Psychiatry Inpatient SOAP Note Outline (UK)
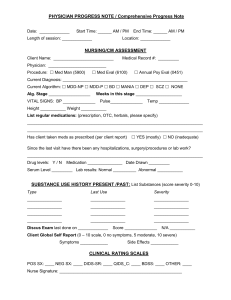
advertisement
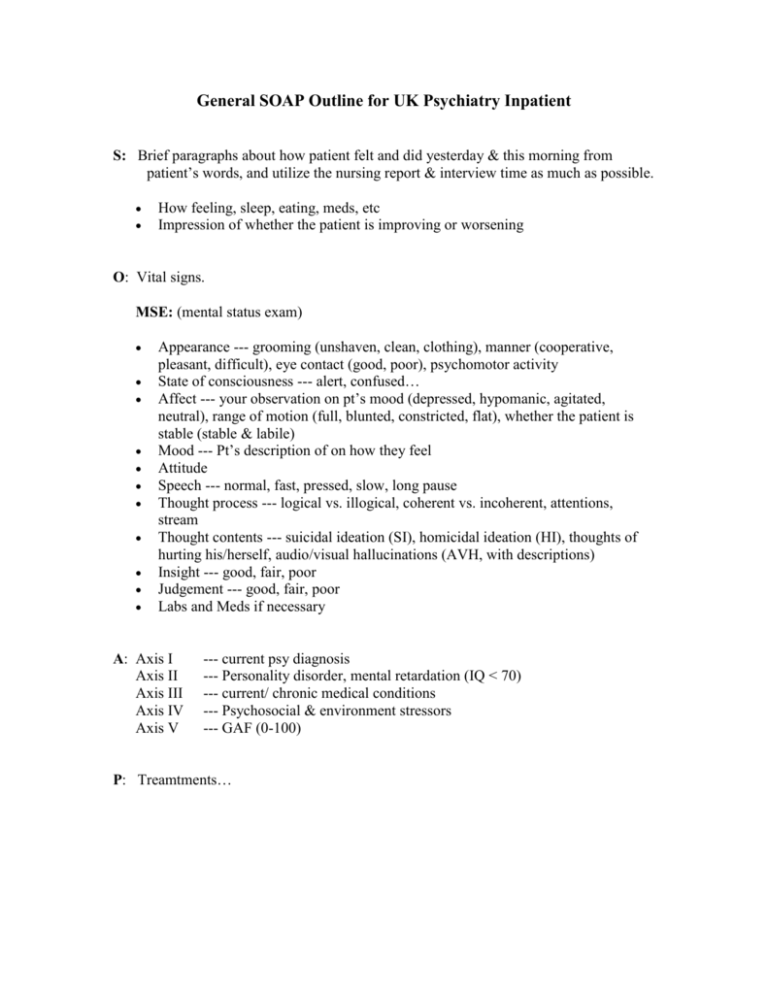
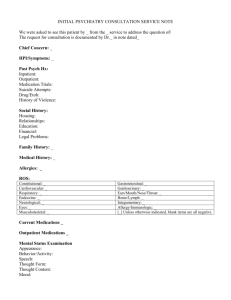
General SOAP Outline for UK Psychiatry Inpatient S: Brief paragraphs about how patient felt and did yesterday & this morning from patient’s words, and utilize the nursing report & interview time as much as possible. How feeling, sleep, eating, meds, etc Impression of whether the patient is improving or worsening O: Vital signs. MSE: (mental status exam) Appearance --- grooming (unshaven, clean, clothing), manner (cooperative, pleasant, difficult), eye contact (good, poor), psychomotor activity State of consciousness --- alert, confused… Affect --- your observation on pt’s mood (depressed, hypomanic, agitated, neutral), range of motion (full, blunted, constricted, flat), whether the patient is stable (stable & labile) Mood --- Pt’s description of on how they feel Attitude Speech --- normal, fast, pressed, slow, long pause Thought process --- logical vs. illogical, coherent vs. incoherent, attentions, stream Thought contents --- suicidal ideation (SI), homicidal ideation (HI), thoughts of hurting his/herself, audio/visual hallucinations (AVH, with descriptions) Insight --- good, fair, poor Judgement --- good, fair, poor Labs and Meds if necessary A: Axis I Axis II Axis III Axis IV Axis V --- current psy diagnosis --- Personality disorder, mental retardation (IQ < 70) --- current/ chronic medical conditions --- Psychosocial & environment stressors --- GAF (0-100) P: Treamtments…