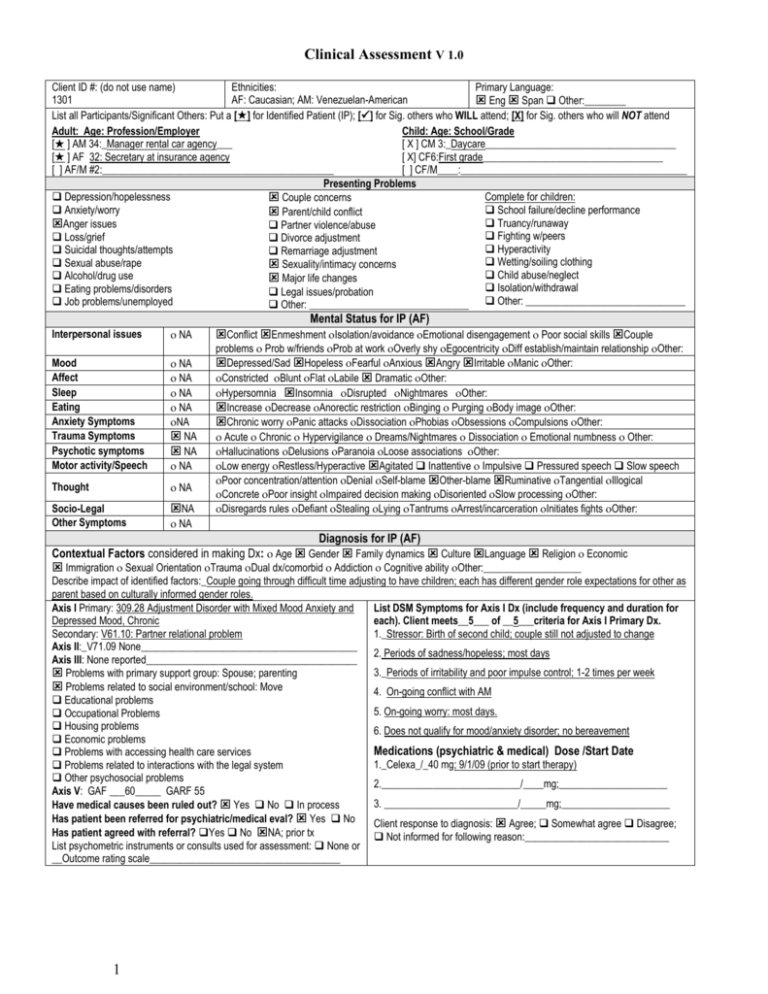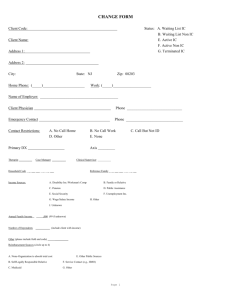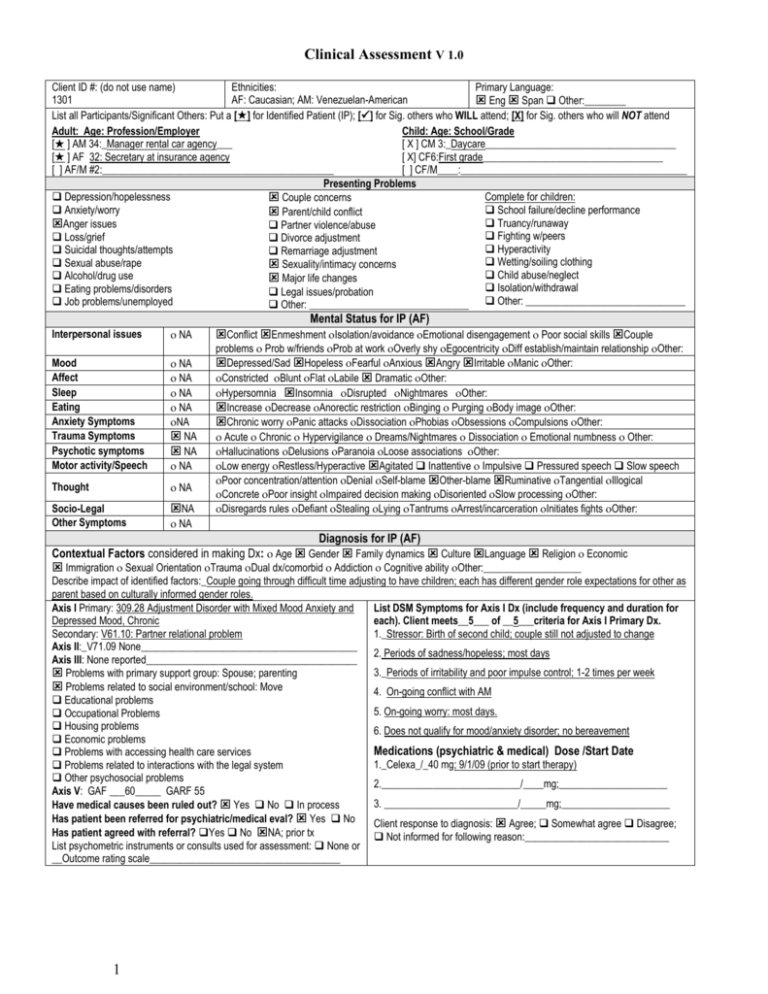
Clinical Assessment V 1.0
Client ID #: (do not use name)
Ethnicities:
Primary Language:
1301
AF: Caucasian; AM: Venezuelan-American
Eng Span Other:________
List all Participants/Significant Others: Put a [] for Identified Patient (IP); [] for Sig. others who WILL attend; [X] for Sig. others who will NOT attend
Adult: Age: Profession/Employer
Child: Age: School/Grade
[ ] AM 34:_Manager rental car agency___
[ X ] CM 3:_Daycare_____________________________________
[ ] AF 32: Secretary at insurance agency
[ X] CF6:First grade___________________________________
[ ] AF/M #2:_____________________________________________
[ ] CF/M____:____________________________________________
Presenting Problems
Depression/hopelessness
Complete for children:
Couple concerns
Anxiety/worry
School failure/decline performance
Parent/child conflict
Truancy/runaway
Anger issues
Partner violence/abuse
Fighting w/peers
Loss/grief
Divorce adjustment
Hyperactivity
Suicidal thoughts/attempts
Remarriage adjustment
Wetting/soiling clothing
Sexual abuse/rape
Sexuality/intimacy concerns
Child abuse/neglect
Alcohol/drug use
Major life changes
Isolation/withdrawal
Eating problems/disorders
Legal issues/probation
Job problems/unemployed
Other: _______________________________ Other: _______________________________
Interpersonal issues
NA
Mood
Affect
Sleep
Eating
Anxiety Symptoms
Trauma Symptoms
Psychotic symptoms
Motor activity/Speech
NA
NA
NA
NA
NA
NA
NA
NA
Thought
NA
Socio-Legal
Other Symptoms
NA
Mental Status for IP (AF)
