Red eye
advertisement

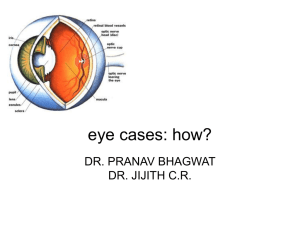
Module II C: 4th year of 3rd Faculty of Medicine S Y L LA B U S SENSORIC DISORDERS Course No 13 Oční klinika 3.LF UK The syllabus, here set forward is only the introduction to the Ophthalmology and brief guide for your easier orientation in main fields in ophthalmology. For recapitulation there are control questions after each chapter. What actually brings the patients to the Ophthalmologist? Most common are the following reasons: 1. 2. 3. 4. 5. unusual eye appearance pain disturbance of visual acuity injury patient is recommended by different medical specialist Unusual eye appearance „red eye“: subconjuctival hemorrhage, conjunctivitis, keratitis, blood in the anterior chamber, iris rubeosis, scleritis or episcleritis etc. „grey cornea“: keratitis, corneal scar, corneal oedema in acute glaucoma, corneal injury, corneal degenerations „grey pupil“: cataract, inflammatory exudate, pupil occlusion „irregular pupil shape “: anterior synechiae, posterior synechiae, acute glaucoma „iris figure“: iris cyst, iris melanoma different eye location: exophthalmus (thyroid eye disease, retrobulbar tumour) enophthalmus ( posttraumatic) different eye position: strabismus „red eye lid, eye lid figure: blepharitis, hordeolum, chalazion, veruca, basalioma pathological eye lid position: entropion, ectropion Pain burning: conjunctival involvement foreign body sensation: erosion, corneal epithelium oedema, corneal or conjunctival foreign body eye ball pain : iritis, iridocyclitis (pain is in association with accommodation) acute glaucoma (propagation of the pain around the eye, nausea) Pain behind the eye and while moved: retrobulbar neuritis Headache and asthenopy: wrong spectacle correction disturbance of visual acuity sudden loss of vision (blindness of the eye): Central retinal artery occlusion Sudden disturbance of visual acuity (floaters, black snow...): vitreous haemorrhage Sudden disturbance of visual acuity (visual field defect – black curtain): retinal detachment Central scotoma: retrobulbar neuritis Blurred vision: acute glaucoma, iritis, keratitis Gradual disturbance of visual acuity: cataract, glaucoma Sudden unset of diplopia: extraocular muscle disturbance Injury Patient history and mechanisms of the injury is very important. Keep in mind that even the perforating eye ball injury with intraocular foreign body can be painless and can be easily missed. Patient is referred by different medical specialist Common questions are: does the patient suffer from: Atherosclerotic or hypertensive retinal vasculopathy, diabetic retinopathy, gynaecologist seeks for gestational retinopathy, neurologist for papilloedena or optic disc atrophy. Main topics Red eye Cataract Glaucoma Pedoophthalmology Diabetes mellitus and the eye Intraocular inflammation Intraocular tumours Age related macular degeneration Trauma Neuroophthalmology Strabismus a amblyopia Refractive errors and its correction Care for handicapped patients Red eye Eye redness is commonly found in so called external eye inflammation (eye lid inflammation, conjunctivitis, keratitis, episcleritis and scleritis) but can be present also in intraocular inflammation (iritis and iridocyclitis). Term Red eye is mostly in association with conjunctivitis and hyperaemia of conjunctival vessels. We call this conjunctival injection. Main reasons for red eye are: Mechanical conjunctival irritation: smoke, foreign body, dusty environment etc. Eye lid inflammation: hordeolum (stye) chalazion blepharitis (Blepharitis squamosa, Blepharitis ulcerosa) Abscess and phlegmona of the eye lid Viral infection: (herpes simplex, herpes zoster ophthalmicus) allergy (drug allergy, pollen allergy etc.) Conjunctivitis: Conjunctivitis is presented by eye redness (Conjunctival vessels hyperaemia, burning itching, send in the eyes sensation, watery eyes, secretion (serous, mucous, purulent, mucopurulent). Conjunctival injection (hyperaemia) is mostly superficial. On the tarsal conjunctiva following features can be found: follicular and papillary reaction, membranes, pseudomembrans, and subconjunctival haemorrhage). Cornea, eye lids, episclera and sclera can be also affected. Treatment differs according to the type of conjunctivitis. Mostly is only local (antiseptic drops, antibiotic and steroid drops and ointment). Systemic treatment is needed less often. Eye with conjunctivitis should not be covered. Infectious conjunctivitis: Bacterial (Streptococcus pneumonia, Haemophilus influenzae, Staphylococus aureus) Viral (adenoviral keratoconjunctivitis, herpes simplex conjunctivitis ) Chlamydia (Chlamydia trachomatis) New born conjunctivitis (Neisseria gonorrhoe, Herpes simplex virus) Conjunctivitis caused by immunological defects Allergical conjunctivitis (drug induced conjunctivitis, vernal keratoconjunctivitis, keratoconjunctivitis, atopic keratoconjunctivitis) Conjunctivitis in cutaneous blistering diseases (Ocular cucatricial pemphigoid, Stevens-Johnson syndrome et. al.) Other conjunctivitis gigantopapillar (keratoconjunctivitis e rosacea, conjunctivitis in Reiter syndrome) Keratitis Infectious keratitis Bacterial keratitis (Staphylococcus aureus, Staphylococcus epidermidis, Streptococcus pneumonie at. al). Clinically presented by the red eye, pain, drop of visual acuity, mixed injection and corneal infiltration is presented. Keratitis can progress to the corneal ulcer with risk of corneal perforation. Therapy: In infectious keratits antibiotics are use. According to the state of infection local or general treatment is performed. For local treatment eye drops, ointment or subconjunctival injection is used. Mydriatics are used to prevent posterior synechiae formation and to reduce the pain. Eye is covered by dressing. Acute corneal transplantation – keratoplasty – is indicated in extreme corneal thinning or in corneal perforation. Viral keratitis (Herpes simplex virus, Herpes zoster ophthalmicus) Therapy: virostatics, corticosteroids, mydriatics Mycotic keratitis (Candida albicans, Aspergillus, Fusarium) Therapy: natamycin 5% drops, amfotericin B 0,2%, mydriatics Non-infectious keratitis Non-infectious keratitis and corneal ulcers are in association with immunological defects or as a part of systemic disease (Mooren´s ulcer, interstitial keratitis in tuberculosis, mononucleosis, herpes simplex, herpes zoster or rubeola infection). Neurological defects can also course noninfectious corneal diseases (neurotrophical keratits, exposure keratitis etc.) Inflammation of episclera and sclera Episcleritis Episcleritis is benign frequently recidiving disease and is presented by bright red eye. Superficial hyperaemia is sectorial or diffuse or localised in place of nodular inflammation. The eye is painful while touched. The most effective treatment seems to be NSAID. Scleritis Scleritis is a serious disease commonly in association with systemic diseases. Hyperaemia is deep, colour is dark red. Eye is very painfull, slight protrusion and motility restriction can be presented. We distinguish between nodular, diffuse and necrotizing form. Necrotizing scleritis can lead to eye ball perforation or even to the eye loss. Diffuse and nodular forms are treated with NSAID, corticosteroids and in recidiving disease by immunosuppressant. Necrotizing form is treated with immunosupresion and corticosteroids. Differential diagnosis – red eye Visual acuity IOP injection uveitis dropped acute glaucoma dropped acute conjunctivitis normal slightly decreased ciliary over 40 mmHg passive hyperaem. normal or increased normal conjunctival Epiphora increased pain by accomodation Cornea smooth, endothelial precipitates normal depth, cells and flare in the fluid active congestion, decolouration, oedema normal – mioticirregular) Anterior chamber iris Pupil intraorbital propagation and hemicrania epithelial oedema Increased ↑↑ burning, itching passive congestion smooth, epithelial microdefects normal depth