HISTOLOGY COURSE 9TH SEMESTER OSLO 96
advertisement

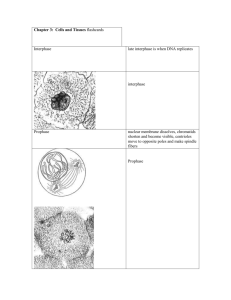
HISTOLOGY COURSE 9TH SEMESTER OSLO 96 Microscopic slides, electron micrographs, tasks for independent study Jon Storm-Mathisen Translated by Megan Eileen Wittmann Anatomical Institute University of Oslo 2002 Storm-Mathisen, Jon “Histology Course. Microscopic slides, electron micrographs, tasks for independent study” Translated by Megan Eileen Wittmann Histology Course 9th Semester Oslo 96 Anatomical Institute, University of Oslo Copyright © 2002 Anatomical Institute, UiO Copied with the permission of the author 1 Contents General information..………………………………………………….……………………… 2 Histology course 1 (Week 1): Male genitalia.….…………………………………………….. 3 Histology course 2 (Week 2): Female genitalia I…………………………………………….. 6 Histology course 3 (Week 3): Female genitalia II……………………………………………. 8 Histology course 4 (Week 11): Placenta……………………………………………………. 10 General information The slide cases and electron micrographs are located in the histology course rooms at Domus Medica. One of the rooms is usually vacant and can be used for independent study. In addition, slide cases and EM pictures are available for loan from the Biomedical Library. Slide cases and electron micrographs are NOT to be removed from the course room. Be responsible: Make sure that the slide preparations are put back undamaged. The principal aim of the course is to provide concrete knowledge of various structures of functional and clinical importance. Following each introductory lecture in a course area, study the relevant slides using a histology textbook. It is important to prepare for the course, noting any problems/questions that should be discussed during the summary course with an instructor. The slides include many structures that are not necessary to identify by name. We have therefore selected the central structures to be identified and investigated. Slides of the same type and number from the different slide cases are not always identical in appearance. It is therefore recommended to examine more than one slide case. The slides are from human tissue if not otherwise specified. Review the guidelines for the investigation of slides under the microscope (Veiledning i undersøkelse av mikroskopiske preparater) from 1st semester for a general review of microscopy techniques etc. Important points, often forgotten: - Condenser always at maximum elevation. - Top lens always in the light path when using objectives x10 and x40. - Aperture diaphragm open, lessen the opening to obtain the desired contrast (high contrast is only advantageous in viewing special details such as cilia, brush border, striation in muscle tissue); this technique reduces visible contrast attained by staining the preparation. - Continuously focus up and down while using x40 (because the “optical section” is thinner than the microtome section). - Always start by examining the slide preparation macroscopically, continuing in succession with x4, x10, x40. Examine all tissue areas. 2 Histology course 1 (Week 1): Male genitalia Slide 1: Testicle H+E In addition to the testicle (testis), the slide preparation also includes the epididymis and mesotestis with connective tissue, nerves and blood vessels. (Take the opportunity to identify arteries, veins and nerves contained in the connective tissue.) Identify: Tunica albuginea Tunica vaginalis (the mesothelium is partially torn and discoloured at the edge of the section, therefore, look also in the fold between the testis and the epididymis. Septula testis (singular: septulum testis) Mediastinum testis, including rete testis Tubuli seminiferi contorti (singular: tubulus seminiferus contortus) - Sertoli cells1 (characteristic appearance; What do these cells do?) - Spermatogonia (closest to the basal lamina) - Spermatocytes (the majority of which are primary spermatocytes, as secondary spermatocytes quickly enter the secondary meiotic division) - Spermatids - Sperm Interstices - Myoid cells (along the outer border of the tubules) - Interstitial cells (Leydig cells2) What is their function? Do they resemble other cells you have seen with a similar function? Are there differences in the germinal epithelium in the different parts of the seminiferous tubules? What is the significance of this? Slide 2: Testicle Cat PFD + toluidine blue The slide includes the same structures as in slide 1, but a few points are better demonstrated. The slide preparation is from a cat, killed under general anaesthesia by perfusion of the vascular system (note the empty and slightly dilated vessels) with an aldehyde solution (cross links proteins so that the tissue is preserved). The tissue sample is thereafter treated with OsO4 and embedded in epoxy plastic (hard enough to cut thin sections). This section is