%
EVALUATON
FORM
10%
OSCE
50%
MCQ
40%
EVALUATON
FORM
10%
Introductory Lectures & courses
MCQ
50%
3trials) short answer questions50%
END MINOR CLINICAL COURSES EVALUATIONS( with 3trials) EVALUATON
OSCE
50%
MCQ
40%
EVALUATON
FORM
10%
FORM
100%
4th Year
40%
Doing a research
(Dissertation)
10%
Preparatory exam( with 2trials) 60%
MCQ short answer questions
(Clinical problems)
OSCE Oral exam
LOG BOOK
10%
EVALUATON
FORM 100%
TOTAL SCORE
=20%
FOR THE
TOTAL 4
YEARS
NOTE
: -MCQ: multiple choice questions.
- OSCE: Objective Structured Clinical Examination.
PARTICIPATING TRAINING CENTERS
1THE TRAINING HOSPITALS:
HOSPITALS TYPE
Baghdad Teaching Hospital
Specialized Surgeries Teaching
Hospital
General Hospital
Surgical Hospital
Child welfare Teaching
Hospital
Pediatric Hospital
Alkadymia Teaching Hospital General Hospital
Child Central Teaching Pediatric Hospital
Hospital
Alalwya Teaching Hospital
Ibnsina Teaching Hospital
Obstetrics &Gynecology
Hospital
General Hospital
Aljamhori Teaching Hospital Surgical Hospital
Albatool Teaching Hospital Obstetrics& Gynecology
Hospital
Alsalam Teaching Hospital General Hospital
Alkhansaa Teaching Hospital Pediatric Hospital
ADRESS
Baghdad
Baghdad
Baghdad
Baghdad
Baghdad
Baghdad
Ninavah
Ninavah
Ninavah
Ninavah
Ninavah
Rizkari General Teaching
Hospital
Raparin Teaching Hospital
Albasrah Hospital
Albasrah Teaching Hospital
General Hospital
Pediatric Hospital
General Hospital
Obstetrics , Gynecology&
Pediatric Hospital
General Hospital
Erbil
Erbil
Albasrah
Albasrah
Alshefaa Teaching Hospital Albasrah
Alsader Teaching Hospital
Alfayhaa Teaching Hospital
General Hospital
General Hospital
Albasrah
Albasrah
3THE FAMILY MEDICINE SPECIALIZED TRAINING HEALTH CARE
CENTERS:
HEALTH CENTERS ADRESS
Aldhubbat Family medicine specialized training PHC center
Almustansyria Family medicine specialized training PHC center
Bab Almuadam Family medicine specialized training PHC center
Alsulakh Family medicine specialized training PHC center
Aladhamya Althalith Family medicine specialized training
PHC center
Kadum Abdnabi Family medicine specialized training PHC center
Baghdad\Alrusafa
Baghdad\Alrusafa
Baghdad\Alrusafa
Baghdad\Alrusafa
Baghdad\Alrusafa
Baghdad\Alrusafa
Alsalam Family medicine specialized training PHC center
Alsalam alsekani Family medicine specialized training PHC center
Alshabab Family medicine specialized training PHC center
Baghdad\Alkarkh
Baghdad\Alkarkh
Baghdad\Alkarkh
Almansor Family medicine specialized training PHC center Baghdad\Alkarkh
Aladel Family medicine specialized training PHC center Baghdad\Alkarkh
Alzahraa Family medicine specialized training PHC center
Aldakhelya Family medicine specialized training PHC
Baghdad\Alkarkh
Baghdad\Alkarkh center
Alhabna Family medicine specialized training PHC center Baghdad\Alkarkh
Alqudis Family medicine specialized training PHC center
Alarabi Family medicine specialized training PHC center
Alhadbaa Family medicine specialized training PHC center
Tamooz Family medicine specialized training PHC center
Barayati Family medicine specialized training PHC center
Alabasya Family medicine specialized training PHC center
Albasrah Family medicine specialized training PHC center
Almuhandeseen Family medicine specialized training PHC center
Alakeel Family medicine specialized training PHC center
Alrazi Family medicine specialized training PHC center
Ezaldeen Saleem Family medicine specialized training PHC center
Ninavah
Ninavah
Ninavah
Ninavah
Erbil
Karbalaa
Albasrah
Albasrah
Albasrah
Albasrah
Albasrah
TYPES OF TRAINING ROTATIONS
1THEOROTICAL TRAINING ROTATIONS:
Introductory Lectures &training courses to Family Medicine (at the 1 st
2months of the 1 st
year) & to Community Medicine (at the 1 st
2months of the 3 rd
year) presented by specialists Family &Community Medicine physicians It would seem both appropriate and necessary at the Family Medicine Program that residents experience an intensive course focused on the concept and elements of Primary Health Care, Family Medicine and
Community Medicine.
Objectives of these introductory Lectures &training courses are:
At the end of rotation, the resident will be able to:
1. Recognize the basic family practice theories, principles and skills
2. Identify and understand national programs related to Primary Health Care
3. Understand family and community dynamics
Process of Training:
The residents will participate in the preparation of the topics and discussing it with tutors.
Learning situation:
. Lectures/seminars
•
Presentation
•
Small group discussion
•
Self-directed learning
•
Clinical practice :
. Active Learning.
. Peer Review.
. Role-play.
. Audit.
. Video-recording and feedback.
There is a written paper at end of each one of courses with score of success of 60% or more. This exam consists of multiple choice questions (MCQ) & short answer questions.
1.
INTRODUCTION TO FAMILY MEDICINE:
The curriculum is inform of theoretical lectures during 2 months period at the beginning of first year of the program
DAY
SUNDAY
MONDAY
TUESDAY
WEDNESDAY
THURESDAY
9-11 am 11-1 pm
Subjects included in theory
•
Concept of family medicine, definition of family medicine and its history
Introduction to the residency program, its history, development, content and requirements.
•
Documentation: SOAP, electronic medical records ,International classification of diseases (ICD) &training skills on The family records.
•
The future of family medicine& the future career of the residents.
•
Concept of Primary Health Care.
•
Primary health care elements & programs overview: e.g. Integrated management of childhood illnesses (IMCI), DM, EYE, EAR, HIV, TB, school health, etc.
•
Referral system.
•
Follow up system.
•
Counseling& communication skills.
•
Consultation modules.
•
Concept of health.
•
Concept of disease.
•
Natural history of the disease.
•
Concept of disease prevention.
•
Infection prevention& control.
•
Introduction to Medical Ethics.
•
Doctor
– patient relationship.
•
Family structure, lifecycles and dynamics.
•
The role of family medicine in illness care.
•
Health education.
•
Strategic planning.
•
Leadership.
•
The role of family in health promotion.
•
The relevance of medical history to family medicine.
•
Problem solving in family medicine & team building.
•
Ethics in family medicine.
•
The family physician (Five stars doctor)
•
Clinical decision making.
•
Integrative medicine.
•
How to break a bad news.
•
Palliative care.
•
Home care.
•
Cultural competence.
•
Managing multiple morbidities.
•
Bioterrorism.
•
Quality improvement.
•
Evidence based medicine (EBM).
•
Preschool vision screening program.
•
Child abuse.
•
Domestic violence.
•
Mental Health.
•
Behavioral Health: Smoking, Alcoholism, Drug abuse &Eating Disorder.
•
Assessment of risks for abuse, neglect, and family and community violence.
•
Health maintenance for adolescents.
•
Health maintenance for adult patients.
•
Health maintenance for older adults (Geriatric Medicine).
•
Polypharmacy and Drug Reactions.
•
General principles of control & prevention of non communicable diseases (NCD).
•
Communicable disease program &Reportable communicable disease
•
AIDS program
•
Population epidemiology, and the interpretation of public health statistical information
•
Community-based disease screening, prevention, health promotion.
•
General principles of emergency medicine ، Trauma- Life Support, First Aids, Cardiac
Arrest& Acute &chronic poisoning
•
General principles of travel medicine
•
General principles of sport medicine
•
Occupational safety
•
•
Environmental health& Waste Disposal
Auditing
•
Clinical methodology
–
How to write a research.
Lists of Skills to be learned:
•
Consultation techniques
•
Documentation skills
•
Presentation skills
•
Health Information System skills
2. COMMUNITY MEDICINE CURRICULUM:
The curriculum is in form of theoretical lectures during 2 months period at the beginning of third year of the program as follows:
Sunday Infectious diseases
(24 hr)
Infectious diseases
= 3hr each section
Epidemiology of (NCD) ( 16 hr)
Monday Epidemiology
(20 hr)
+
(40 hr)
Biostatistics
(20 hr)
Tuesday
Wednesday
Primary Health Care (PHC)
(16 hr)
Administration
+
Occupational
(16 hr)
Sociology(4 hr)
+
Communication Skills
( 4 hr)
Environmental Health
( 8 hr)
Evaluating Medical Researches (10)
+
Evidence Based Medicine (EBM) (6 hr)
Nutrition (16 hr)
Note: Thursday of each week will be as training at the family medicine primary health care center.
1- Applied Epidemiology:
•
Introduction to Applied Epidemiology (Definition & Uses).
•
Screening& Surveillance in health system.
•
Investigation of Epidemic.
•
The Concept of Association and Causation.
•
Importance of Medical research.
•
How to Write a Scientific Paper.
•
Designing of Epidemiological Studies.
•
Cross-Sectional Study.
•
Case Control Study Case Control Study.
•
Cohort Study.
•
Interventional Study.
•
Controlling Chance, Bias, and Confounder in Medical Research.
•
Evaluating medical research.
•
Evidence based problem solving.
2- Primary Health Care :
•
Introduction to PHC.
•
Elements of PHC.
•
Maternal Health Care.
•
Family planning.
•
Child health care.
•
Immunization.
•
Control of Diarrheal Diseases (CDD).
•
Control of Acute Respiratory Infections (ARI).
•
Breast feeding.
•
School health services.
3- Epidemiology of Infectious Disease:
•
Introduction to infectious Diseases.
•
Agent and Environmental Factors in Causing Diseases.
•
Host factors in causing diseases.
•
Mode of disease transmission (chain of events).
•
General control and preventive measures in infectious diseases.
•
Tuberculosis control program in Iraq/NTP.
•
Infections Acquired Through Respiratory Tract.
•
Exanthematous Infection.
•
Throat Infection: Diphtheria & Mump.
•
Salmonellas.
•
Shigellosis.
•
Food Poisoning.
•
Amebic Dysentery.
