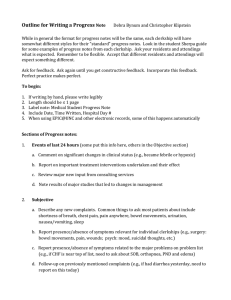
Tips for Writing a Progress Note
advertisement

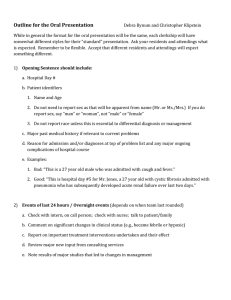
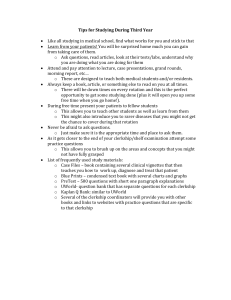
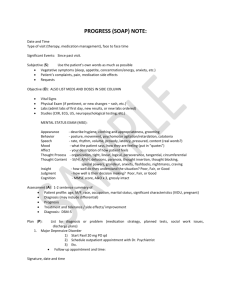
Outline for Writing a Progress Note Debra Bynum and Christopher Klipstein While in general the format for progress notes will be the same, each clerkship will have somewhat different styles for their “standard” progress notes. Look in the student Sherpa guide for some examples of progress notes from each clerkship. Ask your residents and attendings what is expected. Remember to be flexible. Accept that different residents and attendings will expect something different. Ask for feedback. Ask again until you get constructive feedback. Incorporate this feedback. Perfect practice makes perfect. To begin: 1. 2. 3. 4. 5. If writing by hand, please write legibly Length should be ≤ 1 page Label note: Medical Student Progress Note Include Date, Time Written, Hospital Day # When using WebCIS at UNC, some of this happens automatically Sections of Progress notes: 1. Events of last 24 hours (some put this info here, others in the Objective section) a. Comment on significant changes in clinical status (e.g., became febrile or hypoxic) b. Report on important treatment interventions undertaken and their effect c. Review major new input from consulting services d. Note results of major studies that led to changes in management 2. Subjective a. Describe any new complaints. Common things to ask most patients about include shortness of breath, chest pain, pain anywhere, bowel movements, urination, nausea/vomiting, sleep b. Report presence/absence of symptoms relevant for individual clerkships (e.g., surgery: bowel movements, pain, wounds; psych: mood, suicidal thoughts, etc.) c. Report presence/absence of symptoms related to the major problems on problem list (e.g., if CHF is near top of list, need to ask about SOB, orthopnea, PND and edema) d. Follow-up on previously mentioned complaints (e.g., if had diarrhea yesterday, need to report on this today) e. Omit non-essential complaints (e.g., if your patient is upset that his TV is broken, mention this to the appropriate person outside of rounds to help address the problem - this does not need to be written in progress note) 3. Objective a. Physical exam i. List vital signs (give ranges when appropriate, T max and current, include ins/outs) ii. Describe general appearance iii. Report “standard” physical exam from that morning. Ask during each clerkship what should be included in a standard follow-up exam. iv. Emphasize presence/absence of specific exam findings pertinent to major items on problem list (e.g., if CHF is near top of list, need to comment on JVD, crackles, gallops, edema) b. Labs / Studies i. List all lab and study results. Highlight those that result in changes in management. ii. Start with basic labs first. CBC chem 10 LFTs coags other blood labs urine EKG CXR major studies (radiology or biopsy results) c. 4. Events of last 24 hours (if not listed as first part of note above) Medication list (from Medication Administration Record) a. Include complete, up-to-date list b. Include planned finish date for relevant meds (e.g., day 4/10 of vancomycin) c. Include frequency of use for important as needed medications (e.g., list how much pain medication a patient required) 5. Summary statement as first line of Assessment a. Name, Age b. Reason for admission and/or state the working diagnosis if known for major items on problem list 6. Assessment a. Some like to have separate Assessment and Plans sections while others like to link assessment and plan together for each problem on the list b. Organize by problem list, not by organs/systems (e.g., “pneumonia” instead of “pulmonary”) c. Start with the currently most important problem first and report in order of decreasing importance (order of list might change from day to day) d. Use most specific label you can for each problem e. Assess and synthesize, do not just summarize. Demonstrate your thinking of the differential diagnosis and the clinical approach to the major problems f. Include the status of each problem (improving, deteriorating, stable) 7. Plans a. Make an actual plan for the day. Do not just make an assessment and then look for help generating a plan on rounds. b. Include work-up and treatment plans based upon differential diagnosis of each problem. c. Review your plans with your intern/resident so that you have the most up-to-date information and can create plans that will be considered reasonable. d. Include Social Work needs / Discharge planning as last “problem” on list. 8. Sign note a. If handwriting, also print name next to signature. b. If have pager, include pager number as well.