approximately 1μm thick and stained with PFD (para-fenylenediamine, which results in a brown colour in areas where the fat has been fixed with OsO4) + toluidine blue (stains, like haematoxylin, nucleic acids and other acidic substances). PFD-staining is absent in the central portion of the preparation where OsO4 did not reach. Thin plastic sections used in light microscopy are often referred to as “semi-thin sections” (i.e. not as thin as “ultra-thin sections” used in electron microscopy. Thin sections provide high resolution (small structures can be seen more easily than in thicker sections). Identify the same cell types as in slide 1. Note spermatids in various developmental stages (spermatogenesis and spermiogenesis is perhaps best be studied in the central portions of the preparations where the PFD staining is lacking). Attempt to recognize cell nuclei that are dividing (visible chromosomes, nucleus membrane is absent). (Look for the dividing nuclei near the basal lamina. View the entire section. Why?) What are the brown stained (i.e. lipid containing) structures in the Leydig cells? 1 2 Enrico Sertoli (1842-1910). Italian physiologist. Franz von Leydig (1821-1908). German histologist. 3 What is their function? (They are absent from the central portion of the slide preparation. What can be the reason for this?) EM-pictures from the same tissue specimen as slide 2 The electron micrographs are located next to the slide cases. (They are not to be removed from the course room! They can be loaned from the Biomedical Libary, folder marked “GI-traktus, nyre, testis”) H239 Overview of the seminiferous tubule wall H242 Higher magnification of a part of H239 H237 Interstices Compare with slide 2 and identify the following: Sertoli cell (processes emanated by the cell pervade the thickness of the tubule wall) Sperm head Spermatids (various stages) Spermatogonia Primary spermacyte Myoid cells and a portion of a capillary seen in cross section Spermatids containing developing acrosomes. Note its proximity to the Golgi 3 complex in H242 (Can you distinguish signs that spermatids stemming from the same spermatogonium form a syncytium?) Leydig cell (a part of one) with smooth ER, lipid droplets and mitochondra with tubular cristae in H237. (What are the small black particles?) H233-H236 Spermiogenesis Discuss these electron micrographs based on what you know about the sperm structure and genesis. Slide 3: Testicle, Child H+E Compare to slide 1 and try to identify the same structures. How would you characterize the seminiferous tubules? Can you see Leydig cells? Can you identify anything that could possibly be the epididymis? Compare to slide 4. Appendix testis? Slide 4: Epididymis H+E Compare to slide 1. Epididymis (stemming from the Greek “on top of the twin”, the testicles were in old times euphemistically referred to as “the twins”; it is pronounced with the stress on “di” and has the plural form, epididymides, and the genitive case, epididymidis, with the emphasis on “dy”). Identify: 3 Camillo Golgi (1844-1926). Italian anatomist and histologist, received the Nobel-prize in medicine and physiology in 1906 (together with Santiago Ramón y Cajal). (Note: The name is pronounced with “gi” as in the English pronunciation for gin.) 4 Tunica vaginalis Ductuli efferentes Ductus epididymidis Stereocilia (What are they? What is their function?) Smooth muscle cells surrounding the ductus and ductuli Is it possible to identify sperm in the lumen? Note the junctional complex (“terminal bar”) towards the duct lumen. (What does it consist of, at the EM level? What is its function? Where have you seen a similar structure?) Slide 5: Ductus deferens H+E Identify: The pseudostratified epithelium overlying the lamina propria. (Note the longitudinal folds that give the lumen an irregular cross-sectional outline. What does this indicate about its function?) Three layers of smooth muscle. (How are they organized?) Compare the epithelium to that of the ductus epididymidis. Is it possible to state anything about the nerve supply to this tissue? Slide 6: Prostata H+E Identify: Glands: - Characterize the epithelium (there is autolysis, the epithelium is partly torn) - Corpora amylacea (What are they?) Stroma - Smooth-muscle cells (compare to the smooth-muscle cells of the artery vessel walls) - Connective tissue (note the difference from the smooth-muscle regarding colour and structure) Fibrous capsule and surrounding connective tissue - Can you identify parts of the venous and nervous plexuses that pass by the prostate? Slide 7: Prostate, Child H+E The stroma and glands contain the same elements as in slide 6, but are not fully developed. (Try to explain what the differences are.) In the fully developed prostate it is possible to distinguish between the main glands, the