•
Cholera.
•
Poliomyelitis.
•
Hepatitis Viruses (A&E) .
•
Hepatitis B Virus infection.
•
AIDS.
•
STIS.
•
Malaria.
•
Zoonotic infections, criteria, general preventive and control measures.
•
Leshmaniasis.
•
Rabies.
•
Helmenthetic infection.
•
Bilharziasis.
•
Nosocomial infections ,and travelers health.
•
Fever of Unknown Origin (FUO).
4-Epidemiology of Non Communicable Diseases (NCD)
•
Introduction to NCD.
•
Epidemiological Transition.
•
Cardiovascular Diseases.
•
Hypertension.
•
Coronary heart Disease.
•
Rheumatic heart disease.
•
Stroke.
•
DM.
•
Tumors.
•
Respiratory System.
•
Obesity.
•
Blindness.
•
Accidents and injuries.
5-Nutritional Diseases:
•
Introduction, anthropometric measures.
•
Food Constituents/macronutrient, micronutrient.
•
Food Constituents/ energy.
•
Feeding of Vulnerable Groups.
•
Disorder of malnutrition.
•
Nutrition in Specific Diseases.
•
Obesity & overweight.
6-Environmental and occupational health problems.
•
Introduction and common terms, workers.
•
Challenges of occupational disease in developing country.
•
Surveillance monitoring, screening, and prevention of occupational diseases.
•
Physical environment health risks.
•
Measures for health protection of workers.
•
Water pollution, purification, Quality-criteria and standards.
•
Air Pollution, monitoring of air pollution.
•
Food Sanitation.
•
Radiation hazards, radiation protection.
•
Global Environment.
7-Administration in Health System
•
Introduction.
•
Planning.
•
Man power, team working.
•
Evaluation.
•
Information
•
Organization.
8- Medical Sociology
•
Basic principles, Social context of medicine, social and behavioral science, concepts in sociology, Social determinates of diseases. Psychology, social psychology. Cultural factors in health and disease
•
Patient
–
Doctor Relationship
•
Social determinates of diseases (2 lectures)
•
Violence
•
Management of social problem
9- BIOSTATISTICS:
•
Importance of Biostatistics
•
Uses of biostatistics in medicine
•
Types of variables
•
Population and sample
•
Sampling methods
•
Organizing and displaying data
•
Measurement of central location (for grouped and raw data).
•
Measurement of dispersion (for grouped and raw data).
•
The concept of probability.
•
Probability distribution
•
Normal distribution.
•
Z test
•
T test
•
ANOVA test.
•
Chi square test
•
Estimation of Confidence interval
•
Hypothesis testing.
•
Correlation and regression.
•
Survival analysis
•
Nonparametric tests
•
Analysis of health data
2- CLINICAL TRAINING ROTATIONS:
A -GENERAL TRAINING OBJECTIVES OF CLINICAL TRAINING ROTATIONS:
1-Morning training:
2 days at consultant clinic,5days at the ward, and one day at a family medicine primary health center. Except for CCU were duties from 8am-6pm for 4 days & the fifth day at the PHC center.
The resident is committed to attend all the meeting held in hospital including:
Grand tour, Morning report, Death conference, in addition to attendance of
Journal Club after 12 pm in a certain day of the week that should be run by supervisors and trainers at the training center or at the hospital.
2-Evening training:
Word call twice a month, in addition to night consultant clinic twice / month & should be supervised by senior doctor, or progress stage resident.
B -SPECIFIC TRAINING OBJECTIVES OF CLINICAL TRAINING ROTATIONS:
At the clinical training rotation, each resident should:
A -Acquire the following skills:
1- Take complete history, perform and interpret diagnostic procedures commonly used in primary care.
2-Interpret commonly used laboratory tests.
3-Perform life saving procedures and investigations.
4-Demonstrate in cost effectively diagnose and manage of the common signs and symptoms.
5-Demonstrate fundamental knowledge of the management of the chronic conditions.
6- Diagnose and refer acute condition
7-Demonstrate ability to counsel health takers on different issues.
8-Acquire the diagnostic skills, therapeutics& counseling techniques.
THE CONTENT OF THE CLINICAL ROTATIONS:
1The common conditions &symptoms of each system as the following: During the family medicine clinical training rotation the residence should be able to diagnose, investigate and treat the common conditions as the following :
SYSTEM CONDITIONS , SIGNS & SYMTOMS
UNDIFFERETIATED
AND
CONSTITUTIONAL
SYMPTOMS
Evaluation of the following signs and symptoms:
•
Headache
•
Weight loss
•
Dizziness
•
Fever
• Syncope • Pelvic Pain • Chest pain • Smoking problems
• Abdominal Pain • Hoarseness • Cough • Weakness and Fatigue
CENTRAL
NERVOUS
SYSTEM
ENDOCRINE
SYSTEM
1.Diagnosis and treat the following conditions:
• Parkinson ’ s • Transient Ischemic Attacks (TIAs) • Dementia
• Cerebrovascular accident (CVA) • Bell ’ s Palsy • Seizures
Disorders • Trigeminal neuralgia • Migraines • Temporal arteritis
CARDIOVASCULAR
SYSTEM
2. Evaluation of the following signs and symptoms:
*Headache*presentation of sinusitis*Dizziness and vertigo
*Tremor *Seizures*Dementia *Coma*Paresis and paralysis
*Migraine and other Vascular Headache *Other Headaches*Facial nerve injury*Multiple sclerosis*Dementia.
1.Diagnosis and treat the following conditions:
• Coronary artery disease • Rheumatic fever*Heart failure
• Congestive heart failure (CHF) • Heart murmurs
• Valvular heart disease • Peripheral vascular disease
• Arrhythmias • Varicose veins
• Hypertension • Deep venous thrombosis (DVT)
• Thrombophlebitis
2. Evaluation of the following signs and symptoms:
*Chest pain *High blood pressure *Syncope *Leg edema*Irregular rhythm *Dysponea& generalized edema*Palpitation *Heart murmurs*Stable angina*Valvular Heart Diseases*Both congenital and Acquired Arrhythmias and Conduction disorders
1.Diagnosis and treat the following conditions:
•
Obesity
•
Gout
•
Diabetes mellitus
•
Malnutrition
•
Hypoglycemia
•
Vitamin deficiencies
•
Hyperlipidemia
•
Cushing's syndrome
Addison's Syndrome • Endemic Goiter •
Hypo and hyperthyroidism
• Thyroiditis •
Gynecomastia
•
Galactorrhea
2. Evaluation of the following signs and symptoms: • Thyroid nodule • Enlarged thyroid • Polyuria& polydipsia • Hypoglycemia
&hyperglycemic attack • Weight problems • polyphagia • Hirsutism
GASTRO
INTESTINAL (GI)
SYSTEM
GENITO
URINARY (GU)
SYSTEM
HEMATOLOGY
1.Diagnosis and treat the following conditions:
•
Dental hygiene
•
Hepatitis
–
viral& non-viral
•
Congenital pyloric stenosis
•
Gall bladder disease
•
Esophagitis
•
Appendicitis
•
Acute abdomen
•
Peptic ulcer disease (PUD)& Perforating peptic ulcer
•
Inguinal hernia
•
Incarcerated hernia
•
Gastritis
•
Hiatus hernia
•
Flatulence
•
Hemorrhoids
•
Rectal bleeding
•
Jaundice
•
Pancreatitis
•
Irritable bowel syndrome
•
Anal fissure/fistula/abscess
•
Inflammatory bowel disease
•
Common GI tumors
•
Diverticulosis
•
Volvulous
•
Malabsorption
•
Livrer Cirrhosis
•
Mesenteric Ischemia
•
Acute arterial occlusion
2. Evaluation of the following signs and symptoms:
*Heartburn *Epigastric pain *Nausea and vomiting *Dysphagia
*Diarrhea*Constipation*Malena*Hematemesis*Hematochezia
*Abdominal distention *Ascites*Jaundice
1.Diagnosis and treat the following conditions:
•
Cystitis
•
Testicular torsion
•
Pyelonephritis
•
Hematuria
•
Nephrolithiasis
•
Proteinuria
•
Urethritis
•
Prostatic CA
•
Prostatitis
•
Urinary retention - acute, chronic
•
Orchitis
•
Undescended testis
•
Epididymitis
•
Urinary incontinence
•
Benign prostatic hypertrophy (BPH)
•
Hydrocele
• Nephrotic Syndrome Uremia
2. Evaluation of the following signs and symptoms:
• Pyuria • Hematuria • Microalbuminuria • Protienuria • Casts • Dysuria
• frequency • Urgency • Penile discharge • Scrotal Pain, Masses, and swelling • Genital lesions
1.Diagnosis and treat the following conditions:
•
Anemia
•
Leukemia
•
Iron deficiency
•
Pernicious Anemia
•
Acquired immunodeficiency syndrome (AIDS)
•
Bruising
•
Multiple myeloma
• Lymphadenopathy • Routine anticoagulation.
RESPIRATORY
SYSTEM
MUSCULO
SKELETAL
SYSTEM
DERMATOLOGY
2. Evaluation of the following signs and symptoms
• Polycythemia • Leukocytosis • Leukopenia & leukemia • Bleeding tendency • lymphadenopathy
1.Diagnosis and treat the following conditions:
•
Asthma
•
Lung cancer
• Tuberculosis •
Acute bronchitis
•
Pneumonia
• COPD )
•
Pneumothorax.
2. Evaluation of the following signs and symptoms:
*Dysponea*Cough*Hemoptysis*Pleural effusion*Pulmonary nodule *wheezing.
1.Diagnosis and treat the following conditions:
•
Congenital spina bifida
•
Costochondritis
•
Hip dislocation
•
Neck pain
•
Club foot
•
Cervical disc disease
•
Osteoarthritis
•
Synovitis
•
Rheumatoid arthritis
•
Slipped femoral epiphysis
•
Spondyloarthropathies
•
Growing pains
•
Septic Arthritis
•
Nocturnal leg cramps
•
Back pain
•
Tendonitis
•
Disorders of gait, feet and legs in children
•
Sciatica
•
Chondromalacia
•
Bursitis - shoulder, knee, hip
•
Spinal stenosis
2. Evaluation of the following signs and symptoms: *Neck pain*Shoulder pain *Back pain *Hip pain *Knee pain *Foot pain*Arthralgia (s)*Arthritis (monoarticular, polyarticular) *Crystal induced arthritis*Sero negative arthritis *Osteoporosis* dermatological presentation associated with joint problem.