normal oval semimydriatic normal narrow Control questions: 1.Which of the following disease does NOT cause red eye : A) cataract B) corneal erosion C) acute iridocyclitis D) acute conjunctivitis 2.Clinical appearance of acute iridocyclitis does NOT contain: A ) drop of visual acuity B ) decrease of intraocular pressure C ) superficial (conjunctival) injection D ) eye pain 3.The most common course of the red eye is: A) glaucoma B) trauma C) external eye inflammation D) acute iridocyclitis 4.Which of the following diseases is presented by the deep injection end eye pain, commonly in association with systemic disease (even life threatening)? A) episcleritis B) scleritis C) cataract D) conjunctivitis Cataract Cataract is one of the most common causes for blindness worldwide (tab. No.1). Based on data provided by WHO (World Health Organization) there were 38 million blind people in the world in 1990, 42 % from it because of cataract (Tab No.2). Cataract surgery is in the population of people older then 65 years the most common surgery in developed countries. Cataract can by either acquired or congenital. According to the causation of cataract development we recognize senile, posttraumatic and post radiation cataract, cataract in systemic diseases (e.g. diabetes mellitus, galactosemia, myotonic dystrophy), cataract in dermatologic diseases (e.g. atopic dermatitis, ichthyosis), in diseases of central nervous system (e.g. neurofibromatosis) and other ophthalmic diseases (glaucoma, uveitis, tumours, retinitis pigmentosa, degenerative myopia, retinal detachment, ciliary’s body tumours i.e.) Cataract very often develops as a result of toxic activity of drugs (corticosteroids, antimalaric drugs, Amiodaron). Congenital cataract can manifest in early childhood or in older age. It is very often connected with systemic diseases (myotonic dystrophy, Down syndrome, Edwards’s syndrome). Infantile cataract is described as a congenital lens opacification or an early postnatal cataract. Its incidence is 0,4 % in newborns. The cause of infantile cataract is mostly a viral disease of mother in the first trimester of pregnancy (rubella, toxoplasmosis) or toxic activity of drugs, which the woman took in early stages of pregnancy (e.g. corticosteroids). The aetiology of more then 1/3 congenital cataracts is unknown. The development of senile cataract is a multifactorial process. The merits of cataract development are biochemical changes. Genetic and socioeconomic aspects are playing also an important role in the development of senile cataract. The main risk factor is the age. While the incidence of cataract in the age of 50 and less is rare, the incidence in the eighties is 50%. The next important risk factor is the gender. Genetic predisposition was also proved. There is a greater risk of cataract in nutrition deficits and obesity. Sufficiency of proteins, vitamins and other antioxidant substances in the nutrition are in the case of cataract development protecting factors. Higher incidence of cataract was proved in patients with systemic diseases, diabetes mellitus, hypertension etc. There are also some drugs with cataractogenic effect, e.g. corticosteroids, cholinergic miotics, diuretics, chemotherapeutics etc. Recently a great attention is paid to the effect of UV radiance higher then 295 nm, which is absorbed by the crystalline lens. It was experimentally proven, that high doses or a long exposition of UV radiance could affect cataract development in animals. Also alcoholism and smoking are risk factors. Crystalline lens opacification is accompanied by decrease of visual acuity and change in visual functions. Visual acuity can be decreased up to light projection. Patients complain about aggravation of visual acuity in sunlight or during night driving. Defects in colour sense or visual field are also quite common. Every aggravation of visual acuity, which annoys the patient in the work or private life, is an indication for surgical treatment. The criteria for surgical treatment differ in every single patient. Nowadays the most common operation technique in cataract removal is facoemulsification. Ultrasound in frequency of 30 kHz is used in facoemulsification. Destruction of the nucleus is performed mechanically, by vibrations of the ultrasound needle, cavitation effect and finally by acoustic waves, that are distributed through the fluid medium. The ultrasound needle penetrates the eye through a corneal or scleral incision. After removal of the nucleus and other crystalline lens masses, an artificial intraocular lens is implanted into the capsular bag. The most modern intraocular lenses are made from soft materials, they are foldable and can be implanted through a 2,8 – 4,0mm incision. Current cataract surgery is mostly an ambulatory procedure under topical anaesthesia. The small incision and implantation of a soft intraocular lens makes a fast visual rehabilitation possible. Due to rapid evolution of technological processes in construction and production of instrumentation and changes in implantology, cataract surgery becomes a safer procedure. In the future we can expect miniaturization of the needle and implementation of injectable implants, which will enable high-quality recovery of visual acuity including accommodation of the eye. Control questions: 1. The most common operation technique in cataract removal in present time is: a. ECCE b. facoemulsification c. trabeculectomy d. ICCE 2. Posterior subcapsular cataract can cause: a. decreased near visual acuity b. myopisation c. monocular diplopia d. presbyopia 3. The most common anaesthesia in uncomplicated cataract surgery in present time is: a. local b. general anaesthesia c. retrobulbar d. topical 4. For the calculation of the implanted intraocular lens is important to know: a. keratometry and axial length of the eye b. preoperative spectacle correction c. intraocular pressure d. pachymetry 5. In nuclear cataract the most opacification is in: a. the centre of the crystalline lens b. the periphery of the crystalline lens c. near the posterior pole d. under the anterior capsule 6. Nuclear cataract can cause: a. changes in the refraction – myopisation b. monocular diplopia c. decreased near visual acuity d. decreased visual acuity Glaucoma Glaucoma is a group of affections which are characteristic by progressive chronical neuropathy of ocular nerve which is irreversible. Changes in visual field are one of typical signs. Primary glaucoma usually involves both eyes, but the severity of impairment of each eye may be different. Secondary glaucoma occurs as a consequence of some other eye disease, so it is often unilateral. If glaucoma is not diagnosed of properly treated it can proceed into blindness of the eye. Glaucoma is 2nd to 3rd most common reasons of blindness in the world and the disease involves 2-3% of all people older than 40 years. Main risk factors of disease are: higher intraocular pressure (IOP), age, race and genetic factors. Other risk factors are insufficient vascular nutrition of optical nerve disc, long lasting hormone treatment and neurological diseases. In clinic praxis there are two forms of glaucoma: Primary open angle glaucoma POAG (glaucoma simplex), this form is presented by 80% of all glaucomas. More accurate classification is: 1) Primary juvenile glaucoma (in patients from 10-35 years old) 2) POAG with high intraocular pressure POAG with low IOP Ocular hypertension syndrome By POAG the physical findings on the eye- i.e. appearance of eye globe is quite normal, development of pathologic changes is slow and often asymmetric. Patient event doesn´t have to know about the developing changes. By high pressure glaucoma (average IOP in our population is 16 mmHg) there is problem in outflow of ocular fluid throughout of ocular anterior chamber- angle meshwork toward the duct of Schlemm and by this mechanism there is a constant increasing of IOP. When these changes are slow, they are compensated