The Lymphatic System and Immunity: Chpt
advertisement

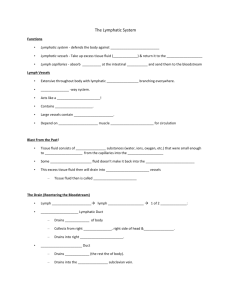
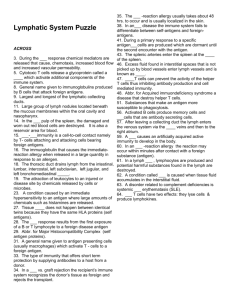
The Lymphatic System and Immunity: Chpt. 22 Pathogen: Fungus: Bacteria Virus Immunity: Consists of: 1. network of lymphatic vessels 2. lymph: similar to interstitial fluid 3. lymphatic tissues & organs 4. Lymphocytes, phagocytes & Functions of Lymphatic System: 1. Production, maintenance, and distribution of lymphocytes 2. Return of fluid and solutes from interstitial fluid 3. Transport of hormones, nutrients Distribution & Structure of Lymph Vessels - form a 1-way system 1. Lymphatic Capillaries (lacteal): similar to systemic blood capillaries except lymphatic capillaries are more lacteals also have thinner walls are found near systemic capillaries endothelial cells overlap and leave “flaps” which open when fluid P> in interstitial space allowing interstitial fluid to enter lymph. cap Proteins and large debris (including bacteria, viruses and cancer cells) easily enter lymph vessels However, lymph takes detours through lymph nodes 2. Small Lymphatic Vessels collect lymph from lymphatic capillaries transport to larger lymphatic vessels larger lymphatic vessels have valves to prevent backflow of lymph often found near arteries and veins 1 superficial and deep lymphatics superficial in subcutaneous layer deep near deep arteries/veins of skeletal muscles lymphangitis: 3. Lymphatic Trunks: collect lymph from the lymphatics major trunks – Lumbar Intestinal Bronchomediastinal R,L Subclavian R,L Jugular Trunks drain lymph into 1 of 2 ducts: 1. Right Lymphatic Duct: collects lymph from the , and trunks , 2. Thoracic Duct: largest begins as an enlarged sac termed the Cisterna Chyli located at L1 which collects lymph from the and trunks. As thoracic duct runs superiorly, accepts lymph from the , and , trunks. Each duct empties lymph into the subclavian veins (R and L) lymphangitis: inflamed lymphatic vessels Lymph Transport: ∙ low pressure ∙ lymph moves one-way ∙skeletal muscle contractions, pressure changes thorax during breathing ∙ valves ∙ arterial pulses ∙ lymphedema: lymph cannot drain due to blockage in limb limb becomes swollen – higher risk of infection in area Lymphoid Cells: • account for 20-30% of all circulating leukocytes (WBCs) • 3 types of lymphocytes: 2 1. T cells (thymus-dependent) – 80% of circulating lymphocytes provide cell-mediated immunity or cellular immunity cytotoxic T cells – attack foreign cells & virus infected cells hand-to hand combat helper T cells – stimulate T & B cells suppressor T cells – 2. B cells (bone marrow-derived) – 10-15% of circulating lymphocytes provide antibody-mediated immunity or humoral immunity when encounter antigen become activated & form 2 types of clones (sensitive to the antigen) plasma cells and memory cells plasma cells make antibodies (immunoglobulins) to attack the antigen memory cells: 3. NK cells (natural killer or large granular) – 5-10% of circulating lymphocytes provide immunological surveillance – “police” Note: lymphocytes circulate in blood, bone marrow, spleen, thymus and lymph tissue. Lymphocyte lifespan 4 - 20 years – new lymphocytes made in bone marrow and lymph tissue 4. Macrophages: 5. Dendritic cells: “Antigen Presenting Cells” Lymphopoiesis: occurs in bone marrow, thymus and peripheral lymph tissue 3 Hemocytoblast generates 2 main types of lymph stem cells – 1.) One group remains in bone marrow: produces immature B cells & NK cells B cells migrate into lymph nodes, spleen & lymph tissue NK cells circulate through peripheral Tissues 2.) The other migrates to the thymus gland to form T cells T cells develop in the thymus gland and then are released to the blood travel to bone marrow, peripheral Lymph Tissues tissues, lymph tissues & lymph • connective tissue with lymphocytes organs • lymphoid or lymphatic nodules densely packed in connective tissue of respiratory, digestive and urinary tracts • examples include MALT (mucosa-associated lymphatic tissue): Peyer's patches and appendix Tonsils ring of lymph. tissue around entrance to pharynx (throat) pharyngeal tonsil or adenoid: palatine tonsils: throat lingual tonsils: back of tongue Lymph Organs 1. Lymph nodes: bean shaped filter and purify lymph before it enters blood (removes 99% of antigens) Each node has a fibrous capsule, a cortex, & a medulla