BEFORE THE LAB YOU HAVE TO READ ABOUT
advertisement

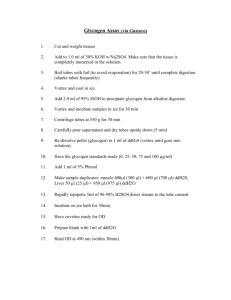
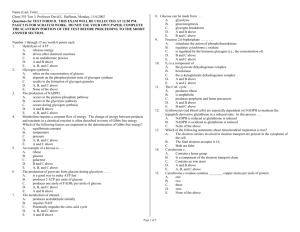
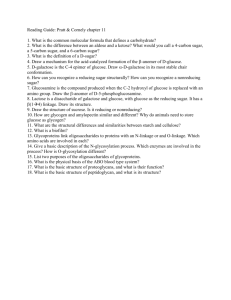
4/6 year 2012/2013 GLYCOGEN GLYCOGEN BEFORE THE LAB YOU HAVE TO READ ABOUT: 1. Glycogen structure. 2. Glycogen synthesis and degradation (reactions with structural formulas and enzymes). 3. The role of glycogen in liver and muscles. INTRODUCTION Glycogen represents the principal storage form of carbohydrate in the mammalian body, mainly in liver and muscles. It is a branched homoglycan composed of α-D-glucopyranose units which are linked via two types of bonds: α-1,4 and α-1,6 (Fig. 1). Its corresponding form in plants is a starch but glycogen is more extensively branched (branches occur every twelve to fourteen glucose residues) and more compact than starch. Glycogen is stored mainly in liver (up to 6-8%) and muscles ( 1%). However, due to the greater mass, muscles contain about three to four times more glycogen than the liver. Glycogen accumulated in liver serves as a reservoir that releases glucose into the blood when the blood glucose level falls below the normal one. Phisiological glucose concentration in blood changes within a narrow interval ranged from 4.4 to 6.7 mmol/l (80-120 mg/dl). Glycogen accumulated in liver is sufficient to maintain glucose concentration on the appropriate level for 12-18 hours. Glycogen’s role in maintaining blood-glucose level is especially important because glucose is the major metabolic fuel for mammals (except ruminants) and a universal fuel for the fetus. Glucose supply is necessary especially for the nervous system and erythrocytes. Glucose is virtually the only fuel used by the brain, except during prolonged starvation. Moreover, the glucose from glycogen is readily mobilized and is therefore a good source of energy for sudden, strenuous activity. Unlike fatty acids, the released glucose can provide energy in the absence of oxygen and can thus supply energy for anaerobic activity. A decrease in the glucose level below 70 mg/dl (hypoglycemia) causes brain dysfunction which can lead to coma and death. CH 2 OH OH -1,4 linkage O CH 2 OH 1 4 O OH OH -1,6 linkage O 1 nonreducing end O OH 6 4 1 OH OH OH 4 1 OH 1 OH O O O HO 4 1 OH O O O O CH2OH CH2 CH2OH CH2OH OH OH Fig.1. Branched structure of glycogen. 1 4/6 year 2012/2013 GLYCOGEN Muscle glycogen is not generally available to other tissues because muscles lack the enzyme glucose-6-phosphatase. Instead of it provides a source of energy for muscle contraction and is a readily available source of glucose for glycolysis within the muscle itself. Glycogen is synthesized from glucose by the pathway of glycogenesis, which occurs mainly in liver and muscle. The glucose donor in the biosynthesis of glycogen is an activated form of glucose uridine diphosphate glucose (UDPGlc). UDPGlc is synthesized from glucose 1-phosphate and uridine triphosphate (UTP) in a reaction catalyzed by UDPGlc pyrophosphorylase. This is a key reaction in glycogen biosynthesis because the energy of the phospho-glycosyl bond of UDPGlc is utilized by glycogen synthase. glucose 1-phosphate + UTP UDPGlc + PPi Glycogen synthase catalyzes formation of glycosidic bonds between C1 of the activated glucose of UDPGlc and C4 of a terminal glucose residue at the non-reducing end of glycogen, liberating uridine diphosphate (UDP) (Fig. 2). O HN HOCH2 O O 1 OH O O O P O P O HO O OH - O O O O + - HOCH2 HOCH2 N 4 OH O HO OH OH O OH OH OH Glycogen (n residues of glucose) UDP-glucose GLYCOGEN SYNTHASE O HN O O O - O P O P O O - O O O HO OH OH UDP 4 1 OH O O O + - HOCH2 HOCH2 HOCH2 N OH OH O O OH OH OH Glycogen (n + 1 residues of glucose) Fig.2. Elongation of a glycogen chain by glycogen synthase. Glycogen synthase can only extend existing chain of glycogen. The “glycogen primer” (known as glycogenin) must be present to initiate glycogen biosynthesis. Glycogenin is a 37-kDa protein, which catalyses the addition of a glucose monomer to one of its own tyrosine residues forming a bond between the C1 of glucose and the tyrosine hydroxyl group. This reaction is due to glycogenin’s glucosyltransferase activity. Further glucose residues can be added to the α1→4 position to make a short chain that is a substrate for glycogen synthase. Glycogenin remains attached to the reducing end of the glycogen molecule. Glycogen synthase cannot make (α1→6) bonds found at the branch points of glycogen. Instead, these are formed by a branching enzyme (amylo[1→4] →[1→6]-transglucosylase). When the chain has been lengthened to at least 11 glucose residues, branching enzyme transfers a part of the α1→4 chain (at least six glucose residues) to a neighboring chain to form an α1→6 linkage, establishing a branch point. The branches grow by further additions of α1→4-glucosyl units and further branching. 