1.Diagnosis and treat the following conditions:
• Acniform eruptionCellulites • Varicella • Dermatitis – contact& other • Urticaria • Other childhood exanthemas • Papulasequamous eruptions(Psoriasis& lichen planus),
•
Tumors of the skin
(Melanoma,Squamous cell carcinoma, Basal cell epithelioma(BCE)
•
Ulcers
•
Disease of the hair
•
Pityriasis rosea
•
Lipoma
•
Lichen planus • Sebaceous cyst • Disorders of the nails(acute and chronic paronychia), • Skin infection( Bacterial ,viral, fungal & parasitic) :
Impetigo, Boils, Rubella, Herpes simplex, Herpes zoster, Scabies
• Sexually transmitted disease(STI). • Vitiligo • Pruritus ani •
Pruritus vulvae • Drug eruptions • Miscellaneous: dry skin,
dermographism, calluses, and corns..
EYE
ENT (Ears, nose, &
Throat)
1.Diagnosis and treat the following conditions:
•
Otitis externa
•
Rhinitis allergic/Non-allergic
• Otitis media( Acute and chronic) • Sinusitis-acute/chronic •
Acute/Chronic tinnitus • Hypertrophied tonsils • Vertigo •
Diseases of the mouth & tongue • Meniere ’ s disease • Epistaxis
• Wax removal • Cleft lip • Deafness • Cleft palate Otitis externa
Tonsillitis (indication for surgery), Bell ’ s palsy, anterior Rhinitis: vasomotor, allergic.Pharyngitis, laryngitis, epiglottitis. Croup syndrome.Aphtous stomatitis, glossitis. Cholesteatoma.
Mastoiditis. Otosclerosis. Teeth abscess. Peritonsillar abscess.
Obstruction of salivary glands.
2. Evaluation of the following signs and symptoms:
*Earache,Ear discharge*Decrease hearing*Tinnitus *Vertigo,
*Stuffy nose, * nasal obstruction* Mouth breathing *Snoring
*Cervical masses*Sore throat *Hoarseness *Facial and head pain*Dysphagia and odynophagia.
1.Diagnosis and treat the following conditions:
• Conjunctivitis(Viral, Bacterial, Allergic, Chemical, Ophthalmic neonartum, Trachoma) • Strabismus • Blepharitis • Cataract
• Hordeolum • Glaucoma • Pinguecla • Pterygium • Blindness
•
Keratitis/iritis
•
Chalazion
•
Refractive errors
•
ectropion,
• entropion,
• herodeolum,
• chalazian
•
Dacrocystitis
• dryness of the eye
•
Ocular disorders associated with systemic diseases
(Hypertension, Diabetes, Thyroid & Autoimmune disorders).
2. Recognize ocular emergencies provide first line management prior to referral: Angle closure glaucoma, Intraocular and orbital infections, Foreign bodies, injuries and lacerations.
3. Evaluation of the following signs and symptoms:
Red eye, Blurred vision, Eye pain, Photophobia, Loss of vision,
Floaters, Discharge, Visual field defect, Tearing.
MEN's HEALTH
ISSUES
WOMEN's HEALTH
ISSUES
Diagnosis and treat the following conditions:
• Erectile dysfunction • Benign prostatic hypertrophy • Hydrocele
• Varicocele • Undescended testicle • Torsion of the testes
• Premature ejaculation
1.
Diagnosis and treat the following conditions:
•
Screening for breast CA, inverted nipples, care of lactating breast, mastitis, abscess, fibrocystic disease of the breast, mastalgia, breast CA
•
Dysmenorrhea, amenorrhea, vaginal bleeding
• ovarian cyst •
Contraception
•
Antenatal, postnatal care and maternal nutrition common problems of puerperium
•
Depression
•
Mastitis
•
Endometritis
•
Thrombophlebitis
•
Violence and abuse
•
Osteoporosis
•
Menopausal problem
•
Infertility
• Breast lump.
ADOLESCENT and
CHILDREN
HEALTH
2. Evaluation of the following signs and symptoms: * Vaginal discharge * Vaginal itching * Pelvic pain including dysmenorrheal
*Abnormal bleeding and amenorrhea * Pelvic masses: uterine and ovarian * Dyspareunia* Incontinence * Menopausal symptoms *
Infertility
1.
Diagnosis and treat the following conditions:
•
Endocrinological changes
•
Disorder of growth and development
•
Physical changes - secondary sexual characteristics
•
Eating disorders (anorexia- bulimia, obesity, exercisers)
•
Tanner staging
•
Accident prevention
•
Sexuality issues
•
Immunization
•
Psychosocial issues and behavioral problem
•
Speech and learning disorders
•
Enuresis
•
Family dynamics
-Minimal brain dysfunction -Mental retardation-Disorders of language, speech and hearing -Reading disability
-Congenital anomalies -Chronic disease.
2. Evaluation of the following signs and symptoms:
Pediatric signs and symptoms: a- Newborn: -Premature and small for date – Jaundice -Respiratory distress and apnea -Feeding problems: Choking, vomiting -Failure to pass stool -pallor, cyanosis – Edema -Distended abdomen -
Petechiae and purpura – Seizure -Bulging fontanel -Mass in the abdomen or back
–
Hypothermia -Positive ortolani sign -Heart murmur -colic-Birth injuries – Fever.
B-Infants: -Fever -Excessive crying and irritability
–
Vomiting -
Diarrhea-Constipation -Mass in the abdomen -Rectal bleeding -
Failure to thrive -hematuria-Tachypnea
–
Stridor
–
Wheezing -
Cough
-Heart murmur – Hypertension -Microcephaly and macrocephaly
-Seizures – Strabismus – Cataracts -Rash: Diaper rash, Eczema,
Infectious purpura and Petechiae – pallor -Enlarged lymph nodes
-In-toeing and out-toeing -Undescended testes
C-Children : -Abdominal pain -Mass in the abdomen – Diarrhea –
Constipation -Rectal bleeding -Rectal itching – Hematuria -
Frequency, Dysuria -Sexual precociousity -Short stature – Obesity
-Enuresis & UTI -Polyuria and polydipsia – Fever -Sore throat -Ear ache -Recurrent URTI -Snoring – Wheezing – Tachycardia -Heart murmur
-Hypertension
–
Arthritis -Knee pain and leg pain
– lump -scoliosis
-convulsion
–
Headache
–
Coma
–
Vertigo -Rashes and itching
-Learning disabilities d) Adolescent
-Acne -Short stature – Obesity -Abdominal pain -Headache
-Anorexia, weight loss -Polyuria, polydipsia-Behavioral problems
PSYCHIATRY 1.
Diagnosis and treat the following conditions:
• Affective disorders(Reactive depression, Endogenous depression,
Mania ,Bipolar (manic-depressive) disorders, Pathologic grief reaction) • Stress & adjustment disorders Generalized anxiety disorders Psychosomatic disorders(Hypochondriasis,Somatization disorder(Briquet ’ s syndrome, hysteria) • Psychogenic pain disorder
Conversion disorder • Factitious disorders and malingering), •
Substance abuse disorders (Alcohol, Tobacco, Illicit drugs, anabolic steroids)
•
Psychotic disorders ( Schizophrenia, and other psychiatric disorders including organic diseases with psychiatric presentation including the organic brain syndrome )
• Psycho sexual dysfunction.
Personality disorders : (Compulsive, Histrionic, Paranoid, Dependent,
Passive- aggressive, Antisocial &borderline).
LIFESTYLE
COUNSELING
1-Health maintenance counseling including ( Sexually transmitted diseases (STDs) • Nutrition • Breast feeding • Exercise and safety issues)
2-Diet (including those with Diabetes, Hypertension, IBS, Peptic ulcer& hyperlipidemia)
3-Stress management technique
4-Smoking, drugs & Substance abuse cessation
5- Premarital counseling
6marital and family counseling:
-Contraception including surgical sterilization-Infertility and artificial insemination. -Adaptation to child bearing. -Impact of new infant on family life. -Abortion and still-birth. -Menopause.
Ability to deal with and support
Acquire the basic rehabilitation techniques
1-Chronicaly ill patient
2-Dying patient
3-Handicapped patient
1post MI
2-post stroke
3-Post neurological deficit
4-post surgical and accidental organ loss (amputation, mastectomy& vision loss)
2-The common office procedures, techniques and investigations:
Type Procedures ,techniques and investigations a) Dermatological procedures Skin biopsy& excision of cysts, naevi, and other lesions - wart cryotherapy - suturing - skin scrapings for fungus
- I&D of abscess - treatment of paronychia
- Burn dressings - foot care - stasis ulcer care
- wedge/partial/total resection of ingrown toe nail
- KOH smears examination (potassium hydroxide).
-Application of liquid nitrogen.
b) Ortho procedures -Joint injection and aspiration
c) GU procedures d) ENT procedures e) Eye procedures
-Insertion of Foley catheters
- insertion and removal of intrauterine device (IUD)
- Removal of wax - nasal packing - Visual Acuity
-Use of pneumatic otoscope. -Rinne and Weber test.-Indirect laryngoscope -Use of head mirror. -
Digital exam of pharynx and oral cavity. -Foreign body removal from ear, nose, throat.- Cerumen removal.- Nasal packing and Cautery.Interpret
Audiograms and Tympanograms.
-Examination of external ocular structure. -Testing visual acuity and color vision. -Use of direct ophthalmoscope.
-Use of Schiotz tonometer-Testing of visual fields.
-Use of fluorescence. -Pinhole test. -Cover-uncover test.
-Be aquatinted with indications, contra- indications and side effects of eye medications: -Mydiriatics &Cycloplegics.
-Topical corticosteroids. -Topical antibiotics. -
Topical Anthesthesia f) CVS and Respiratory procedures - ECG interpretation Chest x-ray interpretation
- PFM and use of spirometry Inhaler technique -
Venipuncture- Arterial puncture, Interpretation of arterial blood gases g)GIT procedures -H. pylori testing breath test
-Insertion of nasogastric tubes
-Paracentesis h)Neurological -Lumbar puncture
i)Lifesaving procedures -CPR
-Cardio version
-Relieving life threatening pneumothorax
-Endotracheal intubation
- Penetrating trauma to the neck, thorax or abdomen
- Blunt trauma to head
- Multiple fractures
- Hemothorax
- Fractures of the spine l) General surgical techniques - Implement sterile techniques
- State the stages of wound healing and care
- List the characteristics of different suture materials
- Apply local and digital block anesthesia
- Name the indications and complications of different surgical techniques
- State the alternative for the surgical procedure carried when applicable a) m) Office surgical procedures -Suturing of simple wound
-Excisions of skin and subcutaneous lesions: moles, skin tags, epidermoid cyst, Lipoma
- Incision and drainage of abscesses
-Removal of ingrown toe nails
- Emergency care of burns
- Casting and splint use
- Aspiration and injection of joints
Breast cyst aspiration
-Anoscopy n)Office obstetric &gynecological -Cautery for benign lesions procedures
- Administration, follows up, and side effect management of the following contraceptive methods.