submucosal glands and the glands of the urethral mucosa. Which glands become enlarged in prostatic hyperplasia? What is the significance of their localization in terms of the functional consequencs of the enlargement? Identify: Urethra, look for the openings of secretory ducts Colliculus seminalis, look for the rudiment of the utriculus prostaticus. (What is it?) Ductus ejaculatorius (plural: ductūs ejaculatorii) This slide preparation provides a good overview of the structure and the immidiate surroundings of the prostate gland. Review the last question under slide 6. Can you see ganglion cells in the nerve plexus, what kind of ganglion cells? Which organ do these nerves innervate and what clinical 5 significance does the proximity to the prostate have? Is there any striated musculature in the section, and to which structure does this belong? (Which organ do you see in addition to the prostate and urethra? Review the structures of the mucous membrane and wall structures?) Slide 8: Penis “HAS” Haematoxylin, azafloxine (eosin can be substituted for azafloxine), saffron corresponds to H+E. Saffron is added in order to stain connective tissue fibres yellow (some pathology laboratories use this as routine staining of histology slides). Identify: Corpora cavernosa penis (the septum dividing them is incomplete) (singular: corpus cavernosum penis) - tunica albuginea and the trabeculae that extend inwards in the corpus (connective tissue or smooth-muscle?) - cavernous spaces (vascular spaces separated by walls containing smooth-muscle cells and connective tissue). Note the size difference between central and peripheral caverns of each corpus, and the thin-walled peripheral veins (explain in terms of the mechanisms for erection) - arteriae helicinae (spiral arteries), characterized by a thick wall, branches of a. profunda penis. (What happens to them during erection?) Corpus spongiosum penis - caverns, compare to the caverns of the corpus cavernosum - urethra, with intraepithelial and paraurethral mucous glands of Littré4. (What type of epithelium lines the urethra?) Surrounding stroma - smooth-muscle (contracts in the cold) - nerves (abundance?), try to locate Vater5-Pacinian6 sensory organ (properties/function?) - nervus and arteria dorsalis penis (Which nerve/artery do these stem from?) Skin (What type of epithelium? Which types of glands can you find?) Histology course 2 (Week 2): Female genitalia I Slide 9: Ovary, Cat H+E Peritoneal epithelium (still called “germinal epithelium” despite not giving rise to germ cells) From where do the primordial germ cells originate? Cortex containing follicles and stroma - primordial follicles: primary oocytes surrounded by a layer of follicle cells - primary follicles: primary oocytes with a zona pellucida and multiple layers of follicle cells - secondary follicles: these have in addition an antrum folliculi and a theca layer (Look for cells in mitosis!) - Graafian7 follicle: secondary oocyte (the 1st meiotic division has taken place), zona pellucida, a large antrum folliculi (containing the liquor folliculi), cumulus oophorus, zona granulosa (granulosa cells resting on the basal membrane), theca (interna and externa) 4 Alexis Littré (1658-1726). French anatomist and surgeon. Abraham Vater (1684-1751). German pathologist (pronunc.: “F....”). Additionally: papilla Vateri (papilla duodeni major). 6 Filippo Pacini (1812-1883). Italian anatomist. 7 Reijnier de Graaf (1641-1673). Dutch anatomist and physician. 5 6 - atretic follicles (What is atresia of follicles?) - stroma (“fibroblasts”) - interstitial cells (collections of cells similar to the interstitial cells of the testis; in the human, they are primarily located in the hilus and mesovarium) Medulla with blood vessels Hilus (hilum) and mesovarium Slide 10: Ovary, Cat PFD + toluidineblue (cf. slide 2 concerning the method of preparation) Identify the same structures as in slide 9. Pay specific attention to the lipid droplets (stained brown) in the interstitial cells and in theca cells. (In the human, steroid hormones are primarily produced by the theca interna.) Compare to the interstitial cells of the testicles in slide 2, which produce the same class of hormones! Lipid droplets (“yolk platelets”) are also present in the oocytes. Note that the theca is vascularized, but not the granulosa. Slide 11: Corpus luteum H+E Most of the slides show a corpus luteum with remains of an ovary. How is a corpus luteum formed, and how do you explain the resulting structure? Which hormones are predominantly produced by each of the two types of endocrine cells? How is hormone production regulated? Identify: Granulosa lutein cells Theca lutein cells (compare to the appearance of the interstitial cells in slide 9 and slide 1) Ovarian stroma (the theca externa is not