Cortex contains dendritic cells, macrophages and T cells Medulla mostly contains B cells and plasma cells Lymph enters lymph nodes via afferent lymph vessels & exits via efferent vessels. There are fewer efferent vessels than afferent which Largest lymph nodes found in the inguinal, axillary, submandibular & cervical regions of body 4 Sometimes the nodes are overwhelmed and become painful/swollen Tonsillitis: Lymphadenopathy: chronic or excessive enlargement of lymph nodes Lymph nodes can also become secondary cancer sites (lymphoma) 2. Thymus Gland located in mediastinum grows throughout childhood and is largest at puberty then atrophies secretes hormones (thymosins) cause T lymphocytes to become immunocompetent 3. Spleen soft, blood rich organ on lateral border of stomach (9-11th rib) largest lymphatic organ Functions of the spleen: 1. spleen cleanses blood: phagocytosis 2. Stores some iron from breakdown of RBCs 3. Initiates the immune response (immune surveillance) of B & T cells 4. Stores platelets spleen surrounded by fibrous capsule inside of spleen contains red pulp: regions containing macrophages & dendritic cells white pulp: contains lymphocytes Injury to spleen: impact on left abdomen can tear capsule Splenectomy: Immunity: Defenses: Nonspecific vs. Specific Nonspecific: same response to any threat Specific: lymphocytes respond to antigens 5 Nonspecific: (p. 776 figure 22-10): prevent entrance and/or limit spread of pathogens 1. Physical Barriers: keep organisms out of body skin: first line of defense keratin and hair sweat, sebaceous glands: secretions contain lysozyme and antibodies mucus membranes in respiratory, digestive, urinary and reproductive tracts HCl in stomach 2. Phagocytes: first line of cellular defense attack & remove microorganisms before lymphocytes detect their presence microphages: neutrophils and eosinophils normally in blood leave blood and travel to injured/infected tissue respond quickly neutrophils become activated which increases metabolic rate (respiratory burst) and they produce nitric oxide & H2O2 to destroy engulfed pathogens. also release cytokines to attract other neutrophils and macrophages to area macrophages: larger, derived from monocytes (leukocyte) Activated Macrophages: 1. Adhere to pathogen & engulf it to destroy it in lysosome Opsonization: complement or antibodies coat pathogen 2. bind to pathogen to "hold" it for other cells to help destroy it 3. release toxic chemicals (cytokines) to destroy pathogen (tumor necrosis factor, defensins) fixed vs. free: fixed include Langherhans cells, microglia and kupffer cells free or mobile: dust cells and those that circulate in blood 6 Movement of microphages & free macrophages: • diapedesis – move through capillary walls out of blood • chemotaxis • adhesion: phagocyte must first attach to target 3. Immunological surveillance: cell (pg. 778 figure 22-11) natural killer (NK) cells: recognize and destroy abnormal cells (via antigens) in peripheral tissues can destroy many types of cells recognizes abnormal cell, adheres to it, produces and releases perforins (exocytosis) which destroys cell membrane of abnormal cell (rotates golgi apparatus to “aim” at cell and then releases perforin proteins) 4. Interferons (cytokines): alpha (), beta() and gamma () interferons •small proteins released from activated lymphocytes, macrophages and cells infected with virus •releases antiviral proteins to healthy cells – inhibit viral replication •also stimulate NK cells and macrophages 5. Complement: • 11 plasma proteins • once activated this system causes a complement cascade which eventually: 1. forms MAC 2. release of histamine 3. attracts neutrophils and macrophages to area 4. facilitates phagocytosis – coating of complement proteins & antibodies makes it easier for phagocyte to adhere/engulf Assist with opsonization 6. Inflammatory Response: 4 signs of inflammation: vasodilation of blood vessels: mast cells release histamine - increased permeability of blood vessels: 7 leukotrienes & prostaglandins also released for inflammation why beneficial? (see tissue notes) 7. Fever: temperature >37.2o C or 99o F pyrogens: circulating proteins, toxins, antibody complexes cause hypothalamus to reset temperature – Endogenous pyrogens = interleukin-1 (IL-1) pyrogen released by active macrophages a cytokine beneficial because: increases metabolism, accelerates defenses inhibits some viruses and bacteria Immunity (specific resistance) Responds to specific antigens – with coordinated action of T and B cells Cellular Immunity: T cells (lymphocytes) : provide cell-mediated immunity directly kill cells indirectly by releasing cytokines Humoral Immunity: B cells (lymphocytes): provide antibody-mediated immunity Antigens: Proteins, polysaccharides, lipids, nucleic acids Mobilize immune system Complete Antigens: Immunogenicity: Stimulate antibody formation Reactivity: react with activated lymphocytes & antibodies Antigenic determinants: Hapten: incomplete antigen Usually doesn’t trigger immune response unless attached to protein Poison ivy & animal dander Self-Antigens: MHC Proteins: glycoproteins MHC Class I: proteins in cell membranes of all nucleated cells -peptide displayed is synthesized within the cell (endogenous) -displays peptides from cellular protein recycling (T cells ignore normal peptides) - if cell is infected it will display the protein and T cell will recognize it and be activated – abnormal peptides activate T cell 8 also occurs during organ rejection Tolerance: immune system doesn’t respond to some antigens – ignores self-antigens and nonharmful antigens Forms of Immunity: Innate: Acquired: Active vs. Passive Passive Immunity: • naturally acquired • artificially acquired (induced) Active Immunity: • naturally acquired • artificially acquired (induced) Specific Defenses and Immunity: T and B cells T Cells: Cell-Mediated Immunity protect against abnormal cells or pathogens inside of our cells 3 Types of T cells: 1.) Cytotoxic: TC or CD8 2.) Helper T: TH or CD4 3.) Suppressor T: TS 1. Cytotoxic: TC or CD8 directly attack foreign cells or cells infected with viruses use physical and chemical methods 9 BUT: must be activated first (this is done by antigen presentation through MHC proteins or HLAs) Note: must be costimulated to be activated T cells respond to either class I or class II antigens (page 789 figure 22-19) CD8 cells activated by class I antigens CD4 respond to class II antigens Once activated form killer T cells and memory T cells Killer T cells release chemicals to destroy cell perforins lymphotoxin activate genes to stimulate cell to die (apoptosis) slow response time Memory T cells: Produced with cytotoxic T cells immediately form cytotoxic T cells if exposed to same antigen again 2. Suppressor TS release suppression factors to limit the immune response inhibit responses of T and B cells Act after initial immune response 3. Helper: TH or CD4 once activated divide to form: active helper T cells & memory helper T cells Activated helper T cells release cytokines which: 1. stimulate production & maturation of killer T cells 2. attract macrophages to area 3. stimulate and attract NK cells 4. stimulate B cell to make antibodies 10 B Cells: antibody-mediated or humoral immunity B cells attack antigen by producing specific antibodies B cell must first be activated or sensitized (usually in lymph node) - Requires helper T cell Once sensitized produces clones that will become: 1. plasma cells: make and secrete antibodies against the antigen (2000 molecules/second) Antibodies released into interstitial fluid & circulate in blood or lymph 2. memory cells: remain for second exposure to antigen Immunoglobulins: antibodies Structure: 2 heavy parallel polypeptide chains: heavy & light Each chain has constant (stem) and variable region Constant region determines antibody class Antigen-antibody complex 5 classes: IgG, IgE, IgD, IgM and IgA IgG: most numerous in plasma (accounts for aprx. 80%) protects against viruses, bacteria & toxins Main antibody of secondary response Only one to cross the placenta IgE: triggers release of histamine & inflammatory chemccals from mast cells allergic reactions, asthma chronic parasitic infections in GI tract IgM: first antibody secreted during primary response IgA: found in saliva, mucus, tears Complete antigen vs. hapten: Complete antigen binds to both antigen binding sites Hapten: Small molecule that triggers immune response by linking to other protein (carrier) Dangers of Haptens Antibodies produced will attack both hapten and its linked protein If carrier is “normal” Antibody attacks normal cells For example, penicillin allergy, poison ivy, detergents, etc. 11 Antibody Effects: 