-Barrier Contraception(Condoms) -Intrauterine device.
-Oral contraceptives.
-Normal cephalic vaginal delivery. -Episiotomy and repair -awareness of the signs of obstructed labour and its management. -Perform a Pap smear-Depend on risk assessment during prenatal follow up -Assess pelvic adequacy for pregnancy and delivery. -Perform and interpret fetal assessment test in the third trimester (NST) -Evaluate fetal maturity and fetoplacental adequacy -Perform fetal monitoring. o)Pediatric &Neonatology techniques &procedures
-Techniques &procedures for care of the newborn:
* Measure the Apgar score.
* Suction the nasopharynx.
* Worm the new born.
- Insert the IV line.
- Resuscitation newborn, infant, and older children.
- Do lumbar puncture.
-Perform suprapubic bladder aspiration.
- Give immunization shot
- Take throat swab
- Perform an ECG and interpret the finding p) Routine laboratory procedures ,techniques and investigations: q)Diagnostic radiological investigations
- Take blood pressure measurements
- Identify infant in distress
- urinalysis: dipstick microscopic venipuncture
- stool for OB - cultures: throat ,nasopharyngeal, cervix/vagina &urethra
- pap smear - injections: ID/SC/IM
Plain X-rays commonly used in PHC:CXR,
Bone/joint, Spine, Abdomen (urinary tract, pelvis)
Mammography
Barium enema : double contrast, neoplasm, ulceration
,narrowing, Dilatation: obstruction, ileus, volvulus
Filling defect, Ulceration.
IVP : kidney, collecting system, pelvis & uterus, bladder.
Nuclear medicine: bone scan, liver spleen scan, lung scan
Ultrasound: Abdomen: liver, spleen, kidney, pancreas Pelvis: gynecological, prostate, bladder, obstetrics
Thyroid ,Breast &Testicle
Computed tomography : Head & neck& Body
MRI: Brain, spine , Musculoskeletal,Pelvis (prostate, gynipathology)
INTERNAL MEDICINE ROTATION
Introduction:
A significant proportion of medical problems which are encountered in primary care, practice are related to the discipline of internal medicine. Primary care doctors are required to be competent in initial assessment and management of all of these medical problems.
Duration : 6 MONTHES.
Objectives:
At the end of the rotation, the resident should acquire knowledge, skills, and demonstrate competence in:
1.Taking care of hospitalized patients in terms of recording a proper history, performing a comprehensive physical examination and be capable in making accurate diagnosis, investigations, and appropriate management of the common medical conditions encountered in Internal Medicine.
2.
Recognizing the condition, initiate appropriate diagnostic and therapeutic measures for the other less common conditions.
3.
Identifying the medical problems which need referral and arranging a proper referral to the most appropriate department.
4.
Identifying hazards of drug treatment, drug interactions, and new advances in therapeutics relevant to Internal Medicine.
5.
Applying the patient-centered model in caring for hospitalized patients and incorporate lifestyle issues, palliative care, ethical decision-making, and family counseling.
Process of Training:
The residents must work on a full time basis as a member of the internal medicine team; participate in the services and educational activities.
Residents should rotate in all major medical subspecialties (cardiology, pulmonary, neurology, etc.).Opportunities to work in outpatient clinics should be provided with multidisciplinary approach to caring for illness, showing the role of nurses, social workers and physiotherapist is important.
Learning situation:
•
In-patient Internal Medicine wards
•
Out-patient clinics of Internal Medicine
•
Continuing medical education(CME) activities
•
CCU
•
Procedure Rooms (Endoscopy, echo, etc.)
Content of Training:
1-Cardiovascular:
•
Common and/or Important conditions:
-Coronary Artery Disease -Congestive Heart Failure -Essential Hypertension -
Supraventricular tachyarrhythmias -Valvular Heart Disease -Peripheral Vascular Disease
-Dyslipidemia
•
Other Less Common conditions:
-Pericardial Disease -Ventricular arrhythmias -Cardiomyopathies -Heart Block
2-Respiratory:
•
Common and/or Important conditions:
-Upper Respiratory Tract Infections -Pneumothorax -Pneumonia and Bronchitis -
Tuberculosis -Bronchial Asthma -Smoking
•
Other less Common conditions:
-Pulmonary Embolism -Respiratory Failure -Interstitial Lung Disease -Lung
Cancer
3-Central nervous System:
•
Common and/or Important Conditions:
-Seizure Disorders -Stroke syndromes -Headache -Bell ’ s Palsy -Meningitis and
Encephalitis -Parkinson Disease
•
Other less Common conditions:
-Dementia -Multiple Sclerosis -Delirium
4-Gastrointestinal Tract:
•
Common and/or Important Conditions:
-Gastroesophageal Reflux Disease -Gastroenteritis -Peptic Ulcer Disease and H-
Pylori Infection -Inflammatory Bowel Disease – Constipation -
Hepatitis -Irritable Bowel Syndrome
•
Other less Common conditions:
-GI malignancies -Pancreatitis -Inflammatory Bowel Disease.
5-Endocrinology
•
Common and/or Important Conditions:
-Diabetes Mellitus - Type 1 and 2 -Obesity -Thyroid Disease -Hyperuricemia
•
Other less Common conditions:
-Pituitary Disease -Adrenal Disease
6-Infectious Diseases:
•
Common and/or Important Conditions:
-Malaria -Pyrexia of Unknown Origin -Human Immunodeficiency Virus (HIV)
•
Other less Common conditions:
-Brucellosis -Leishmaniasis
7-Rheumatology
•
Common and/or Important Conditions:
-Osteoarthritis -Acute arthropathies -Rheumatoid Arthritis -Chronic inflammatory arthropathies.
•
Other less Common conditions:
-Polymyalgia rheumatica -Vasculitis -Systemic Lupus Erythematosus (SLE)
8-Renal:
Common and/or Important Conditions:
-Glomerulonephritis -Hematuria -Pyelonephritis -Proteinuria -Renal failure
Other less Common conditions:
-Renal cell tumors
9-Hematology
Common and/or Important Conditions:
-Anemia -Bleeding disorders
Other less Common conditions:
-Myeloproliferative disorders -Leukemia -Lymphoma
Lists of Skills to be learned:
-Venipuncture -Arterial puncture -Interpretation of arterial blood gases -
Serial Peak Flow measurement. -Spirometry -Chest x-ray interpretation -
Inhaler technique -H. pylori testing -breath test -Lumbar puncture -ECG interpretation -Use of ophthalmoscope in examining fundi -Stress test interpretation -Endotracheal intubation -Insertion of nasogastric tubes -Paracentesis
-Insertion of Foley catheters -Joint injection and aspiration
EMERGENCY ROTATION
Introduction:
The family physician must become competent to deal with any emergency situation, which he/she might encounter at the health center.
Duration: 2 months, 1month within internal medicine rotation &1month within general surgery rotation.
Objectives:
At the end of this rotation, the resident should be able to:
1. Make an initial assessment; begin treatment of any emergency condition of all age groups and make an appropriate referral when needed.
2. Learn and practice basic minor orthopedic and surgical procedures.
3. Communicate effectively and compassionately with patient and families.
Process of Training:
During the rotation the resident will work as full time in the emergency unit.
Residents should participate in the service and educational activities of the department.
Learning situations:
•
Clinical setting.
Content of Learning
•
Cardio respiratory arrest
•
Ischemic heart disease ( acute myocardial infarction and unstable angina)
•
Life threatening arrhythmias
•
Heart failure
•
Drowning
•
Acute laryngeal obstruction
•
Raised intra-cranial pressure and head injury
•
Poisoning, inhalation and envenomation of environmental exposure.
•
Infectious emergencies, including meningitis
•
Trauma
•
Acute abdomen
•
Anaphylaxis and hypersensitivity reactions
•
Dehydration and shock
•
Hypoglycemia , hyperglycemia and diabetic keto-acidosis
•
Status Asthmaticus
•
Status epilepticus and febrile convulsions
•
Sickle cell crises
•
Moderate and severe burns
•
Foreign bodies
•
Common fractures in adults and children
•
Psychiatric emergencies, including violent patients
•
Obstetric and gynecologic emergencies
List of Skills:
•
General skills
•
Resuscitation
•
Insertion of cannula (adult and pediatric)
•
Set up delivery line/drip
•
Administer IV, IM injections
•
Urethral catheterization (male and female)
•
Needle thoracocentesis
•
Arterial blood gases
•
Suturing
•
Drainage of abscesses
•
Lumbar puncture
•
Interpretation of radiological images in the emergency setting
GENERAL SURGERY ROTATION
Introduction:
Many surgical conditions presents commonly to the primary health care physician. A significant proportion of these problems could be dealt at a primary care practice. The Family Physician should provide comprehensive care for the common surgical conditions.
Duration: 4 months.
General Objectives:
At the end of Surgery rotation, the residents should be able to:
1.
Recognize and manage common surgical problems and emergencies which may need referral to the surgeon.
2.
Perform with competency minor surgical procedures, e.g. Incision of abscesses, suturing, dressing, removal of foreign bodies and circumcision.
3.
Understand how patients are managed pre-and post-operatively, e.g.
Explaining to patients about surgery and taking consent.
Contents:
•
Wound management
•
Acute abdomen and abdominal pain
•
Preoperative evaluation and management
•
Postoperative management
•
Breast lump
•
Thyroid lumps
•
Hernias
•
Common urological conditions
•
Renal calculi
•
Torsion of the testes and other testicular conditions
•
Anorectal conditions including hemorrhoids
•
Prostate disease including benign prostate hypertrophy
Process of Training:
The residents must work on a full time basis as a member of the surgical team; participate in the services and educational activities.
Learning Situation:
•
Out-patient clinics.
•
In-patient wards.
•
Minor surgery.
•
Operation Theater.
•
Continuing medical education (CME) activities.