by patient and such impaired person often doesn´t realize these changes. In this case there is a typical glaucomatous papilla: disc excavation which is sometimes accidentally diagnosed for instance at ophthalmologist during the exam for glasses correction. If there are any changes on papilla, they usually correspond to visual field changes. Typical changes on papilla and on the visual field are also found in patient with low pressure glaucoma (normal pressure glaucoma). These changes are caused probably by decreased perfusion of optical disc region. There is also a group of patients who have mild elevation of IOP – like 21 mmHg, but they still have normal papilla findings and also the visual field is normal. This one can be ocular hypertension. These patients are not necessarily treated, but they should be observed to check any further changes on papilla or in the visual field. Primary angle closure glaucoma (PACG) is present in approximately 1/5 of all patients. We can distinguish acute, chronicle or subacute form of the disease. This form of glaucoma usually appears in small hyperopic eyes with shallow anterior chamber and narrow anterior chamber angle. During patient life the iris diaphragm is pulled by increasing volume of crystalline lens anteriorly and by this anterior chamber angle becomes more tight - narrow. By mydriasis (dark places, pharmacologic induced, stress) the iris and anterior part of lens came into a contact and this can cause pupil block. The aqueous humour accumulates behind iris and pulls the iris root anteriorly towards to the trabecular meshwork in anterior chamber angle. This makes outflow of intraocular fluid impossible and intraocular pressure increases dramatically. In prodromal phase there is blurred vision, patients can see ”irisation”, which means colour circles around spot sources of light, patients can feel pain in the eye or headache. These symptoms usually diminish spontaneously. With progress of changes these attacks are usually longer and more intensive, intervals between attacks are shorter. These prodromal problems can result in fully developed acute glaucoma attack. For this a prompt and high elevation of IOP is typical. The patients have a pain in the eye, they can have a severe headache, they have nausea and even vomiting is not uncommon. Another symptoms: bradycardia and sweating. Eye globe is painful, hyperaemic, there can be corneal epithelial oedema with appropriate loss of visual acuity. Anterior chamber is shallow, iris with hyperaemia, pupil has irregular shape and may be little dilatated. There is poor light reaction of the pupil. This angle closure glaucoma is urgent ophthalmic state and it may cause loss of vision of affected eye within several hours or days. Treatment consists of decreasing production of the aqueous humour, than we should apply miotics to liberate outflow through iridocorneal angle and also we have to calm down the patient. In the case of gonioadhesions (irreversible findings), we speak about chronic glaucoma. Glaucoma treatment: The aim of glaucoma treatment is to preserve visual function and to hold quality of life. The treatment should be multifactorial, aggressive and safe and without any adverse affects. There is also a question of cost effectiveness. That is why we have to think about the type of glaucoma, risk factors and target intraocular pressure when choosing appropriate treatment. Requested target intraocular pressure (IOP) depends also on the progression of disease and another factor is expected length of life of the patient. Treatment is always highly individual. We can divide treatment in 1) medicaments - local or systemic 2) laser treatment and 3) surgical treatment. Nowadays we use these groups of medicines for local treatment: Intraocular fluid Secretion outflow TM outflow US Sympatomimetics non-selective selective epinephrine d-EPIFRIN clonidin ARUCLONIN brimonidin ALFAGAN + + + + + Sympatolytics non-selective timolol TIMOLOL levobunolol VISTAGAN beta selective bataxolol BETOPTIC + + + with internal sympatomimetic activity carteolol ARTEOPTIC + Parasympatomimetics pilocarpine PILOCARPINE PILOGEL ung. Carboanhydrase inhibitors (ICA) local systemic dorsolamid TRUSOPT brinsolamid AZOPT acetazolamid DILURAN + + + + + Prostaglandins docosanoids unoproston RESCULA latanoprost XALATAN travoprost TRAVATAN + prostamides bimatoprost LUMIGAN + Control questions: 1) What is glaucoma? - increased IOP - visual field changes - chronic progressive neuropathy of II. cranial nerve - changes in blood supply for II. cranial nerve 2) How we treat glaucoma nowadays? - enucleation of the globe - reaching of requested IOP - by eye drops - by laser 3) Main risk factors for glaucoma are: - age, sex, genetic factors - age, race, , genetic factors, increased IOP - refractive error, increased IOP, sex - blood circulation disorders, age, genetic factors, sex 4) Other risk factors for glaucoma are: - IOP (intraocular pressure) - blood supply, vascular insufficiency - age and race - genetic factors 5) Glaucoma is classified according - direct ophthalmocsopy + other imaging methods - gonioscopy - tonometry - perimetry 6) Target intraocular pressure during glaucoma treatment is: - 23 mmHg - 12 mmHg - is the same like average pressure in healthy people - individual 7) Clinical finding in POAG - normal outer appearance of the eye, glaucomatous papilla of n. II - shallow anterior chamber, normal papilla n. II appearance - shallow anterior chamber, glaucomatous papilla of n. II (excavation op the disc) - deep anterior chamber, normal appearance of papilla n. II 8) Clinical findings in PACG - deep anterior chamber, glaucomatous papilla of n. II (excavation op the disc) - shallow anterior chamber, normal papilla n. II appearance - shallow anterior chamber, glaucomatous papilla of n. II (excavation op the disc) - deep anterior chamber, normal appearance of papilla n. II + + + 9) Incidence of glaucoma - in 2% of people aged over 40 years - in 1% of people over 40 years - in more than 2% of people aged over 40 years - only in white race 10) Acute glaucoma attack - nausea, vomiting, conjunctival hyperaemia, corneal oedema, shallow anterior chamber, narrow pupil - nausea, vomiting, conjunctival hyperaemia, corneal oedema, shallow anterior chamber, dilatated pupill - nausea, vomiting, conjunctival hyperaemia, corneal oedema, deep anterior chamber, narrow pupil - nausea, vomiting, conjunctival hyperaemia, corneal oedema, deep anterior chamber, dilatated pupil Paediatric ophthalmology The ocular perception is not inborn, but it is a developing process since the birth of child. The function of vision could be affected negatively already during the birth. These are principal groups of diseases: 1. Retinopathy of prematurity 2. Congenital eye defects 3. Congenital intraocular infections 4. Intraocular tumours 5. Congenital glaucoma 6. Ophthalmia neonatorum Retinopathy of prematurity (ROP) Retinopathy of prematurity is a proliferative retinopathy which affects pre-term infants exposed to high ambient oxygen concentration. The disease begins as an abnormal vasoproliferation in the retina of a premature infant. With progressing disease, fibroglial proliferation may occur in the retina and vitreous with the possibility of retinal traction or detachment. Dangerous factors: Weight birth fewer than 1500 gm. Childbirth before 32nd week of gestation age 90% ROP heals up spontaneously, but the rest of the children have serious functional defects. Congenital eye defects These are principal groups. Anophthalmos – this is a rare condition in which one or both eyeballs are absent or rudimentary. Microphthalmos- one or both eyes are markedly smaller than normal. Many other ocular abnormalities may be present (e.g. cataract, glaucoma ..).The vision could be poor. Abnormalities of corneal size and shape – dysgenesis mesodermalis corneae and iris includes posterior stromal defect with leucoma and iris adhesions