Conflict Enmeshment Isolation/avoidance Emotional disengagement Poor social skills Couple
problems Prob w/friends Prob at work Overly shy Egocentricity Diff establish/maintain relationship Other:
Depressed/Sad Hopeless Fearful Anxious Angry Irritable Manic Other:
Constricted Blunt Flat Labile Dramatic Other:
Hypersomnia Insomnia Disrupted Nightmares Other:
Increase Decrease Anorectic restriction Binging Purging Body image Other:
Chronic worry Panic attacks Dissociation Phobias Obsessions Compulsions Other:
Acute Chronic Hypervigilance Dreams/Nightmares Dissociation Emotional numbness Other:
Hallucinations Delusions Paranoia Loose associations Other:
Low energy Restless/Hyperactive Agitated Inattentive Impulsive Pressured speech Slow speech
Poor concentration/attention Denial Self-blame Other-blame Ruminative Tangential Illogical
Concrete Poor insight Impaired decision making Disoriented Slow processing Other:
Disregards rules Defiant Stealing Lying Tantrums Arrest/incarceration Initiates fights Other:
NA
Diagnosis for IP (AF)
Contextual Factors considered in making Dx: Age Gender Family dynamics Culture Language Religion Economic
Immigration Sexual Orientation Trauma Dual dx/comorbid Addiction Cognitive ability Other:___________________
Describe impact of identified factors:_Couple going through difficult time adjusting to have children; each has different gender role expectations for other as
parent based on culturally informed gender roles.
Axis I Primary: 309.28 Adjustment Disorder with Mixed Mood Anxiety and
List DSM Symptoms for Axis I Dx (include frequency and duration for
Depressed Mood, Chronic
each). Client meets__5___ of __5___criteria for Axis I Primary Dx.