Lists of Skills to be learned:
•
Suturing of simple wounds
•
Excision of skin and subcutaneous lesions: Sebaceous, dermoid, cysts or
Lipoma
•
Incision and drainage of abscesses
•
Removal of ingrowing toe nails
•
Circumcision
ORTHOPEDIC ROTATION
Introduction:
Many orthopedic and sports related conditions presents commonly to the primary health care physician. A significant proportion of these problems could be dealt with in a primary care practice. The family physician should provide comprehensive care for common orthopedics conditions.
Duration : 1 months within general surgery rotation .
General Objectives:
At the end of this rotation the resident will be able to:
1. Identify and manage common fractures.
2. Perform initial assessment of musculoskeletal injuries.
3. Apply casts and slabs for different conditions independently.
4. Manage patients with chronic joint disorders.
5. Perform specific orthopedic physical and radiological examinations and
Procedures.
6. Recognize the role of physiotherapy in the management musculoskeletal
Problems.
7. Make physical activity prescriptions.
Process of Training:
The residents must work on a full time basis as a member of the Orthopedic
Department.
Learning Situation:
•
Out-patient clinics.
•
In-patient wards.
•
Emergency Room.
•
Operation Theater.
•
Continuing medical education (CME) activities.
Contents:
•
Common fractures in adults and pediatrics.
•
Back pain.
•
Neck pain.
•
Shoulder pain.
•
Ankle and knee pain.
•
Arthritis.
•
Carpal Tunnel Syndrome.
•
Tendonitis and bursitis.
Lists of Skills to be learned:
•
Joint and spine examination.
•
Casting, splinting and bandaging.
•
Interpretation of radiological images.
•
Joint aspiration and injection of joints.
PEDIATRIC ROTATION
Introduction:
Children represent a significant proportion of the daily attendance to the primary health care system. This necessitates a proper systematic and a holistic approach to this age group by the family physician.
Duration: 4 months.
General Objectives:
By the end of the pediatric rotation, the residents should be able to:
1. Establish rapport with the patients and their families, and obtain a comprehensive history.
2. Perform a complete physical examination.
3. Formulate a problem list, differential diagnosis and plan of management, taking into consideration the available resources.
4. Assess growth and development, use growth charts, and detect the deviant cases.
5. Interpret common laboratory results, and read simple x-rays (i.e. chest, abdomen, etc).
6. Gain pharmacological knowledge of common medications used.
7. Demonstrate how to provide care to the newborns and the infants.
8. Recognize cases that need referral to the hospital or to the specialist.
9. Identify, assess and manage children with disabilities.
10. Define available resources within the community and learn how to utilize them.
Process of Training:
The resident must work on a full time basis as a member of the Child Health team; participate fully in all of the educational activities.
Learning situation:
•
Out-patient clinics.
•
Emergency Room.
•
In-patient wards.
•
Neonatology Department.
•
Continuing medical education(CME) activities.
Contents:
1-Pediatric Emergencies:
The resident should recognize the following life threatening conditions and be able to stabilize the patient before transferring to the hospital.
-Epiglottitis -Sickle cell crisis -Severe respiratory infections -Status Asthmaticus
-Chocking – Status -epilepticus -Anaphylaxis -Cardiorespiratory resuscitation
-Heart failure and cyanotic heart diseases -Septic shock -Poisoning and drug overdose -Hypovolemic shock.
2-Care of the newborn babies:
1. The resident is expected to be knowledgeable and skillful in performing the followings such as:
•
Resuscitation of newborn babies.
•
Assessing Apgar score.
•
Performing routine newborn examination and detect any abnormalities.
•
Managing neonatal jaundice.
•
Managing infant of diabetic mother.
2. The resident should have some knowledge about :
•
Prematurity.
•
Birth asphyxia.
•
Respiratory distress syndrome.
•
Neonatal and intrauterine infections.
3-Genetics and Congenital Anomalies:
The resident should gain adequate knowledge related to the following areas:
•
Genetic disorders, e.g. Down syndrome, Turner Syndrome.
•
Consanguinity and its impact on health,
•
Genetic counseling.
4-Pediatric nutrition:
The resident should acquire basic knowledge about the followings :
•
Breast feeding and its advantages.
•
Modified cow's milk formula, its advantages and disadvantages.
•
Recommended children's daily requirements for proteins, carbohydrates, fat, vitamins and minerals.
•
Weaning food and time of its use.
•
Protein energy malnutrition, causes, manifestation and management.
•
Iron deficiency anemia, diagnosis, and management.
•
Various diseases related to nutritional deficiencies, e.g. Vitamin A
• deficiency, Vitamin B Deficiency, Ricketts, etc.
5-Systemic Infections:
The resident should be able to recognize and manage the following common pediatric problems. Such as:
-Respiratory tract infections -Tuberculosis -Tonsillitis -Gastroenteritis
-Simple urinary tract infection -Endocarditis -Viral infections like measles, rubella, mumps, and chicken pox -Pneumonias -Meningitis
6-Cardiovascular System:
The resident should be able to recognize the following clinical conditions and transfer them to the hospital for further work up like :
•
Congenital heart disease.
•
Valvular heart disease.
•
Arrhythmias.
•
Congestive heart failure.
•
Hypertension
•
Rheumatic heart disease.
7-Gastrointestinal System:
The resident should have adequate knowledge and ability to diagnose and manage the following conditions:
-Gastroenteritis -Acute and chronic constipation -Simple cases of nutritional anemia -
Intestinal infestations -Common and congenital GI disorder they should be able to recognize the following conditions and refer them for further work-up and management:
-Chronic diarrhea and malnutrition -Chronic malabsorption -Failure to thrive. -
Liver disease.
8-Central nervous System:
The resident should acquire basic knowledge about:
•
Headache in children.
•
Diagnosing and managing febrile convulsions.
•
Symptoms and signs of raised intracranial pressure.
•
Cerebral palsy and its complications.
•
Seizure disorder.
9-Hematological system:
The resident should acquire basic knowledge pertinent to the following conditions:
•
Diagnosis and management of iron deficiency anemia.
•
Diagnosis and management of sickle cell disease, and other hemoglobinopathies.
•
Diagnosis of G6PD deficiency, and hemolytic crises.
•
Signs and symptoms of leukemia and other bleeding disorders.
10-Endocrinal conditions:
The residents should acquire basic knowledge and manage the followings:
•
Diabetes mellitus and diabetic ketoacidosis
•
Hypothyroidism and hyperthyroidism and interpret the TSH in a newborn
•
Other hormonal disorder, e.g. growth hormone and adrenal hormone
11-Musculoskeletal system:
The residents should be able to recognize signs, symptoms and differential diagnosis of the followings:
-Septic arthritis and/or osteomyelitis -Rheumatoid arthritis -Rheumatic arthritis -
Arthralgia
Lists of Skills to be learned:
The residents are expected to perform the following basic procedures by the end of their rotation:
-Venipuncture -Lumbar puncture -Starting IV line -Bladder tap
-Resuscitation of the newborn and older children
OBSTETRICS & GYNECOLOGY ROTATION
Introduction:
A significant proportion of problems dealt within a primary care practice are related to the discipline of obstetrics and gynecology.
The family physician should be competent in providing comprehensive care in dealing with all obstetrics and gynecology cases seen in primary health care practice
Duration: 4 months.
Objectives:
At the end of rotation, the resident will be able to:
1.
Recognize national health structures, policy and guidelines of obstetrics and gynecology cases.
2.
Provide excellent antenatal and postnatal care including promotive, preventive and rehabilitative aspects.
3.
Identify high risk patients, apply proper interventions and arrange appropriate referrals.
4.
Manage common obstetrics and gynecology conditions
5.
Identify and provide interim management of life threatening problems during pregnancy.
6.
Manage normal delivery.
7.
Understand the management of complicated labor.
8.
Perform screening, counseling and health education in the issues related to mother and fetus aspects.
9.
Order proper and necessary investigations.
10.
Identify and apply proper interventions for cases that need specialist consultation.
11.
Perform technical procedures commonly practiced in primary care (see skill list below).
Process of Training:
The resident must work on a full time basis as a member of the Obstetrics and
Gynecology team; participate fully in both the service and educational activities.
Learning situation:
•
In-patient wards.
•
Delivery room.
•
Out-patient clinics.
•
Operation Theater.
•
Emergency Room.
•
Continuing medical education (CME) activities.
Content of Training:
1-Obstetrics:
•
Normal antenatal care: diagnosis, establishing due dates, screening, assessment of progress, patient education.
•
High risk pregnancy: identification, proper initial management and referral.
•
Medical problems in pregnancy: i.e. diabetes, hypertension, thyroid disease, anemia, smoking, etc.
•
Health education and counseling: genetic counseling, breast feeding, nutrition, birth spacing, etc.
•
Normal labor and delivery.
•
Labor and delivery problems: i.e. obstructed labor, infection, fetal distress, post partum and intrapartum bleeding, pupueral pyrexia, etc.
•
Antenatal bleeding and abortions.
•
Obstetric emergency: i.e. preterm labor, premature rupture of membrane.
•
Indications for cesarean section, and other assisted delivery procedure (e.g. ventouse and forceps)
2-Gynecology:
•
Physiology and problems of menstruation.
•
Abnormal uterine bleeding.
•
Infection and diseases of the female reproductive system including sexual
•
Transmitted diseases.
•
Breast disorders.
•
Trauma to the reproductive system including sexual assault.
•
Pelvic pain.
•
Benign and malignant neoplasia of the female reproductive system.
•
Menopause and geriatric gynecology.
•
Cervical conditions
•
Ectopic pregnancy.
•
Family planning and birth spacing.
•
Infertility.
•
Family and sexual counseling.
•
Gynecological problems in children.
Lists of Skills to be learned:
•
Obtaining vaginal and cervical cytology.
•
Microscopic diagnosis of urine and vaginal smears.
•
Ultrasound examination (viability scan) and interpretation.
•
Management of labor.
•
Induction of labor.
•
Episiotomy repair.
•
Assistance in cesarean section.
•
Neonatal resuscitation.
•
IUCD Insertion.
PSYCHIATRY ROTATION
Introduction:
A significant proportion of problems dealt with in a primary care practice are related to the discipline of psychiatry.
The Family Physician should be able to provide appropriate psychiatric care for children, adolescents, adults and geriatric population.
Duration: 2 months
Objectives:
At the end of rotation, the residents should be able to:
1. Take a good psychiatry history.
2. Recognize and manage patients with psychiatric illness in primary health care.
3. Identify psychiatric conditions which need referral.
§ Manage emergency cases in psychiatry.