distinguishable) Loose connective tissue and/or blood-clot in the previous antrum Slide 12: Ovary, 6 year-old H+E Compare to slide 9. Which structures do you see in both slides, and which are absent from this slide? (Ignore the cystic structure located centrally in the preparation. There are some autolytic changes in the tissue.) Which other organ is found on the slide, besides the ovary? Slide 24: Mesonephros and the primitive gonad, Chicken embryo H+E Identify: The primitive, indifferent gonad forming the gonadal ridge, at the posterior wall of the coelom, between the mesonephros and the mesentery (look at slide preparations from different slide cases, as the gonad may be better viewed in some preparations than in others). Primordial germ cells (large, globular nuclei), surrounded by supporting cells to form the primitive sex cords (From where do the primordial germ cells migrate to this area? What originates from the sex cords in the two sexes? Review the descent of the testis and ovary.) Wolffian8 duct (mesonephric duct) What originates from it? What is formed from the Müllerian9 duct (paramesonephric duct, not identifiable in the sections)? 8 9 Kaspar Friedrich Wolff (1733-1794). German anatomist, embryologist and physiologist, worked in St. Petersburg. Johannes Peter Müller (1801-1858). German anatomist, physiologist and pathologist. 7 Slide 13: Tuba uterina, 11 year-old H+E Synnonyms: uterine tube, salpinx, Falloppian10 tube Identify: Mucosa - epithelium (Can you identify different types of cells? Can you infer something about their functions, based on their appearances?) - lamina propria (richly vascular) Muscularis (circular and longitudinal layers) Serosa (peritoneum) (the peritoneal mesothelium is, for the most part, ruined in this preparation) From which tube segment does the preparation most likely stem? Histology course 3 (Week 3): Female genitalia II Slide 14: Uterus, early proliferative phase H+E Identify: Endometrium - characteristics of the surface epithelium (in many areas the epithelium is torn) - characteristics of the glands - stroma (identify the different types of cells) Is it cell rich? - spiral arteries (What happens to them during menstruation?) - stratum basale (lamina basalis) - stratum functionale (lamina functionalis) Myometrium Slide 15: Uterus, late proliferative phase H+E Identify the same points as in slide 14. Compare the breadth of the cell layers and the tissue structure in the two slides. Slide 16: Uterus, early secretory phase H+E Identify the same items as in slides 14 and 15. Compare the breadth of the cell layers and the tissue structure in the three slides. 10 Gabriele Falloppio (Falloppius) (1523-1563?). Italian anatomist, student of Andreas Vesalius. 8 Slide 17: Uterus, curettage, secretory phase H+E Uterine scraping with a curette (curettement, abrasio) is used in diagnostic investigation and treatment. Identify the same structures as in slides 14-16. Based on the appearance of the endometrium, is slide 16 most likely from an earlier or a later stage of the menstrual cycle than slide 17? Note the characteristic form of the glands (“saw-toothed”). Can you see gland epithelial cells that show sign of containing aggregates of glycogen particles (washed out in the preparation of the tissue)? Can you from what you see, realize that the spiral arteries are in fact coiled? Review the hormonal regulation of the menstrual cycle. Slide 18: Cervix uteri H+E Identify: The wall of the cervical canal (canalis cervicis uteri) - surface epithelium (low cuboidal in many areas, in other areas the epithelium is missing due to preparation artifact) (Can the height of the epithelium give an indication of which phase in the menstrual cycle this slide represents?) - plicae palmatae (surface epithelial folds with a gland-like structure), secretion-filled cavities (What is the function of the cervical secretions and how does the consistency change throughout the menstrual cycle?) - myometrium Portio vaginalis cervicis uteri (“portio”) - epithelium of a type similar to that of the vagina (How would you classify this epithelium?) Locate the transition between cervical and vaginal epithelium (the location where malignancy often arises); this transitional zone is often outside the opening of the cervical canal, a phenomenon mistakenly called “erosion” due to the fact that the columnar epithelium of the cervix has a red colour. (What is the actual explanation for this colour?) - loose connective tissue, rich in plasma cells (What is their significance at this site?) Slide 19: Vaginal smear Papanicolaou11 The smear is stained with a mixture of haematoxylin and various other dies (“Pap-smears” are used throughout the world in exfoliation cytology for the early diagnosis of cancer, particularly of the cervix utreri). Identify