2 4/6 year 2012/2013 GLYCOGEN The biological effect of branching is to make the glycogen molecule more soluble and increase in the number of nonreducing ends, which accelerates both synthesis and degradation of glycogen. Glycogen breakdown (glycogenolysis) requires the interplay of the following enzymes: glycogen phosphorylase, debranching enzyme (which has two activities of α-[1→4]→α-[1→4]-glucan transferase and amylo-[1→6]-glucosidase) and phosphoglucomutase. Glycogen phosphorylase catalyzes the phosphorolytic cleavage by adding inorganic phosphate (phosphorolysis) to the α1→4 linkages of glycogen to yield glucose 1-phosphate. The phosphorolytic cleavage of glycogen is energetically advantageous because the released sugar is already phosphorylated. glycogen(n residues) + Pi glucose 1-phosphate + glycogen(n-1 residues) α-[1→4]→α-[1→4]-glucan transferase translocates a trisaccharide unit from one branch to the other, exposing a single glucose residue joined by an α-1,6-glycosidic linkage. Amylo-[1→6]-glucosidase hydrolyzes the release of free glucose breaking an α1→6 bond . Phosphoglucomutase converts glucose 1-phosphate formed during phosphorolytic cleavage of glycogen into glucose 6- phosphate. Further fate of glucose 6-phosphate depends on type of tissue. Liver and kidney contain a hydrolytic enzyme: glucose 6-phosphatase, which converts glucose 6-phosphate to dephosphorylated glucose. The free glucose formed from glycogen in liver is released into the bloodstream and carried to tissues that require it as a fuel. Glucose 6-phosphatase is not present in muscle, so muscle glycogen cannot directly act as a source of blood glucose. Instead, the glucose 6-phosphate is further processed by enzymes of glycolytic pathway. Glycogen is synthesized and degraded by different pathways. The principal enzymes controlling glycogen metabolism (glycogen phosphorylase and glycogen synthase) are regulated by allosteric mechanisms and covalent modifications due to its reversible phosphorylation and dephosphorylation in response to hormones action (glucagon, insulin, epinephrine). Cyclic adenosine-3’,5’monophosphate (cAMP) integrates the regulation of glycogenolysis and glycogenesis by promoting the simultaneous activation of phosphorylase and inhibition of glycogen synthase. Insulin acts reciprocally by inhibiting glycogenolysis and stimulating glycogenesis. EXPERIMENTS 1. Isolation of glycogen from animal liver Principle of the method Glycosidic bonds in glycogen are resistant to hydrolytic activity of OH- at elevated temperature. In contrast, peptide bonds in proteins, ester bonds in lipids and phosphodiester bonds in ribonucleic acids undergo hydrolysis at high temperature and in alkaline pH (i.e. in KOH solution). Under these conditions the glycogen solution, only slightly contaminated with other polysaccharides, fragments of denatured DNA and low molecular weight compounds, can be obtained. Addition of ethanol results in glycogen precipitation and allows to obtain relatively purified glycogen. 3 4/6 year 2012/2013 GLYCOGEN Reagents 1. 30% KOH solution 2. 96% ethanol Procedure Turn on the water bath before experiment! 1. Put one gram of liver into a centrifuge tube containing 2.5 ml of 30% KOH solution. 2. Seal the tube with rubber stopper with a reflux column and put it into a boiling water bath for 30 minutes shaking it from time to time. 3. After complete resolving of the tissue, cool the tube down. 4. Add 4.5 ml of 96% ethanol and shake it vigorously. 5. Seal the tube again with rubber stopper with a reflux column and put it into the boiling water bath. BE CAREFUL! Do not let alcohol evaporate, take the tube out of the water baths as soon as it starts to boil. 6. After cooling, spin down the glycogen precipitate by centrifugation (5 min, 3000 rpm). Before centrifugation, buckets with tubes should be balanced in pairs!!! 7. Discard the supernatant, dissolve the precipitate in 3 ml of water (stir with glass rod). 8. Afterwards, precipitate the glycogen by adding 6 ml of 96% ethanol (stir thoroughly the content of the tube). 9. Spin down the precipitated glycogen as previously described. 10. Discard the supernatant carefully. 11. Dry the precipitate by putting the tube upside down on a filter paper. 12. Dissolve the precipitate in 10 ml of distilled water. The resulting opaque solution of glycogen will be used in experiment 3. 