Secondary: V61.10: Partner relational problem
1._Stressor: Birth of second child; couple still not adjusted to change
Axis II:_V71.09 None__________________________________________
2. Periods of sadness/hopeless; most days
Axis III: None reported_________________________________________
3._Periods of irritability and poor impulse control; 1-2 times per week
Problems with primary support group: Spouse; parenting
Problems related to social environment/school: Move
4. On-going conflict with AM
Educational problems
5. On-going worry: most days.
Occupational Problems
Housing problems
6. Does not qualify for mood/anxiety disorder; no bereavement
Economic problems
Medications (psychiatric & medical) Dose /Start Date
Problems with accessing health care services
1._Celexa_/_40 mg; 9/1/09 (prior to start therapy)
Problems related to interactions with the legal system
Other psychosocial problems
2.___________________________/____mg;_____________________
Axis V: GAF ___60_____ GARF 55
3. __________________________/_____mg;_____________________
Have medical causes been ruled out? Yes No In process
Has patient been referred for psychiatric/medical eval? Yes No
Client response to diagnosis: Agree; Somewhat agree Disagree;
Has patient agreed with referral? Yes No NA; prior tx
Not informed for following reason:____________________________
List psychometric instruments or consults used for assessment: None or
__Outcome rating scale_____________________________________
1
Interpersonal issues
NA
Mood
Affect
Sleep
Eating
Anxiety Symptoms
Trauma Symptoms
Psychotic symptoms
Motor activity/Speech
NA
NA
NA
NA
NA
NA
NA
NA
Thought
NA
Socio-Legal
Other Symptoms
NA
Mental Status for IP (AM)
Conflict Enmeshment Isolation/avoidance Emotional disengagement Poor social skills Couple
problems Prob w/friends Prob at work Overly shy Egocentricity Diff establish/maintain relationship Other:
Depressed/Sad Hopeless Fearful Anxious Angry Irritable Manic Other:
Constricted Blunt Flat Labile Dramatic Other:
Hypersomnia Insomnia Disrupted Nightmares Other:
Increase Decrease Anorectic restriction Binging Purging Body image Other:
Chronic worry Panic attacks Dissociation Phobias Obsessions Compulsions Other:
Acute Chronic Hypervigilance Dreams/Nightmares Dissociation Emotional numbness Other:
Hallucinations Delusions Paranoia Loose associations Other:
Low energy Restless/Hyperactive Agitated Inattentive Impulsive Pressured speech Slow speech
Poor concentration/attention Denial Self-blame Other-blame Ruminative Tangential Illogical
Concrete Poor insight Impaired decision making Disoriented Slow processing Other:
Disregards rules Defiant Stealing Lying Tantrums Arrest/incarceration Initiates fights Other:
NA
Diagnosis for IP (AM)
Contextual Factors considered in making Dx: Age Gender Family dynamics Culture Language Religion Economic
Immigration Sexual Orientation Trauma Dual dx/comorbid Addiction Cognitive ability Other:___________________
Describe impact of identified factors:_Couple going through difficult time adjusting to have children; each has different gender role expectations for other as
parent based on culturally informed gender roles.
Axis I Primary: 309.4 Adjustment Disorder with Depressed Mood
List DSM Symptoms for Axis I Dx (include frequency and duration for
Secondary: V61.10: Partner relational problem
each). Client meets___5__ of __5___criteria for Axis I Primary Dx.
Axis II:_V71.09 None__________________________________________ 1._ Trigger: AF becoming increasingly unhappy with him following birth of
Axis III: None reported_________________________________________
second child; couple still not adjusted to change.