§
Identify contributing factors that affect the etiology and management of the illness.
§
Identify the role of other professionals involved in the care of patients with mental disorders such as psychologist and social workers.
Process of Training:
The residents must work on a full time basis as a member of the psychiatry team; participate fully in both the services and educational activities.
Learning Situation:
•
OPD Clinic
•
In-patients
•
Emergency room
•
Continuing medical education(CME) activities
Content of Training:
•
Mood disorders as major depressive disorder, dysthymic, adjustment disorder disturbance of conduct, bipolar disorders
•
Anxiety disorder e.g. panic attack, phobias, obsessive/compulsive disorder, generalized anxiety disorder
•
Somatoform disorders e.g. somatisation, pain, hypochondriasis
•
Normal and abnormal psychological growth and development across the life cycle and variants.
•
Role of the family and its function in coping with stress
•
Cognitive disorders such as dementia, delirium, amnestic disorder, etc.
•
Substance related disorders e.g. alcohol, opioids, amphetamines, etc.
•
Psychotic disorders e.g. schizophrenia
•
Sleeping disorders e.g. insomnia, hypersomnia, narcolepsy, parasomnias
•
Eating disorders e.g. anorexia nervosa, bulimia nervosa
•
Personality disorders
•
Problems related to physical (including domestic violence), social and psychological abuse e.g. domestic violence, physical abuse: acute, chronic, neglect, emotional abuse, Munchausen ’ s by proxy, sexual abuse/incest, family breakdown, community and legal resources (crisis and ongoing)
•
Other treatment modalities as psychotherapy, behavioral therapy, relaxation technique, etc.
Behavioral Pediatrics:
The residents are required to manage the following abnormal behaviors:
•
Learning disorders.
•
Hyperactivity.
•
Mental retardation.
•
Language problems.
E.N.T. (OTOLARYNGOLOGY) ROTATION
Introduction:
A significant proportion of problems dealt with primary health care are related to the specialty of ENT. The family physician should be competent in initial assessment and management of common ENT problems.
Duration: 2 months
Objectives:
At the end of the rotation, the resident should be able to:
1. Recognize, assess and manage common ENT conditions dealt with in primary health care.
2. Recognize, assess and provide interim management of ENT emergencies.
3. Suspect and early recognize ENT tumors and perform appropriate and timely referrals.
4. Identify the ENT conditions which should be referred to secondary care.
5. Identify psychosocial factors affecting ENT conditions.
Process of Training:
•
In-patient wards.
•
Out-patient clinics.
•
Operation Theater.
•
Emergency Room.
•
Continuing medical education (CME) activities.
•
Contents of Learning:
1. Demonstrate basic knowledge related to: a. Anatomy of ENT. b. ENT examination. c. Hearing tests.
2. Management of Common ENT conditions encountered in PHC: a. Throat infections. b. Painful and discharging ear (otitis media, eternal). c. Acute and chronic nasal congestion and discharge. d. Acute and chronic Sinusitis. e. Nasal obstruction. f. Deafness. g. Tinnitus and vertigo.
3. Management of ENT emergencies: a. Epistaxis. b. Stridor. c. ENT trauma.
Skills to be learned:
•
Ear wax removal.
•
Wick application and removal.
•
Ear syringing.
•
Nasal packing for epistaxis control.
•
Audiogram interpretation.
•
Foreign body removal from ENT tracts.
•
Emergency needle tracheostomy.
DERMATOLOGY ROTATION
Introduction:
The family physician should be competent in the initial assessment and management of common dermatological problems.
Duration: 2 months
Objective:
At the end of the rotation, the resident should be able to:
1. Attain the practical knowledge needed for the diagnosis and treatment of common skin conditions in all age groups.
2. Diagnose, assess and manage acute and chronic dermatological conditions.
3. Recognize the skin manifestations of systemic diseases.
4. Identify the dermatological conditions which should be referred to secondary care.
5. Recognize serious conditions and perform appropriate and timely referrals.
6. Identify psychosocial and economic factors affecting skin conditions.
Process of Training:
During the rotation, the resident will work as full time in the Dermatology department. They are expected to participate in the services and educational activities of the department during the rotation.
Learning Situation:
•
Out-patient clinics
•
In-patient wards
•
Continuing medical education(CME) activities
Content of Training:
•
Variations of normal skin
•
Morphology of skin lesions
•
Creams, ointments and how to use them
•
Eczema
•
Seborrheic dermatitis
•
Psoriasis
•
Infections, infestations:
•
Impetigo
•
Perianal streptococcal infections
•
Thrush
•
Scabies, lice
•
Common birth marks
•
Urticaria
•
Drug/food rashes
•
Nappy rash
•
Viral exanthemas
•
Acne vulgaris
•
Acne rosacea
•
Pruritus.
•
Photosensitivity.
•
Dry, itchy skin.
•
Papulasequamous diseases.
•
Moles and melanomas.
•
Skin disorders in old age
•
Skin manifestation of systemic diseases.
•
Lichen planus.
•
Pityriasis rosea
•
Alopecia.
•
Blistering disorders.
•
Pemphigoid.
•
Pemphigus.
•
Hematomas:
•
Strawberry naevus.
•
Pyogenic granuloma.
•
Sexually transmitted infections (STIs):
•
Diagnosis, testing and referral for common STIs.
•
Current effective treatments for common STIs.
•
Contact tracing and the management of partners with STIs.
• legal requirements of GP ’ s in relation to STIs
•
HIV antibody testing and protocols
•
Providing support, primary care and in conjunction with a local Specialist unit).
•
Social and emotional aspects.
•
Infection control.
•
Treatment of genital warts.
•
Planter and palmar warts and cones.
Lists of Skills to be learned:
•
Thermal cautery.
•
Cryotherapy.
•
KOH preparation, microscopy.
•
Skin biopsy.
•
Use of Wood's light.
•
Excision of small tumor.
•
Intralesional injection.
OPHTHALMOLOGY
ROTATION
Introduction:
The family physician will frequently encounter many eye related problems in primary health care. Therefore, he/she should be equipped with the necessary knowledge and skills in order to make accurate diagnosis and appropriate management.
Duration: 2 months.
Objectives:
At the end of this rotation, the resident should be able to:
1. Diagnose and treat common eye conditions
2. Recognize, assess, manage and appropriately refer serious ophthalmologic cases.
3. Perform common ophthalmologic procedures which can be done at primary care practice.
4. Describe the social, economical, and cultural factors affecting ophthalmology problems.
5. Give appropriate advice on preventive and rehabilitative aspects of eye conditions.
Process of Training:
The residents must work on a full time basis as a member of Ophthalmology team and participate fully in both the services and educational activities.
Learning Situation:
•
OPD Clinic
•
In-patients wards
•
Emergency room
•
Operating theatre
•
Continuing medical education(CME) activities
Contents:
•
Red Eye
•
Eye trauma, including corneal abrasion, corneal foreign body, etc.
•
Painful conditions, e.g. Herpes simplex infections
•
Glaucoma
•
Corneal ulcer (refer for expert management)
•
Scleritis (refer for expert management)
•
Iridocyclitis (refer for expert management)
•
Perforation. Penetrating injury of the globe ((refer for expert management)
•
Acute visual loss
•
Common Pediatrics eye problems
•
Squint
•
Diabetic/hypertensive retinopathy (refer early for intervention)
•
Retinal artery thrombosis, amaurosis fugax.
•
Retinal detachment (refer immediately for expert management)
•
Corneal abrasion
•
Cataract
•
Blocked tear duct
•
Infectious and allergic conjunctivitis
•
Unilateral eye problems
•
Visual acuity testing
•
Ambylopia
•
Retinoblastoma
List of Skills to be learned:
•
Proper ophthalmic examination
•
Fundoscopic examination (identify normal fundus and major abnormalities e.g.
Papilloedema, cupping nerve head, diabetic retinopathy, hypertension and retinal detachment, etc.
•
Irrigation of an eye
•
Fluorescein staining of cornea
•
Testing of visual acuity
•
Removal of foreign body
LABORATOTY MEDICINE ROTATION
Introduction:
The family physician will frequently need many laboratory investigations in primary health care. Therefore, he/she should be equipped with the necessary knowledge and skills in order to make accurate interpretation of the result of the laboratory investigations &be able to do the routine laboratory investigations.
Duration:1 month.
Objectives:
At the end of this rotation, the resident should be able to:
The trainee should have brief information about the overall laboratory operation as sample collection& handling used in the lab, reading and interpreting the lab investigations.
Process of Training:
The residents must work on a full time basis as a member of laboratory team and participate fully in both the services and educational activities during the rotation.
Learning Situation:
Inpatient & outpatient laboratory & Blood bank
Contents:
Microbiological section:
The trainee should have brief information about the overall operation in the section, sample collection& handling, culture media used in lab and interpreting Gram stain and Zeil-Neelson stain (z-n), it also involves:
1.
Urine and Stool examination.
2.
Blood, bone marrow and mycobacterium.
3.
Antibiogram.
•
The difference between identification and susceptibility disc.
•
The choice of antibiotic discs according to specimen and to organism isolated.
4.
Others :
Fungi +KOH smear, general ideas about special test like:
Salmonella typing, antigen detecting of bacteria & Cryptococcus in CSF.
Hematology section:
•
Prepare a smear, stain and read differential WBC count.
•
Do ESR test and read it.
•
Blood film inspection: normal &abnormal.
•
Reticulocyte reading.
•
Do manual hematocrit and read it.
Serology section:
•
Techniques of serology: agglutination, ELIZA, precipitation, etc.
•
Know the spectrum of tests positive values, causes of false positive.
•
Observe the ongoing test, their performance and interpretation.
•
Perform one slide and tube agglutination test, read, and interpret.
Chemistry section:
•
Collection &handling of appropriate specimens, type of containers and preservatives+ additives used for particular tests.
•
Special chemistry, like organic acid, toxicology
Blood bank:
•
Learn practice donor selection, complete procedure.
•
Screening test : VDRL,Hbs Ag, HCV,HIV
•
Learn and practice grouping and Rh :* Cell grouping
* Serum grouping
•
Learn and practice Coombs test: direct & indirect
•
State the side effect of blood transfusion
List of Skills to be learned:
Routine laboratory procedures, techniques and investigations as:
- Urinalysis: dipstick microscopic venipuncture - stool for OB - cultures: Throat, nasopharyngeal,
Cervix/vagina &urethra - pap smear - injections: ID/SC/IM.