2. Preparation of a calibration curve for glucose determination and quantitative task (individual for each student) Principle of the method Glucose has reducing properties and reduces dinitrosalicylic reagent under alkaline pH conditions, while itself is oxidized to gluconic acid. After reduction, the yellow dinitrosalicylic reagent changes to orange, with a maximum absorbance at 550 nm. The color change is directly proportional to the amount of glucose in the sample. Reagents 1. Glucose standard solution (0.01 mol/l) 2. 0.05 mol/l phosphate buffer, pH 6.9 3. Dinitrosalicylic reagent (1% 3,5-dinitrosalicylic acid, 1.6% NaOH, 30% sodium potassium tartrate) 4 4/6 year 2012/2013 GLYCOGEN Procedure 1. Prepare 9 tubes calibrated for 10 ml. 2. Add 1 ml of given individual task solution (IT) to the tubes 8 and 9. 3. To each of 9 tubes add the reagents in order according to the table 1. Mix carefully every time a new compound is added. PLEASE NOTE that tubes tube 1 is a blank sample, tubes 2-7 are the standard samples for preparation of a calibration curve, , while tubes 8 and 9 contain the individual task for each student. Table 1 Tubes 1 2 3 4 5 6 7 8, 9 1 ml IT Glucose standard solution (0.01 mol/l) H2O 0.05 mol/l phosphate buffer, pH 6.9 Dinitrosalicylic reagent 0.2 0.4 0.6 0.8 1.0 1.2 2.0 1.8 1.6 1.4 1.2 1.0 0.8 1.0 0.5 0.5 0.5 0.5 0.5 0.5 0.5 0.5 2 2 2 2 2 2 2 2 4 6 8 10 12 ? In test tubes you have respectively: moles of glucose in sample 2 4. After addition of reagents shake well the contents of all tubes and heat them in the boiling water bath for 10 minutes. 5. Take tubes out of the bath and cool them down. 6. Add distilled water to the final volume of 10 ml. 7. Shake the tubes carefully and read the absorbance of each sample (tubes 2-7 for calibration curve, 8-9 for individual task) against the blank sample (tube 1) at 550 nm. 8. Draw the calibration curve. Plot the resulting absorbance values versus the amount of glucose [µmoles] in the appropriate samples. 9. Individual task: read the average amount [µmoles] of glucose in your task solution from the calibration curve. Calculate g of glucose in 1 ml of the task solution using molecular weight value for glucose 180 g/mol. 3. Acid hydrolysis of glycogen. Quantification of glycogen content in liver (%) based on the released glucose amount Principle of the method Glycosidic bonds are fairly stable, they can be broken chemically by strong aqueous acids. Glycogen undergoes hydrolysis at 100°C under acidic pH, and if the hydrolysis lasts for a sufficiently long time, the whole amount of glycogen is degraded to free glucose. Reagents 1. 2 mol/l HCl solution 2. 1.2 mol/l NaOH solution 3. Dinitrosalicylic reagent (1% 3,5-dinitrosalicylic acid, 1.6% NaOH, 30% sodium potasium tartrate) 4. 0.05 mol/l phosphate buffer, pH 6.9 5. Glycogen solution from experiment 1 5 4/6 year 2012/2013 GLYCOGEN Procedure 1. Take 5 ml of the glycogen solution obtained in the first experiment, add 5 ml of distilled water and shake it well (dilution 1:1). 2. Prepare 10 calibrated test tubes. 3. Add 0.4 ml of the diluted glycogen to each test tube numbered from 1 to 9, but 0.4 ml of distilled water to test tube 10 (blank sample). 4. Add 0.6 ml of 2 mol/l HCl solution to all tubes and write down the time (to). 5. Immediately neutralize the contents of 1 and 10 tubes by adding 1 ml of 1.2 mol/l NaOH solution. 6. Put the remaining tubes (from 2 to 9) into a boiling water bath. 7. Take out the tubes 2 to 8 from the water bath in intervals of four minutes, and immediately neutralize their contents with NaOH (1 ml of 1.2 mol/l NaOH solution). 8. Take the tube 9 out from the bath after 40 minutes, and neutralize it as described above. 9. Add 0.5 ml of 0.05 mol/l phosphate buffer pH 6.9 to all tubes to obtain the same final pH value. 10. Add 2 ml of dinitrosalicylic reagent. Shake the tubes well to mix content, and put them into the boiling water bath for 10 minutes. 11. Afterwards, take the tubes out from the bath, cool down and add distilled water to the final volume of 10 ml. Mix well again. 12. Read the absorbance at 550 nm against the blank sample (tube 10). 13. Read the amount [µmoles] of glucose from the calibration curve for glucose prepared during experiment 2. 14. Plot the number of µmoles of released glucose (Y axis) versus time of acid hydrolysis of glycogen (X axis). 15. Calculate the amount of glucose [µg] released during complete hydrolysis of the glycogen sample and then, calculate percentage content of glycogen in liver. You should take into account all dilutions of the glycogen preparation obtained from 1 g of tissue and multiply the calculated amount of glucose by 0.9 due to the fact that 162 g of glycogen yield 180 g of glucose (162:180). 6