1. Neutralization: bind to pathogen site so pathogen cannot bind to other cells effective at preventing viral and toxin binding to host cells 2. Agglutination and precipitation: binds to several antigens and clumps them together 3. Activate complement 4. Attract phagocytes 5. Opsonization: antibodies surround/coat pathogen so phagocytes can grab and ingest it more easily 6. Stimulate inflammation: via mast cells 7. Prevent bacteria and viruses from adhering to cells mainly IgA in saliva etc. prevents binding/entrance of pathogens Primary vs. Secondary Responses to Antigen Exposure Immunological competence: the ability to produce an immune response after exposure to an antigen Form antibodies (antibody titer) Note: monoclonal antibodies used in research, clinical testing, treatment Important Cytokines (pg. 799 table 22-3) 1. Interleukins (IL-2 etc) produces by leukocytes and macrophages stimulate T and B cell activity increase antibody production trigger fever and inflammation 2. Interferons resistance to viral infections stimulate NK cells and macrophages 3. Tumor necrosis factors (TNFs) slow tumor growth, can kill tumor cells cause fever, increase neutrophil production 12 stimulate T cells activation 4. Perforin 5. Lymphotoxins 6. Leukotrienes stimulate inflammation Response to Bacterial Infection Defense Against Bacterial and Viral Pathogens 13 Summary of Immune Response 14 Clinical Aspects of the Immune System 1. Immunodeficiency diseases: Severe combined immunodeficiency disease (SCID) AIDS: - HIV infection Immunosuppressive Drugs: 2. Autoimmune Disorders: B cells produce autoantibodies Can be due to decreases suppressor T cells Increased stimulation of helper T cells Tissue damage Examples: thyroiditis, rheumatoid arthritis, insulin-dependent diabetes mellitus, multiple sclerosis, lupus 3. Allergies excessive immune response to antigen (allergens) 15 usually IgE antibody response may be genetic response releases histamine, heparin, cytokines etc. 4 categories of allergic reactions: 1.) Type I: immediate hypersensitivity Rapid & severe response to antigen (allergen) IgE binds to mast cells & triggers release of histamine increased capillary permeability cause swelling (hives) smooth muscles contract in respiratory passageways - difficulty breathing Can be local or systemic Local: histamine: runny nose, watery eyes, itchy, hives If allergen inhaled: bronchoconstriction Tx: antihistamine, benedryl, corticosteroids Systemic anaphylaxis: (pg. 801 figure 22-26) allergen activates mast cells throughout the body – when allergen is in the blood vasodilation can be so great as to drop BP and cause anaphylactic shock bronchoconstriction restricts air flow Tx: Epi 2.) Type II (subacute hypersensitivity): cytotoxic reactions Caused by IgG and IgM Slower onset (1-3 hours, longer duration) Blood transfusion reaction 3.) Type III: immune complex disorders Antigens widely distributed throughout the body Results in numerous antibody-antigen complexes, can’t be removed Causes inflammation and cell lysis by neutrophils Glomerulonephritis, systemic lupus erythematosus, and rheumatoid arthritis. 4.) Type IV: delayed hypersensitivity Slowest to appear (1-3 days) Caused by cytokines (antihistamines don’t work), corticosteroids help Allergic contact dermatitis (caused by haptens: poison ivy, detergents, etc) Tine test for tuberculosis Stress and the Immune System: caused by CRH and ACTH: glucocorticoids secreted to limit response- chronic secretion interferes with immune function 16 1. depression of inflammatory response: 2. decreased number and activity of phagocytes: 3. inhibition of interleukin secretion: 4. decreased production of antibodies Aging and the Immune System Immune system diminishes with age, increasing vulnerability to infections and cancer Thymic hormone production is greatly reduced T cells become less responsive to antigens Fewer T cells reduces responsiveness of B cells Immune surveillance against tumor cells declines Nervous & Endocrine System adjust sensitivity of Immune System How to have a healthy immune system: Don’t be too clean!! The “hygiene hypothesis” Rest/De-stress Diet Supplements Laugh ↑ number & activity of cytotoxic T cells that attack viral infected cells, cancer & tumor cells ↑ number of NK cells ↑ activated T cells ↑ IgA ↑ gamma interferon ↑antibody formation ↓ cortisol 17