to leucoma. The vision is very poor if any. Coloboma of the iris indicates incomplete closure of the foetal ocular cleft and usually occurs bellow. All these anomalies might be together combined and are influencing function of sick eye according to the level of damage. Congenital intraocular infections Congenital choriorethinopathy are combined with congenital eye defects (microphthalmos and cataract) and other organs defects (heart and central nervous system). The most dangerous are the first 3 months of gestation. Etiology: TORCHS (toxoplasmosis, rubella, cytomegalovirus, herpes virus and syphilis). Changes of the eye have very difficult treatment connected with the treatment of the systemic diseases. Intraocular tumours The most common intraocular malignancy in childhood is retinoblastoma. Retinoblastoma is occurs between 1/14 000 and 1/20 000 live births. The age at the time of diagnosis averages 18 months of life. Retinoblastoma occurs in both genders and in 30 – 35% is bilateral. Only 6% of patients have a family history of the tumour, which is bilateral tumour. Sporadic cases constitute 94 % of all case of retinoblastoma. In this case is the tumour mostly unilateral, rarely might occur bilateral. The typical clinical symptoms are either leukocoria („white pupil“) or acute strabismus or decreased vision. The treatment of unilateral retinoblastoma is enucleation. The treatment of bilateral tumours is enucleation in case of the worse eye and the radio-, chemo- or cryo therapy in case of the better eye. Exceptionally, in vital indications, it is necessary to perform bilateral enucleation. Congenital glaucoma Congenital glaucoma can be defined as a form of increased intraocular pressure. It arises by inborn occluding of the chamber angle. Clinical findings: The earliest and most constant symptom is epiphora. Later symptoms include increased corneal diameter (megalocornea) and epithelial oedema and opacity of the corneal stroma. Treatment: 1. Surgical procedure: trabeculotomy and trabeculectomy 2. Medical treatment: beta-blocators In untreated cases, blindness occurs early. Ophthalmia neonatorum Ophthalmia neonatorum or conjunctivitis of the newborns is any inflammation or infection of the conjunctiva in the newborn. The time of onset is an important factor for diagnosis. Etiology: 1) Gonococcal conjunctivitis: Its onset is from 2nd to 5th day. The main complication is the corneal ulcer. The blindness used to be 10 %. 2) Chlamydial and herpes conjunctivitis: Its onset is from 5thto 14th day. Chronic pulmonary diseases are the late complications of untreated chlamydial ocular infection. Treatment of chlamydial infection include macrolid antibiotic per os. Local application is insufficient. The keratitis and encephalitis are the early complications of herpes ocular infection. Control questions: 1. The most common intraocular malignancy in childhood is A) Carcinoma of the lacrimal gland B) Chorioidal melanoma C) Retinoblastoma D) Basal cell carcinoma of the eyelids 2. What does the ROP abbreviation mean? A) Congenital toxoplasmosis B) Retinopathy of prematurity C) Increased intraocular pressure D) Viral keratitis 3. Photophobia, epiphora and increased corneal diameter (or corneal oedema) in infants are characteristic symptoms for A) Obstruction of the nasolacrimal system B) Conjunctivitis C) Congenital glaucoma D) Retinoblastoma 4. Exotropia is A) Convergent strabismus B) Divergent strabismus C) Pseudostrabismus D) Vertical strabismus 5. Amblyopia is A) Lazy – eye blindness B) Sight old -age C) Squint D) Farsightedness Diabetes mellitus Diabetic retinopathy is a late organ complication of diabetes mellitus, appearing after 10-20 years duration of diabetes. In civilised countries is one of the most frequent reasons of blindness. 5% of diabetics are blind through diabetic retinopathy. Diabetic retinopathy rise on the strenght of microangiopathy. Creation of microaneurysms, obliteration of capillaries, failure of perfusion and resulting hypoxia of the retina rise by reason of damage of capillaries wall. Ophthalmologic finding: 1. microaneurysms 2. phlebopathy 3. haemorrhages 4. soft cotton-wool spots 5. hard exudates 6. macular oedema 7. neovascularizations Types of diabetic retinopathy: 1. Nonproliferative diabetic retinopathy /NPDR/about 90% of diabetic retinopathies, slow progression, low degree of risk for blindness. Decrease of vision is mostly caused through diabetic maculopathy. Characteristic is diabetic microangiopathy and focal changes without neovascularization. 2. Proliferative diabetic retinopathy /PDR/ For this form are characteristic fibrovascular proliferation/ retinal neovascularization or optic disc neovascularization / between retina and vitreous. Complication of PDR is: vitreous haemorrhages /haemophthalmus/, tractive detachment of retina and glaucoma, caused by neovascularization of iris in angle of the anterior chamber. About 50% of patients get blind. Therapy: Very important is prevention: good compensation of diabetes mellitus and periodical examination of eye ground. Basis of therapy is laser photocoagulation/argon or diode laser/ focal or panretinal laser photocoagulation. By complication of PDR we perform an operation – pars plana victrectomy/PPV/- removing of haemophthalmus, removing of epiretinal membrane, tamponade of retinal detachment by gas or silicone oil, endolaserphotocoagulation. Very important is close cooperation between eye doctors and diabetic doctors. Control questions: 1. Fluorescent angiography is used by disorder: a) retina b) cornea c) conjunctiva d) lens 2. Resolution of optic coherence tomography is: a) 0,8um b) 8um c) 80um d) 800um 3. Diabetic retinopathy divide into: a) nonproliferative b) proliferative c) diabetic maculopathy d) all is right 4. Findings by nonproliferative diabetic retinopathy: a) optic disc neovascularization b) retinal neovascularization c) tractive retinal detachment d) retinal haemorrhages 5. Part of therapy of diabetic retinopathy is: a) brachytherapy b) refractive surgery c) control of diabetes mellitus et risk factors d) partial perforating keratoplasty Intraocular inflammations: Intraocular inflammation can affect either the whole uvea – panuveitis, anterior part of uvea – anterior uveitis, intermedial pars (pars planitis, vitritis, peripheral chorioiditis etc.) or posterior part of uvea - posterior uveitis (chorioiditis, chorioretinitis). From the pathological point of view uveitis can be divided into granulomatous and nongranulomatous inflammation. From the etiological point of view uveitis is divided into exogenous and endogenous. Endogenous uveitis: Uveitis in association with systemic diseases (tuberculosis, sarcoidosis) Parasital infection (toxocarosis) Viral infection (Herpes simplex, Rubeola virus) Mycotic infection (Candida) Idiopatic uveitis Uveitis is also divided into acute and chronic (longer than 6 weeks). Anterior uveitis: For anterior uveitis is characteristic: Ocular pain Photophobia Ciliar injection Changes in iris structure and colour Corneal precipitates, inflammatory exudates in the anterior chamber, hypopyon Posterior synechiae Narrow pupil, slow photoreaction Lower intraocular pressure due to lower production of the intraocular fluid (IOP can be also normal or later higher – secondary glaucoma) Therapy: Mydriatics, steroids (drops, ointment, parabulbar injection, tablets) In the case of apparent aetiology causal therapy is indicated – e.g. Virostatics Posterior uveitis During inflammation of posterior uvea tract visual acuity is always impaired and scotomas and distortions of vision are present. The onset is slow, vitreous opacities are present. For chorioiditis grey-yellow lesions are typical. Very often the inflammation involves also retina – chorioretinitis. The lesions are healed by chorioretinal scar. Therapy depends on etiology Sympathetic ophthalmia Special attention should be payed to sympathetic ophthalmia. It is a chronic granulomatous