DIAGNOSTIC RADIOLOGY ROTATION
Introduction:
The family physician will frequently need many radiological investigations in primary health care. Therefore, he/she should be equipped with the necessary knowledge and skills in order to make accurate interpretation of the result of the radiological investigations.
Duration: 1 month.
Objectives:
At the end of the radiology rotation each resident should be able to interpret common radiological investigations.
Process of Training:
The residents must work on a full time basis as a member of radiological team and participate fully in both the services and educational activities during the rotation.
Learning Situation:
Inpatient& outpatient radiological unit.
List of Skills to be learned:
Interpretation of the diagnostic radiological investigations as plain X-rays, Barium enema IVP, Ultrasound, Nuclear medicine, Computed tomography& MRI.
Contents:
•
Interpret plain X-rays commonly used in PHC:
CXR, Bone/joint, Spine, Abdomen (urinary tract, pelvis) Mammography
•
Barium enema : double contrast, neoplasm, ulceration, narrowing, Dilatation: obstruction, ileus, volvulus, filling defect, Ulceration.
•
IVP : kidney, collecting system, pelvis & uterus, bladder.
•
Nuclear medicine: bone scan, liver spleen scan, lung scan
•
Ultrasound: Abdomen: liver, spleen, kidney, pancreas
Pelvis: gynecological, prostate, bladder, obstetrics
Thyroid, Breast, Testicle.
•
Computed tomography : Head & neck, Body
•
MRI:
-Brain, spine, Musculoskeletal, Pelvis (prostate, gynipathology).
ELECTIVES ROTATION
Introduction:
The aim of the elective is to help the resident in selecting specific areas of interest which will further enhance overall training for future career. This should be decided by the resident in consultation with the Residency Progress Subcommittee
(RPS) and the department/organization concerned.
Duration: 2 months.
Contents:
Specifics cannot be determined for each elective rotation. However, the following guidelines should be observed:
1. The discipline should be relevant to Family Medicine
2. The elective could be in one of the clinical or non-clinical rotations related to Family
Medicine.
3. A maximum of two months could be used in the same specialty.
4. Approval of the Residency Progress Subcommittee (RPS) of the elective is mandatory.
Learning Situations:
Should be appropriate to the chosen elective rotation and should be approved by the RPS.
Examples:
•
Sports Medicine.
•
Rheumatology.
•
Diabetes.
•
Child Health Psychiatry.
•
Palliative Care.
•
Radiology.
3. PHC CENTER TRAINING CURRICULUM
A-Curriculum of training at primary health care center for first year:
- Morning: Family Medicine Clinics
- Afternoon: Seminars.
WEEK Subject
1 Concept of PHC and practical training to assess the efficiency of provided services at PHC centre.
2
Concept of family medicine and practical training on recording and referral system.
3,4&5 Health care of children under 5years :
IMCI strategy (including Acute respiratory tract infection (ARI) &Diarrheal diseases (CDD)programs) :Asessement,classification,identification of treatment
& treatment of sick child aged 2months up to 5years:general danger sign &main five symptoms:1)cough or difficult breathing2)diarrhea3)throat problem 4)ear problem5)fever
6&7 IMCI strategy (including neonatal care): Assessment, classification, identification of treatment & treatment of sick young infant aged up to 2months.
8,9&10 IMCI strategy (including growth monitoring program& breast feeding): checking malnutrition&anemia, assessment of feeding of child under 5years, feeding recommendation & counseling about feeding problems &breast feeding problems.
11 IMCI strategy (including immunization program): checking immunization status.
12 IMCI strategy (including preschool vision screening): checking any other problem in children aged under 5years.
13 IMCI strategy Counseling & follow up care for children aged under 5years.
14 School health services& dental health services.
15 Adolescent health maintenance.
16&17 Maternal health care Premarital care, preconception care, antenatal care
(routine Antenatal care, immunization).
18 Antenatal care (specific health problems in pregnancy): morning sickness, anemia, other nutritional deficiencies.
19 Toxemias of pregnancy &gestational diabetes mellitus.
20 Medical diseases in pregnancy : as liver diseases, heart diseases, essential hypertension, thyroid diseases kidney diseases.
21 Congenital infections (as syphilis, toxoplasmosis, germen measles,
CMVinfection, herpes virus infection HIV infection), Tetanus, &Rh status.
22 Prenatal genetic screening& mental preparation.
23 Intranatal & Postnatal care: care of the mother and the newborn.
24 Family planning.
25 Breast self examination program.
26 Women's health: osteoporosis& postmenopausal symptoms.
27&28
Premenstrual syndrome , premenstrual dysphonic disorder, dysmenorrheal
29 Dysfunctional Uterine Bleeding (DUB).
30 Vulvovaginitis and bacterial vaginosis, microbiological swab, cervical abnormalities &cervical smear (PAP smear).
31 Sexually Transmitted Infections (STIs).
32&33
Infertility (male &female infertility).
34&35 Mental Health & sleep disorders.
36&37 Health education program & communication.
38 TB control program including DOTS strategy.
39 Health visitor program.
40 Environmental health.
B-Curriculum of training at primary health care center for second year:
Week Subject
1 Communicable disease (including communicable diseases control program) : Epidemiology of communicable diseases.
2
Respiratory infections : Smallpox, Chickenpox, Measles ,
Rubella, Mumps , Influenza(including swine flu &avian flu) .
3&4 Diphtheria, whooping cough& meningococcal meningitis.
5&6
Intestinal infections: Poliomyelitis, viral hepatitis, acute diarrhoeal diseases.
6&7 Cholera, Typhoid fever, Food poisoning.
8&9 Amoebiasis, enterobiasis, ascariasis, Hookworm infection& schistomiasis.
10 Arthropod born diseases : Malaria.
11 Zoonoses: Viral zoonoses : Rabies, hemorrhagic fever.
12 Bacterial zoonoses : Brucellosis, plague human salmonellosis.
13
Rickettsial zoonoses: Rickettsial zoonoses: Scrub typhus, Murine typhus&
Tick typhus.
14 Parasitic zoonoses: Taeniasis, Hydatid disease, Leishmaniasis
15 Adult health care (including no communicable diseases (NCD) control program: Ischemic heart diseases (Acute ST Segment elevation myocardial infarction& angina).
16 Heart failure.
17 Hyperlipoproteinemia.
18 Hypertension (including screening program of hypertension& Diabetes
Mellitus).
19 Diabetes Mellitus (including screening program of hypertension&
Diabetes Mellitus).
20 Arrhythmias.
21&2
2
Obesity (weight management nutrition).
23 Deep Venous Thrombosis and Pulmonary Thromboembolism.
24 Chronic Obstructive Pulmonary Diseases& asthma.
25 Pneumonia.
26 Other Pulmonary Diseases (restrictive lung diseases, supportive lung diseases &pleural diseases).
27 Esophageal Disorders, Peptic Ulcer Disease.
28 Inflammatory Bowel Disease, Irritable Bowel Syndrome.
29 Thyroid disorders.
30&3
1
Acne, Rosacea, dermatitis, psoriasis, other common dermatologic conditions & common skin cancers.
32 Headache (migraine &non migraine headache).
33 Seizures.
34 Anemia& certain hematologic conditions.
35 Rheumatoid arthritis, osteoarthritis & common connective tissue diseases.
36 Renal disease, enuresis, & urinary tract infections.
37 Fluid &electrolyte disturbance.
38 Breast, Lung, and Brain Cancer Updates.
39 Cancer pain management, palliative care.
40 Travel medicine.
C-Curriculum of training at primary health care center for third year:
Week Subject
1 EMERGENCY AND SPORTS MEDICINE: Treatment of the
Patient in Cardiac arrest
2
3
4
5
Advanced trauma life support.
Diabetic ketoacidosis.
Emergency treatment of abdominal pain in the elderly.
Acute and chronic poisoning.
6 Urticaria and angioneurotic edema.
Fracture management. 7
8 Heat and cold Illness.
Upper extremity injuries. 9
10 Lower extremity: strains and sprains.
11 Low back pain.
12 Acceleration and deceleration neck injuries& concussions.
13 Exercise prescription& female athlete triad.
14 Infectious disease and Sports, Preparticipation Evaluation.
15 GERIATRIC MEDICINE : Elder abuse.
16 Dementia and delirium, Parkinson's disease.
17 Polymyalgia rheumatica and Temporal arteritis.
18 Constipation &urinary incontinence.
19 Polypharmacy and Drug Reactions.
20 Falls.
21 Cerebrovascular accidents.
6
7
8
9
10
22 Diagnostic measures in PHC center : ECG.
23 X-RAY.
24&25 Ultrasound.
26
27
GENERAL SURGERY AND SURGICAL
SUBSPECIALTIES, Acute Appendicitis& hernia.
Biliary tract disease.
28&29 Office surgery.
30 Pancreatitis & Pancreatic Carcinoma.
31
32
Anorectal diseases ,colorectal cancer and other colonic disorders
Ophthalmologic problems.
Renal Stones & prostate Disease. 33
34
35
Ear, nose, and throat problems.
Ulcers.
D-Curriculum of training at primary health care center for fourth year:
Week Subject
1,2,3&4 Problem solving &team building.
5 Behavioral sciences & mental disorders: Depressive Disorders, Bipolar
Disorder& schizophrenia.
Smocking, drugs addiction &alcohol dependence.
Generalized anxiety disorder.
Factitious disorder.
Somatoform disorders.
Panic disorder.
11 Social Phobia, Post-traumatic Stress.
Obsessive compulsive disorder & sexual dysfunction. 12
13
14
Patient use of alternative (Integrative) medicine.
Domestic violence.
15
16
Ethics and responsibilities associated with referrals.
Consultations& How to break bad news.
17&18 Auditing
IN-TRAINING EVALUATION OF THE RESIDENTS (BEFORE FINAL
EXAMINATION)
There are many types of evaluations; the success mark for each evaluation is ≥ 60%.
1End course evaluations :
Each resident will be evaluated by the end of each course by written papers
(consists of short answer questions& MCQ) &clinical examinations as objective
Structured Clinical Examination (OSCE), these evaluations are done by the trainers and supervisors & these evaluations are of two types as the following:
•
End theoretical course evaluations
•
End clinical course evaluations (of the total evaluation for each one of them).