Axis IV:
2. Periods of sadness/hopeless following arguments (1-4 times/week)
Problems with primary support group: Spouse; parenting
Problems related to social environment/school: Move
3._Periods of irritability and poor impulse control (1-4 days/week)
Educational problems
4. On-going conflict with AF_
Occupational Problems
Housing problems
5. Does not qualify for mood disorder; no bereavement
Economic problems
6. ____________________________________________________
Problems with accessing health care services
Problems related to interactions with the legal system
Medications (psychiatric & medical) Dose /Start Date
Other psychosocial problems
1._NA__________________________/____mg;____________________
Axis V: GAF ___60_____ GARF 55
2.___________________________/____mg;_____________________
Have medical causes been ruled out? Yes No In process
Has patient been referred for psychiatric/medical eval? Yes No
3. __________________________/_____mg;_____________________
Has patient agreed with referral? Yes No NA
List psychometric instruments or consults used for assessment: None or Client response to diagnosis: Agree; Somewhat agree Disagree;
Not informed for following reason:____________________________
__Outcome rating scale_____________________________________
Medical Necessity: Check all that apply Significant impairment Probability of significant impairment Probable developmental arrest
Areas of impairment: Daily activities Social relationships Health Work/School Living arrangement Other:_______________________
Risk Assessment
Suicidality:
No indication
Denies
Active Ideation
Passive Ideation
Intent without plan
Intent with means
Ideation in past yr
Attempt in past yr
Family/peer hx of
completed suicide
Homicidality:
Hx Substance:
Sexual & Physical Abuse and Other Risk Factors:
Current child w abuse hx: Sexual;Physical;Emotional;Neglect
No indication
Alc abuse: No
Adult w childhood abuse: Sexual;Physical;Emotional;Neglect
Denies
indication Denies
Adult w abuse/assault in adulthood: Sexual; Physical; Current
Active Ideation
Past Current:
Passive Ideation
Freq/Amt: _____________ History of perpetrating abuse: Sexual; Physical
Elder/Dependent Adult Abuse/Neglect
Intent w/o means
Drug: No indication
Anorexia/Bulimia/Other eating disorder
Intent with means Denies Past
Cutting or other self harm: Current; Past; Method:_____________
Ideation in past yr Current
Violence past yr
Drugs:________________ Criminal/legal hx:__________________________
Hx assault/temper
Freq/Amt:_____________ None reported
Family/sig.other abuses
Cruelty to animals
Indicators of Safety: At least one outside person who provides strong support Able to cite specific reasons to live, not harm self/other Hopeful
Has future goals Willing to dispose of dangerous items Willingness to reduce contact with people who make situation worse Willing to
implement safety plan, safety interventions Developing set of alternatives to self/other harm
Sustained period of safety: ________ Other:
Safety Plan includes: NA Verbal no harm contract Written no harm contract Emergency contact card Emergency therapist/agency
number Medication management Specific plan for contacting friends/support persons during crisis Specific plan of where to go during crisis
Specific self-calming tasks to reduce risk before reach crisis level (e.g., journaling, exercising, etc.) Specific daily/weekly activities to reduce stressors
2
Other:
Notes: Legal/Ethical Action Taken: NA__________________________________________________________________________________
Case Management
Patient Referrals and Professional Contacts
Has contact been made with Social Worker: Yes No: explain:________________ N/A
Has client been referred for medical assessment: Yes No evidence for need
Has client been referred for psychiatric assessment: Yes; cl agree; Yes, cl disagree Not rec.
Has contact been made with treating physicians or other professionals: Yes No N/A
Has client been referred for social services: Job/training Welfare/Food/Housing Victim
services Legal aid Medical Other:_______________________ N/A
Anticipated forensic/legal processes related to treatment: No; Yes_Potential divorce_________
Has client been referred for group or other support services: Yes No None recommended
Client social support network includes: Supportive family; Supportive partner; Friends;
Religious/spiritual organization; Supportive work/social group; Other___________________
Anticipated effects treatment will have on others in support system?: (Parents, children, siblings, sig.
other, etc.): If couple issues not addressed, likely to affect children’s behavior._________________
Is there anything else client will need to be successful?____________________________________
Date 1st Visit: 11/1/09 Last visit: 11/14/09
Session Freq: Once week Every other
week Other:________________
Expected Length of Treatment:3 months
Client Sense of Hope: Little 1----AF----------------5----AM---------------10 High Hope
If Child/Adolescent: Is Family Involved?
Yes No
Modalities: Individual Adult
Individual Child
Couple
Family
Group: _________
Is client involved in mental health or other
medical treatment elsewhere?
No
Yes:________________________
Expected Outcome and Prognosis:
Return to normal functioning
Expect improvement, anticipate less than normal functioning
Maintain current status/prevent deterioration
Evaluation of Assessment/Client Perspective
How was assessment method adapted to client needs? Used tone, language comfortable for couple; allow each person to share perspective.
Age, culture, ability level, and other diversity issues adjusted for by: Provided opportunity for each to verbalize cultural/gender expectations.
Systemic/family dynamics considered in following ways: Address over/underfunctioning dynamic by allowing each to speak for self; assign AM task of
rescheduling appts.
Describe actual or potential areas of client-therapist agreement/disagreement related to the above assessment: Couple seems to see situation as
personality rather than cultural/gender conflict.
______________________________________________,_______________
Therapist Signature
License/intern status
_____________
Date
______________________________________________,_______________
Supervisor Signature
License
_____________
Date
Abbreviations: AF: Adult Female; AM: Adult Male; CF#: Child Female with age, e.g. CF12; CM# Child Male with age; Hx:
History; Cl: Client.
3
© 2007. Diane R. Gehart, Ph.D. All rights reserved. www.mftcompetencies.org
4 of 4