bilateral inflammation of uveal tract that develops weeks to months after perforation of one eye. The injured eye has after perforation mild chronic inflammation. The first sight of the inflammation in the fellow eye is usually anterior uveitis with corneal precipitates. It is an autoimmune process with not very clear pathophysiology. Treatment includes immunosupression and in some cases enucleation of the injured eye Panuveitis Panuveitis is characterised by inflammation of the whole uveal tract – sarcoidosis, tuberculosis, toxoplasmosis, sympathetic uveitis … Endophthalmitis Endophthalmitis is a very severe inflammation of intraocular structures. Exogenous endophthalmitis (postoperative or posttraumatic) is more often than endogene endophthalmitis (infection reaches the eye structures by blood stream). Sometimes the endophthalmitis is not caused by infectious agens only, or else for example by leaving lens cortex in the eye– sterile endophthalmitis. Endophthalmitis is accompanied by drop of visual acuity, hypopyon, vitritis, and pain. Infectious endophthalmitis is treated by pars plana vitrectomy with application of antibiotics intravitrealy and intravenously. Sterile endophthalmitis is treated with steroids. Inflammation of the optic nerve – optic neuritis Optic neuritis can be divided by localisation into: Intraocular neuritis – inflammation is located in the optic nerve disc Retrobulbar neuritis - inflammation is located in the optic nerve behind the disc Optic neuritis can be further divided into: Acute (developed in few hours) Chronic (slow course – weeks to months) Clinically optic neuritis is accompanied by dull pain behind the eye, sudden severe drop of vision with central scotoma, sometimes temporary amaurosis. Ophthalmoscopically papillary oedema is present only in intraocular neuritis, not in retrobulbar neuritis. It is almost always unilateral. Inflammation of the optic nerve affects mostly young adult persons. The most common cause of optic neuritis is multiple sclerosis. Other optic neuritis are parainfectious or postinfectious. Therapy of optic neuritis due to multiple sclerosis is always in cooperation with neurologists. Intravenous application of steroids is often used. Control questions: 1/ Anterior uveitis is inflammation of: a) conjunctiva b) iris and ciliary body c) chorioid and retina d) cornea and iris 2/ Posterior synechies by uveitis are: a) adhesions of eyelids b) adhesions of iris et cornea c) adhesions of tarsal et bulbar conjunctiva d) adhesions of iris et anterior site of lens 3/ Symptom of neuritis are not: a) blunt pain behind the eye b) mucopurulent secretion c) sudden and deep decrease of sight d) central scotoma 4/ The most frequent causation of neuritis by young adults is: a) tuberculosis b) toxoplasmosis c) sclerosis multiplex d) varicella zoster virus Intraocular tumours Uveal malignant melanoma Incidence of uveal malignant melanoma is 5-7 cases per 1.000.000 people. In 80%, the uvea is forfeited, in 5-8% the iris is lost and in 10-15% the corpus ciliare is lost. Most cases are occurring in people over 50 years in age. Risk factors are: uveal nevus, neurofibromatosis, congenital intraocular melanocytosis. Clinical manifestation depends in localization of the tumour. Melanoma in iris and corpus ciliare can exist without any clinical symptoms for a long time and usually is diagnosed randomly during routine eye exams for some other reason (e.g., eye glass prescription). In other cases, melanoma is diagnosed in the course of complications like retina detachment, secondary glaucoma and cataract. Patients with melanoma of the uvea remains long time without any symptoms, others develop decreased vision, visual field changes and fotopsy. Malignant melanoma of iris This kind of tumour can be diffuse of nodular. Diagnosis is usually depends on the strength of growth and vascularisation of the tumour. In differential diagnosis, we have to consider cyst of iris, nevus of iris and juvenile xantogranulomatosis. Iridectomy or iridocyclectomy is indicated for smaller tumours. For digger ones, enucleation must be considered. Malignant melanoma of corpus ciliare Dilatation of scleral vessels in correspondent quadrant can often be present in this kind of malignant melanoma as well as lenticular astigmatism caused by pressure on lens due to tumour growth. Other symptoms include decrease intraocular pressure, sub/luxation of lens and unilateral cataract. During checkups, we often find a pigmented nodular tumour growing in the direction of the lens and anterior chamber of the vitreous. Much rarer is a diffuse type of malignant melanoma (ring melanoma). In differential diagnosis we have to consider cysts and intraocular inflammation. Malignant melanoma of choroid This type of melanoma is manifested as pigmented or amelanotic formation in different sizes usually in a semispherical shape. After break of Bruch membrane tumour forms typical mushroom-shape. Complications are vitreous bleeding; disperse pigment cells in vitreous, retinal detachment, secondary glaucoma etc. Malignant melanoma of choroid can grow extrascleraly. In differential diagnosis, we have to consider retina nevus, haemangioma, metastatic tumours and posterior scleritis. Examination procedures are biomicroscopy, gonioscopy, opthalmoscopy, fluorescein angiography, sonography, nMR and computer tomography. Treatment depends on size, localization, shape of the tumour, visual acuity; age and status of the patient. We consider radiotherapy (brachytherapy, teletherapy), photocoagulation, diathermy, cryotherapy, local resection of the tumour, enucleation or exenteration of the orbit Control questions: 1. The most important examination to determinate tumour size is: a) RTG b) CT c) Sonography with 10 MHz sonde d) MRI 2. This intraocular tumour does not belong among malignant intraocular tumours: a) retinal astrocytoma b) hypertrophy of retinal pigment epithelium c) choroid haemangioma d) all of them does 3. The most frequent malignant intraocular tumour in adult age is: a) metastasis carcinoma b) uveal malignant melanoma c) retinoblastoma d) choroidal haemangioma 4. A choroidal haemangioma can be part of: a) Sturge-Weber syndrome b) neurofibromatosis c) Tuberal sclerosis d) Von Hippel-Lindau syndrome 5. Uveal melanoma can be treated with: a) brachytherapy b) Lekssell gamma knife c) enucleation d) all answers are correct Age-Related Macular Degeneration Age-Related Macular Degeneration (ARMD), formerly known as senile macular degeneration, is the leading cause in visual loss in people residing in the western world over 50 years in age. In early stages, we can find macular druses and/or retinal pigment epithelium cells displacement during opthalmoscopy examination with clinical response in decreased visual acuity, metamorphopsy and central scotoma. ARMD can be subdivided into atrophic (characterized by hard druses) and neovascular (characterized by retina elevation in macular area) subtypes. Atrophic ARMD is much more frequent (88% cases), neovascular subtype results within few months in practical visual loss in most cases and constitutes 88% cases of practical blindness. The only known proven therapeutical method of neovascular ARMD remains photodynamic therapy with Verteporphin (PDT). PDT decreases the risk of loss of visual acuity by 3 lines of ERDTS in two years two times as compared with a group of patients without treatment. This method consists in i.v. application of photosensitive substance (Verteporphin), which is selectively absorbed in neovascular tissue. Exposure of laser radiation of 689 nm wave-length leads in coagulation cascade, thrombosis and neovascular tissue damage. Control guestions: 1) Age-Related Macular Degeneration (ARMD) is leading cause of acquired loss of visual acuity among people over: a) 35 years b) 40 years c) 45 years d) 50 years 2) ARMD concerns: a) macula b) optic nerve c) retinal periphery d) sclera 3) The first symptom