2Ongoing evaluations: This includes continuous evaluation of the resident by his trainers & supervisor through years of engagement of the board. these evaluations are done by special evaluation forms as two types as the following :
•
Special evaluation forms for PHC center training (as shown in the appendix I
,page 77)& the evaluations of the four years are equal to 20% of the total 4 th year evaluations).
•
Special evaluation forms. (Filled by trainer) for hospital training (10% of the total evaluation for each of the first three years) as shown in the appendix II, page 78.
3Preparatory examination: This will be performed at the beginning of fourth year of residency and successes in this exam is mandatory to participate at the final one, it weighs 60% of the total one year evaluation; it consist of the following:
•
Oral exam
•
OSCE
•
Written clinical problems.
4log book evaluation :
At the end of four years of training ,each resident is responsible for presenting a log book includes clinical presentations of 250 cases from the PHC center, also it includes seminars ,clinical meetings, journal clubs & other activities which are done or participated by the resident himself, the log book weighs 10% of the total fourth year evaluation.
5Dissertation project evaluation:
A dissertation project on a selected subject in family medicine should be selected by the resident at the beginning of third year is mandatory as a fulfillment for the final exam, it weighs 10% of the total one year evaluation.
The four years
’
in-Training evaluations are as following :
1.
First year evaluations(weighs 10% of the total 4years in-Training evaluations :
It consists of 1 end theoretical course examination, 2 end clinical course examinations &2 ongoing evaluations by 2special evaluations forms (in hospital
&PHC center training).
2.
Second year evaluations (weighs 20% of the total 4years in-Training evaluations
):
It consists of 2 end clinical course examinations &2 ongoing evaluations by 2special evaluations forms (for hospital &PHC center training).
3.
Third year evaluations (weighs 30% of the total 4years in-Training evaluations ):
It consists of 1 end theoretical course examination, 1 end clinical course examinations (90%) &2 Ongoing evaluations by 2 special evaluations forms (for hospital training (10%) &PHC center training).
4.
Fourth year evaluations (weighs 40% of the total 4years in-Training evaluations ): it consists of 1 Ongoing evaluation by special evaluation form (for PHC center training)(20%), preparatory examination (60%),log book evaluation(10%) & research evaluation(10%).
Resets of the examinations:
A reset is necessary only in a failed trial of the examination. All examinations must be passed for a maximum of three trials (except the preparatory examination for a maximum of two trials) from the sitting of the first examination; otherwise we recommend that a further period of training occurs before resetting the examination.
Content of the Examinations:
The discipline of general practice has few fixed boundaries, being defined as much by what patients elect to present to us as by our own views on the GP's job description. General practice is also constantly evolving, reflecting advances in clinical practice, shifts in social expectation and changes in the political, administrative and fiscal framework.
In devising the content of the examinations, the Panel of Examiners is guided by the following blueprint which describes in general terms the domains of competence required of a contemporary general practitioner:
§ Factual knowledge
§
Evolving knowledge: uncertainty, 'hot topics', qualitative research
§ The evidence base of practice: knowledge of literature, quantitative research
§
Critical appraisal skills: interpretation of literature, principles of statistics
§ Application of knowledge: justification, prioritizing, audit
§
Problem-solving: general applications
§ Problem-solving: case-specific, clinical management
§
Personal care: matching principles to individual patients
§ Written communication
§
Verbal communication: the consultation process
§ The practice context: 'team' issues, practice management, business skills
§
Regulatory framework of practice
§ The wider context: medico-political, legal and societal issues
§
Ethnic and trans-cultural issues
§ Values and attitudes: ethics, integrity, consistency, caritas
§
Self-awareness: insight, reflective learning, 'the doctor as person'
§ Commitment to maintaining standards: personal and professional growth, continuing medical education.
Within each examination a variety of contexts will be examined in order to test an appropriate range and depth. Candidates may find it helpful to consider the various roles the doctor may adopt in the course of ordinary practice, for example:
-Clinician -Family physician -Patient ’ s advocate – Gatekeeper -Resource allocator
-Handler of information -Team member -Team leader -Partner
–
Colleague -Employer
–
Manager -Business-person – Learner -Teacher -Reflective practitioner -Researcher
-Agent and shaper of policy -Member of a profession -Person and individual
Learning Situations
1-The Consultation:
Every encounter with patients is a learning experience. The trainee should utilize these opportunities to improve his understanding of patients, their, clinical problems, diagnostic skills, and management abilities.
2-Morning Activities:
This 45-60 minutes session per day is devoted to the discussion of cases seen by the trainee. It can be conducted at the beginning of the session for the previous day cases or at the end of the morning session. Discussion may random cases or problematic cases (cases that are brought by trainees for discussion).
3-Case Presentation:
The trainer will ask the trainees to present cases for the group.
4-Tutorial and Seminars:
In these sessions the trainee will be actively involved to present, discuss, and give feedback. It can include review of clinical topics, discussion of cases, problem-based sessions and evidence-based medicine practical sessions.
5-Journal Clubs:
In These sessions the trainee will be actively involved to present, discuss, and give feedback about different published medical researches. These sessions should be done at least twice weekly in the hospital or in the PHC centers with the trainers &supervisors.
6- Other Activities: as grand tours &death conferences.
REQUIREMENTS TO FILFULL THE RESIDENCY TRANING
PROGRAM
1-LOG BOOK:
The residents are required to keep a logbook where he/or she will record clinical presentations of 250 cases from the PHC center, also it includes clinical meetings, journal clubs &all procedures and activities. The activities must be dated and categorized to the rotation of the training and whether it was performed or observed by the resident. Participation and attendance in seminars and continuing medical education (CME) activities are also included. Each activity registered in the logbook must be countersigned by the Supervisors.
2-RESEARCH (Dissertation):
Introduction:
The family physician should be able to conduct basic research relevant to
Family Medicine in Oman and write scientific papers. This is important because for his/her future career as a leader in this field of specialty. This includes the formulation of hypothesis, objectives, methodology, analysis and writing the paper.
Duration: Longitudinal component (mainly throughout the 3rd year of the residency program).
Objectives:
At the end of the research the residents should be able to :
1. Identify specific problems to solve.
2. Define the objectives of the project.
3. Critically appraise the medical literature.
4. Describe the methodology.
5. Collect, and analyze the data.
6. Write the findings including a scientific discussion.
7. Utilize these findings.
Content:
Planning followed by data collection can start at the beginning of the third year of the residency program. The resident, under supervision, will divide his time between:
1. Reviewing the literature
2. Writing the protocol
3. Collecting and analyzing the data
4. Writing the Scientific paper
Methods of Instruction:
1. Personal consultation with the supervisor, advisor as well as other experts in the field.
2. Supervised field work.
3. Guided reading and library work.
4. Self-directed learning.
Rules and Regulations:
1. Candidates should be encouraged to think of the research subject(s) as early as possible during the first year of training.
2. An initial proposal on a research subject or more should be submitted to the supervisor for approval.
3. The final report will be composed of nine parts: a. Summary/Abstract. b. Introduction. c. Literature Review. d. Materials and Methods. e. Results.
f. Discussion. g. Conclusion & recommendations. h. References. i. Appendices.
4. The final manuscript should be typed and bound in a hard cover and must be submitted at least two months before the end of the fourth year of the residency program.
Evaluation:
The project will be assessed by two examiners. If the two examiners pass the candidate, he/she will be awarded a
“
Pass
”
grade. If one examiner fails the candidate, the project will be assessed by a third independent examiner.
ADMINSTRATIVE INSTRUCTIONS OF THE RESIDENCY TRANING
PROGRAM
1The resident is allowed to take a usual vacation of not more than 30 days every year of the of the residency training program & If the resident is in need for more than 30 days then the whole training year will be postponed but the resident is not allowed to postpone the 1 st
year of residency training program .
2The resident have the right to have a temporary withhold of his training for maximum of one year if he has an eligible excuse.
3A pregnant resident have the right to have a leave of maximum of three months duration & it should be compensated later.
ADMINSTRATIVE WARNINGS OF THE RESIDENCY TRANING
PROGRAM
1-Primary warning : if the absence of the resident is more than 5% of the whole duration of the of the residency training program
4Secondary warning : if the absence of the resident is more than 10% of the whole training year of the residency program
5Final warning : if the absence of the resident is more than 15% of the whole training year of the residency program
4-Discontinuation of the training of resident: if the absence of the resident is more than 20% of the whole training year of the residency program.
DISCONTINUATION OF THE RESIDENCY TRANING PROGRAM:
1-
If the absence of the resident is more than 20% of the whole training year of the residency program.
2-
If the resident is failed in the whole allowable trials to succeed.
3-
If the resident behaves badly with the supervisors, trainers, colleagues or patients & do not follow the professional rules.
APPENDICES (
SPECIAL EVALUATION FORMS OF THE
TRANING PROGRAM):
APPENDIX I:
RISIDENT MONTHLY EVALUATION FORM AT THE PHC
CENTER
زﻛرﻣﻟا ﻲﻓ ﻲﺑرﻌﻟا دروﺑﻟا ﺔﺑﻠطﻟ ﺔﯾﻣﻠﻌﻟا تﺎطﺎﺷﻧﻟاو ( ﺔﯾدﺎﯾﺗﻋﻷاو ﺔﯾﺿرﻣﻟا ) تازﺎﺟﻷاو تﺎﺑﺎﯾﻐﻠﻟ يرﮭﺷﻟا فﻗوﻣﻟا ةرﺎﻣﺗﺳأ
: ﺔﻧﺳ ﻟا / :
ةرﺳﻷا بط / ﻲﺑﯾردﺗﻟا ﻲﺣﺻﻟا
رﮭﺷﻟا
: ﻲﺣﺻﻟا زﻛرﻣﻟا مﺳأ
: ﺔﻠﺣرﻣﻟا
ةزﺎﺟﻷا ﺦﯾرﺎﺗ
ﺔﯾﺿرﻣﻟا
تدﺟو نإ
ةزﺎﺟﻷا ﺦﯾرﺎﺗ
ﺔﯾدﺎﯾﺗﻋﻷا
تدﺟو نإ
بﺎﯾﻐﻟا ﺦﯾرﺎﺗ
دﺟو نإ
ﺔﯾﻣﻠﻌﻟا تﺎطﺎﺷﻧﻟا بﻟﺎطﻟا مﺳأ ت
:
ﺦﯾرﺎﺗﻟاو ف ِ رﺷﻣﻟا ﻊﯾﻗوﺗ
:
ﺦﯾرﺎﺗﻟاو بﱢردﻣﻟا ﻊﯾﻗوﺗ