areas of squamous epithelial cells sloughed (shed, exfoliated) from the vaginal wall, granulocytes, and bacteria. (Note: the bacteria are in a lower focal plane. Why?) Slide 19: Cervical smear Papanicolaou11 Identify groups of columnar epithelial cells shed from the cervical canal, and mucous strands from the cervical secretions. (Squamous epithelial cells, etc. from the vagina are also seen.) 11 George Nicholas Papanicolaou (1883-1962). Greek-American physician and cytolgist, introduced in 1928 the method of exfoliative cytology for the detection of atypic cells in smears as a sign of cancer in situ. 9 Histology course 4 (Week 11): Placenta, umbilical cord, mammary gland Slide 21: Endometrium with egg H+E Identify: Endometrium. Compare to slide 17: Gland shape, appearance of the gland epithelium, relative amounts of gland/stroma, appearance of the stroma cells, presence and appearance of spiral arteries. (What is meant by saying that the stroma cells have undergone decidual reaction? Find such areas.) Notice the variation between different parts of the section. Egg (conceptus) - decidua (part of the endometrium that is shed once pregnancy has ended) - cells from the trophoblast that have invaded the endometrium (notice areas of “atypia”, the trophoblast shares certain qualities with malignant cells (which ones?) and can give rise to malignant tumours (chorion-carcinoma, hydatide mole)) - syncytiotrophoblast - intervillous spaces (What occupies these spaces?) - cytotrophoblast - extraembryonic mesoderm - chorionic villi (Which layers constitute the chorion?) - chorionic cavity (extraembryonic coelom) This pregnancy is reported to be of about the 3rd weeks duration. If this has been calculated from the first day of the last menstrual bleeding, how long has gone by since the time of fertilization? Which structures would you expect to see at this stage? Recapitulate the terms zygote, morula, blastocyst (blastula), embryoblast. Slide 22: Placenta, 3 months H+E Identify: Chorionic cavity Chorionic plate Chorion villi - extraembryonal mesoderm with blood vessels (the foetus has erythrocytes containing a nucleus). Notice the immature nature of the loose connective tissue (mesenchyme). - Hofbauer12-cells (“immature macrophages”, possibly protect against an immune reaction between the fetus and the mother; do you know other mechanisms that add to this?). - cytotrophoblast (this later becomes discontinuous and the fetal blood vessels come in direct contact with the syncytiotrophoblast, recapitulate the placenta barrier) - syncytiotrophoblast (How is the surface facing the intervillous spaces?) Maternal (intervillous) spaces (note areas with erythrocytes and leukocytes) (Can you detect parts of the decidua, i.e. the uterine mucosa?) Review the terms chorion leave, chorion frondosum, decidua basalis, decidua capsularis, decidua parietalis, primary/secondary/tertiary chorionic villi, cotyledons. 12 J. Isfred Isidore Hofbauer (1878-1961). American gynecologist. 10 Slide 23: Umbilical cord H+E Identify: Arteriae umbilicales Vena umbilicalis Mucoid connective tissue (“Wharton’s13 jelly”) (extraembryonic mesoderm, compare the appearance to that of the extraembryonic mesoderm of slide 22) Surface epithelium (amnion epithelium, extraembryonic ectoderm) Which other structures can one find in the umbilical cord at earlier stages of development? What happens to the blood vessels of the umbilical cord at birth? (Function of this? Mechanism by which it takes place?) Slide 24: Mesonephros and the gonadal ridge, Chicken embryo H+E Suggest approximately how old in human development this specimen corresponds to. (This slide is more thoroughly examined under Female genitalia I.) Slide 25: Lactating mammary gland (mamma lactans) H+E Identify: lobules (lobuli) interstitial connective tissue (connective tissue network separates the lobules and, intralobularly, the secretory acini) acini (Are you able to identify both proteinaceous and fatty secretions within the acinar lumina? What is their relevance in breast-feeding? Many acini are distended by milk that has been lost during the tissue preparation. Notice the variation in secretory state among the acini.) epithelial cells and myoepithelial cells (the latter are located between the basal lamina and the epithelial cells, but this cannot be distinguished in the preparation) plasma cells (Abundant within and between the lobuli. What is their clinical importance in this location? Review the mechanism of transfer of immunoglobulins through secretory epithelia.) ducts What is the histological appearance of the quiescent mammary gland? What changes do the mammary glands undergo during pregnancy? Review the hormonal mechanisms that instigate these changes. 13 Thomas Wharton (1610-1673). English anatomist and physician. 11