of neovascular ARMD can be: a) bitemporal hemianopsy b) amaurosis c) metamorphopsy d) enlargement of reading distance („short hands“) 4) Prognosis of a) b) c) d) Neovascular ARMD without treatment is: good bad within 10 years bad in several month bad within 5 years 5) The only proven known method of neovascular ARMD is: a) Thalidomide b) photodynamic treatment with Verteporphin c) electronic chip implantation d) retinal transplantation Traumatology of the eye Ocular traumas can be divided by origin into mechanical, electrical, thermal and chemical ones. The orbit is often involved too. Most frequent mechanical ocular traumas are: corneal or conjunctival erosion; recurrent corneal erosion; non-perforating conjunctival, corneal or scleral injury; perforating conjunctival, corneal or scleral injury. Superficial injury can be treated with local antiseptic or ATB ointment. In case of deep non-perforating wound, suture must be made under antiseptic conditions. Perforating injury can lead to endophthalmitis, which can result to visual loss and loss of the eye in unfavourable progress. First-aid requires covering the eye or both eyes if immobilization of eye movement is needed. Foreign bodies are either metallic or non-metallic. Metallic bodies can be removed by endomagnet. Final treatment requires suturing the ocular tissues in microsurgical station. The presence of foreign bodies can often be found on conjunctiva and cornea, which causes serious difficulties like epiphora, photosensitivity, pain and blepharospasm. Conjunctival injection and presence of foreign body on conjunctiva or cornea is present. Treatment requires removal of the foreign body, application of antiseptic or ATB ointment and covering of the eye. More serious ocular injury is perforating trauma of cornea or sclera with intraocular presence of foreign body. Diagnose is made upon anamnesis, opthalmoscopy, sonography and computer tomography or nMR. Treatment subsists in immediate suture of perforating wound. Foreign body can be removed during primary surgical treatment or during 2nd phase. In this case, PPV is done and the foreign body is removed by endoscopic forceps or magnet. If the foreign body contains iron or copper, all pieces must be removed; otherwise their presence will lead to toxic damage of retinal photoreceptors – metalosis. Non-metallic foreign bodies can be inert or organic. Glass and plexiglass are inert materials. Those materials, if not contaminated, do not cause inflammation and little parts can stay inside of the eye. By contrast, all organic foreign bodies’ must be removed as soon as possible. If a foreign body hits the eye at high speed, it can exit the globe on the posterior pole. This type of trauma is called double penetrating injury. A large non-perforation injury of the eye is called a contusion. Mechanical energy progresses from the front surface inside to posterior pole of the eye. Depending on the seriousness of the injury, damage to the eye can be reversible or irreversible. High impact to the eye can lead to eye rupture. Rupture of the sclera can be covered by conjunctiva and therefore realized with difficulty. Large ruptures of the eye often lead to atrophy of eye bulb. With a major ocular injury, there is always a risk of sympathetic ophthalmia. With such an injury, the affected eye activates an immune response, which leads to gronulomatous uveitis of the other sympathized eye. The consequences of such injuries illustrate just how important it is to examine both eyes after major injuries. It is fortunate that sympathetic ophthalmia usually responds well to steroids therapy. Damage to the eye can be caused by infrared, ultraviolet and ionizing radiation. Laser radiation and direct sun light can also be damaging. Infrared light – long exposure to heat radiation, for example during glass-blowing can cause glass-blower cataract. During trauma caused by high temperature, the following must be considered – temperature, duration of exposure and amount of harmful substance, the eye has been exposed to. Ultraviolet light is dangerous during welding (photoelectrical ophthalmia) and in high mountain areas, and has damaging effect of the corneal epithelium. Ionizing radiation causes similar symptoms like those caused by photoelectrical opthalmia. Electrical energy can be the cause of eye burn and cataract. Serious damage to the cornea and conjunctiva is caused by acid and alkali burn. Acid causes coagulative necrosis; alkali causes colliquative necrosis, which is worse because the burn penetrates faster and deeper. Timely and appropriate first aid is crucial for the future prognosis of the eye and sight. Immediate and thorough dilution of the harmful substance must follow (most often water rinse). Any large pieces of foreign bodies are necessary to remove mechanically. It is very important to remove any mortar or lime substance from upper lid conjunctiva till its eversion or double eversion. Insufficient removal of those foreign bodies causes prolonged exposure to the harmful substance, resulting in loss of transparency of the cornea, scarification of the conjunctiva and conglutination of tarsal and palpebral conjunctiva (symblepharon). Late consequences of burn can be solved in chirurgical manner. The ultimate success of corneal transplantation and chirurgical removal of symblepharon becomes problematic. Control questions: 1) Corneal erosion causes: a) foreign object in the other eye b) foreign object in the eye c) increase of intraocular pressure d) decrease of intraocular pressure 2) Contusion of the eye can harm: a) cornea b) iris c) ciliary body d) all structures of the eye 3) Which of the following materials of foreign origin is well tolerated by the eye and it not a cause of inflammation? a) wood b) glass c) copper d) iron 4) Which of the following is not appropriate treatment for lime burn of the eye? a) thorough water rinse b) rinse by acid c) mechanical removal of the lime d) immediate transport to an ophthalmologist 5) Which of the following statements about sympathetic ophthalmia is false? a) inflammation of the functional eye caused by blind eye after major injury b) granulomatous panuveitis c) treated by steroids d) caused by retinal detachment Neuroophthalmology The eye is a sensory organ, which transforms optical information to bioelectric potentials. These potentials are led through the visual pathway to the central nervous system, where they are further utilized. The light is transformed by retinal photoreceptors to bioelectric potentials. The photoreceptors are connected to the central nervous system by the visual pathway. The visual pathway consists of three neurons. Its long dendrites create the visual pathway up to the corpus geniculatum laterale. We can divide the retinal pathway clinically (retina, optic nerve…) or anatomically (first neuron, second neuron …). The part of visual pathway from retina to corpus geniculatum laterale is called primary visual pathway. A lesion of the peripheral neuron shows as an atrophy of the optic nerve. It is visible by an ophthalmoscope and followed by a defect in the photoreaction. Insult of the central neuron in visual pathway is shown neither by an optic disc atrophy nor defect in the photoreaction. Retinotopic lay-out of the visual pathway is described as if there was a lesion in any location, there is a specific defect in the visual field. Other way round, according to a specific defect in visual field we can assess a location in the visual pathway, which is used in diagnostics of visual pathway diseases. We picked out some optic disc pathologies: papilloedema, neuritis, neuropathy and optic disc atrophy. The optic disc is examined by direct or indirect ophthalmoscopy, event. digital imaging (HRT machine). In physiological case optic disc has distinct margins, physiological colour and no elevation. Papilloedema is not a disease of the optic nerve, but a sign of raised intracranial pressure (event. high pressure in the orbital apex). Papilloedema appears as a champagne cork. It is elevated above the retinal plane, into the eye bowl. The optic disc has indistinct margins and there may be seen parapapillary flame-shaped haemorrhages. There is no direct correlation between the appearance of the optic disc and visual functions. Optic nerve inflammation (optic neuritis) Based on the localization of the optic nerve inflammation we speak about intraocular neuritis, the inflammation is right in the optic disc and retrobulbar neuritis, the inflammation affects the part behind the optic disc. Due to the emergence we differentiate an acute neuritis, which develops in couple hours or days and chronic, with sneaking development in weeks or months. Clinical features of optic neuritis are dull pain behind the eye bowl, sudden and severe visual impairment because of a central scotoma, which may culminate to mostly temporary amaurosis. According to the localization of the pathologic focus regarding the optic disc, it clinically appears as an optic disc swelling in the case of intraocular neuritis. Normal disc is associated with retrobulbar neuritis. The finding is usually monocular, but it may be also bilateral with a time delay between appearances on both eyes. Optic neuritis develops usually in young adults. The most common etiology is sclerosis multiplex. Parainfectious or postinfectious neuritis may also occur basically after all infections, but it is very rare. The therapy depends on etiology and clinical features. In the case of sclerosis multiplex we cooperate with neurologists and mostly submit corticosteroids, initially in pulse intravenous application, later on per oral. Optic nerve neuropathy can be hereditary or acquired. Acquired neuropathy can be either exogenous or endogenous. The endogenous neuropathies are for example: alcohol, tobacco and drug-induced neuropathy. These neuropathies are rare in our country. Very unique is the methanol neuropathy with its acute development and vision or even life threat. In intoxication with smaller amount of methanol, which is fortunately more common, the visual impairment can occur with latency of 1 or 2 days. In this case, there is a risk of blindness without treatment. Optic disc atrophy is an end result of a disorder of visual pathway. Atrophy appears as a white or dirty grey disc, which is a clinical expression and is hard to define exactly. It occurs after destruction of a larger count of nervous fibres, compensative gliosis and reduction in number of small blood vessels on the disc surface. The most common is a simplex atrophy with sharp margins, white and flat disc or light excavation. In the case of bilateral simplex atrophy, we think about a lesion in chiasm or the visual tract. Glaucoma atrophy is typical with its disc excavation. This excavation may reach to the margins in late stages. Hereditary disc atrophy is very rare. Control questions: 1. The first neuron of the visual pathway is: a) rods b) cones c) bipolar retinal cells d) Ganlion retinal cells 2. Primary visual pathway is: a) visual pathway from the dominant eye b) visual pathway of the better seeing eye c) visual pathways of monkeys d) the part of visual pathway from retina to corpus geniculatum laterale 3. A sign of papilloedema is not: a) indistinct margins b) decrease of visual acuity c) parapapillar haemorrhages d) optic disc elevation 4. Clinical features of acute optic neuritis: a) forehead pain b) mostly bilateral c) reduction in visual field d) central scotoma 5. The optic nerve atrophy does not define: a) simplex atrophy, where a white disc occurs b) glaucoma atrophy, where the disc is excavated c) optic disc swelling d) atrophy flava in tapetoretinal degeneration Strabismus and amblyopia Strabismus or heterotrophy is signification for muscular and sensory defect of common eye cooperation. In normal way the globes are in balance standing and the Picture of watched subject impacts into the fovea in both eyes. If the globes are in incorrect balance standing the picture does not impact into the fovea in one eye. This eye is sheering of. The grade of divergence is measured by the angle which is contained by the axis of eye view both eyes. The balanced standing of the eyes, theirs motorical and sensorial coordination, are supposition for binocular vision. As a single binocular vision we denoted the ability to make one Picture of watched subject. As a current parallel vision we denote the ability to perceive the retinas of both eyes currently. The fusion is the ability to impact the pictures from both eyes to single view. The stereopsis is the ability of the three-dimensional vision. The progression of the vision function takes several years. The binocular vision is fixed about 5 years of life. The strabismus is divided to concomitant and incomitant. The concomitant strabismus - we differentiate this type on line of deviation to convergence strabismus /ezotropia/ and divergence strabismus /exotropia/. We difference sursumvergent strabismus and deorsumvergent strabismus in combinated form of strabismus. The tendency of the treatment is reaching of the parallel eyes standing and to make binocular functions. The treatment includes the correction of the refractive defect, the training amblyopia / pleoptics/, training binocular functions /or optics/, surgical correction of the strabismus The incomitant /paralytic/ strabismus-is characterized by limited mobility of the globe /e.g. myasthenia, myogenic and neurogenic paralysis/, diplopia, variable deviation of the squint in the various vision directions and forced compensational carriage of the head to stopped diplopia. Amblyopia - lazy-eye blindness. It means abnormal progress of the vision which is clinical definite as a decrease of the eyes visual resolution at optimal correction without symptoms of the eyes diseases. We differentiate amblyopia to congenital amblyopia, amblyopia from the cessation of the progression, /it occurs the first 4 years/ and amblyopia of the deletion the functions /it occurs after the finishing of the functional progression/ Error of Refraction and their Correction The eye refraction expresses the ratio between the length of the globe in the optical axis and optical power of refraction settings. The refraction settings include the cornea, the anterior chamber, the lens and the vitreous humour. The latter make up an optical eye system. The largest refraction value is provided by the cornea /about 43 dioptres/. The lens only provides about a half optical power. As emmetropia we denote a stage which the focus, into which the parallel incoming rays are refracting, is situated on the retina. In emmetropia the length of eye is in correct ratio with the optical power of its refraction settings. If the ratio is disturbed and the focus is not situated on retina anymore, we speak about refraction defect or ametropia. In ametropia, the rays converge outside of retina, which results in forming an unfocused Picture. We differentiate between a refraction ametropia /the optical system is to intense or to weak at o normal globe length/ and an axial ametropia /the globe length in an optical axis to long or to short at a normal optical power A vast majority of ametropia is axial. There are basically 3 errors of refraction: 1, Farsightedness /hypermetropia/: rays meet as far as behind the retina. 2, Short-sightedness /myopia/: rays meet in front of the retina. 3, Astigmatism: optical eye system does not avail of the same optical power in all meridians. We correct hypermetropia with connecting /convex/ lenses of a plus value, myopia with diffuse /concave/ lenses of a minus value, astigmatism with cylindrical glasses which avail of a variable optical power in various axes. Presbyopia is a state, in which aging physiological decrease the amplitude of accommodation, which manifests gradually with increasing problems while looking at o short distance e.g. reading. The first disorders are developing around the 40th year of again people who had not wearing glasses yet. Subjective disorders recede on prescribing a correction for looking at a short distance. To establish refraction we use both objective and subjective methods. Among objective methods mainly ranks a direct skiascopy. To establish total eye refraction we use a refractometer and to establish a corneal astigmatism we use a keratometer. The current modern devices allow for measuring of refraction as well as corneal curvature automatically an autorefraktometer. The letter examination is quite fast and accurate. Uncorrected eye defects reduce the quality of vision and inflict numerous subjective disorders/ pain in the eyes, a headache, and tiredness. To correct refraction defects, glasses and contact lenses are most frequently applied. A refraction defect, however, can be removed surgically, too. Surgical refraction jobs can be divided into those on the cornea and intraocular operation. Among the surgical jobson the cornea, there belongs a change to the corneal refraction with an excimer laser, by term coagulation, performing of refraction slits. Among intraocular operations, there rank, e.g. removing of a patients clear lens /refraction lensectomy/ and implantation an artificial intraocular lens inside the eye. The lens consequently corrects a refraction defect. From all mentioned methods, the most used one is the laser refractive surgery. Corneal curvature is changed by an “excimer” laser during this procedure. Excimer laser is an ultraviolet-based laser in the wavelength of 193nm. The laser ray removes a thin layer of corneal tissue and changes the corneal curvature and herewith the optical power of the cornea. In present time there are two techniques used: undersurface and surface ablation. The undersurface technique – LASIK (laser in situ keratomileusis) has its most advantages like no pain after treatment, fast visual recovery, and long stabile visual outcome even in correction of high refractive errors. It is the most used technique in present time. A surface layer of corneal tissue (flap) is during this method created and under this flap acts the laser a change of corneal curvature. At the end of the surgery the flap is set back, which highly reduces postoperative pain. Among the surface ablation techniques belong PRK (photorefractive keratectomy), LASEK and epi-LASIK. Surface ablation techniques are used in refractive errors up to 5 dioptres. These techniques are based on a surface treatment of corneal curvature by a laser beam after previous removal of the epithelium. Control questions: 1. In myopia is not true: a) the eye bowl is usually short b) the patient has decreased distance visual acuity c) correction is provided by concave lenses d) the eye sees well without correction to the short distance 2. Presbyopia is: a) drawing off the pathological tissue of the eye under pressure b) diplopia caused by a pressure on the eye bowl c) lazy-eye acquired in the childhood d) age related decreased ability of focusing to the near distance 3. The most common surgical technique in correction of refractive errors is: a) LASIK – undersurface laser ablation technique b) PRK – surface laser ablation technique c) exchange of crystalline lens for artificial intraocular lens d) conductive keratoplasty 4. Laser correction - LASIK for refractive errors is: a) change in the curvature of crystalline lens by laser b) change in the depth of anterior chamber by laser c) change in the curvature of cornea by laser acting on the epithelium d) change in the curvature of cornea by laser acting on the stroma 5. Emmetropia is: a) stage, when the refractive error is 0 dioptres b) stage, when the dioptres differ in both eyes c) stage, when the refractive error is different then 0 dioptres d) stage, when there is a refractive error Social ophthalmology. Severe Sight Impairment and Blindness. Severe Sight Impairment and Blindness present one of the most significant worldwide problems at presents. According to figures the WHO the number of the blind in the world is about 40 million. The prevalence of the sight impairment and blind people is 10-40 timers higher in the developing countries than the technically advanced once. In the developing countries the prevalence of the blinds estimated at 0.4 to 8.8 %. The main causes are cataracts, infection diseases and malnutrition deficit. The prevalence of the blindness in the technically advanced countries is about 0.2%.The cause of blindness, in most part, consists in macular degeneration, diabetic retinopathy, glaucoma. A unified and exact delimitation of the notion of blindness is not easy because there are considerably criteria determining the extent of vision impairment. Complete absolute blindness is only one to be delimited exactly. However not only persons with absolute blindness, but a number of persons with a decreased vision resolution live in decreased existential conditions, so that they can be considered to be blind, especially from the social or legal point of view. The classification is also influenced by the capacity of the handicapped to adapt to the newly originating life situation, while an important role is played by the age, the time of losing sight, intelligence, psychological and general health condition of the patient, and ability of orientation in unfamiliar setting, environmental influence, family, etc. From this point of view, there follow 2 grades of sight impairment- absolute and practical blindness. Absolute blindness- is a loss of vision including the status from a total loss of the feeling of light/ amaurosis/ up to retaining the feeling of light with a defect light projections, i.e. the loss of an ability to determine the direction from which the light is coming. Practical blindness-is defined as a sight disorder barring orientation in an unfamiliar setting. It corresponds to a decrease in central visual resolution below 3/60 and a binocular narrowing of the vision field below 10 degrees around central fixation. Rehabilitation of vision-impaired and blind people depends on age at which the vision impairment occurred. The aim of rehabilitation consists in maintaining and/or developing the remnants of vision and utilizing touch and hearing to perceive sensations of the surrounding world. There is a necessity of a close cooperation of the eye doctor with the professionals in specialized facilities/ kindergartens for the vision –impaired, the blind/, basic school/ the weak-vision, with remnants of vision and the blind/, special schools / weak-vision, the blind/ secondary school for vision-impaired youth, apprentice centres for the vision-impaired youth/ specialization in upholstering, book-binding, engineering mechanic/, centres for prequalification and rehabilitation of vision-impaired and blind people who acquired impairment at later age. Part of correct and complete rehabilitation is also a suitable use of rehabilitation/ improving/ and compensation/substituting/aids. The improving aids are determined for the visualimpaired people, whose vision has been partly retained and used. They include, in the firs place, glasses, binocular glasses, tarpon, magnifying glasses and electronic devices of a TV character. The substituting aids are determined for the blind. In this group fall, e.g., a while stick, the blindness clock, tape recorders, sound books, and books in the Braille script. Rehabilitation of the vision-impaired is either specific, or further life of the handicapped often depends on it. It is important to erasure a corresponding pre-school and school education and tuition, include the handicapped in employment and secure the social guarantee in disease and the old age. This Syllabus was prepared by: MUDr. Renáta Brunnerová, MUDr. Jara Hornová, CSc, Prof.MUDr. Pavel Kuchynka,CSc, MUDr. Magda Netuková,PhD, Doc. MUDr. Petr Souček, PhD, MUDr. Pavel Stodůlka, PhD, MUDr. Magda Vokrojová, PhD.