Outline for the Oral Presentation
advertisement
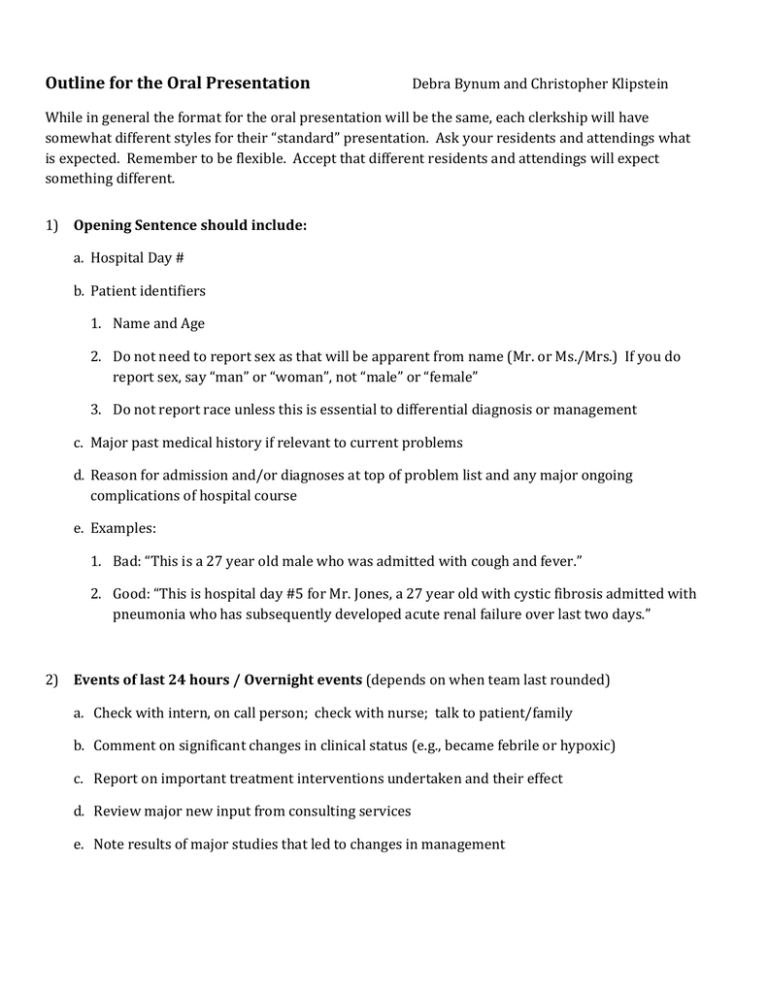
Outline for the Oral Presentation Debra Bynum and Christopher Klipstein While in general the format for the oral presentation will be the same, each clerkship will have somewhat different styles for their “standard” presentation. Ask your residents and attendings what is expected. Remember to be flexible. Accept that different residents and attendings will expect something different. 1) Opening Sentence should include: a. Hospital Day # b. Patient identifiers 1. Name and Age 2. Do not need to report sex as that will be apparent from name (Mr. or Ms./Mrs.) If you do report sex, say “man” or “woman”, not “male” or “female” 3. Do not report race unless this is essential to differential diagnosis or management c. Major past medical history if relevant to current problems d. Reason for admission and/or diagnoses at top of problem list and any major ongoing complications of hospital course e. Examples: 1. Bad: “This is a 27 year old male who was admitted with cough and fever.” 2. Good: “This is hospital day #5 for Mr. Jones, a 27 year old with cystic fibrosis admitted with pneumonia who has subsequently developed acute renal failure over last two days.” 2) Events of last 24 hours / Overnight events (depends on when team last rounded) a. Check with intern, on call person; check with nurse; talk to patient/family b. Comment on significant changes in clinical status (e.g., became febrile or hypoxic) c. Report on important treatment interventions undertaken and their effect d. Review major new input from consulting services e. Note results of major studies that led to changes in management 3) Subjective / Review of Systems a. Describe any new complaints. Common things to ask most patients about include shortness of breath, chest pain, pain anywhere, bowel movements, urination, nausea/vomiting, sleep b. Report presence/absence of symptoms relevant for individual clerkships (e.g., surgery: bowel movements, pain, wounds; psych: mood, suicidal thoughts, etc.) c. Report presence/absence of symptoms related to the major problems on problem list (e.g., if CHF is near top of list, need to ask about SOB, orthopnea, PND and edema) d. Follow-up on previously mentioned complaints (e.g., if had diarrhea yesterday, need to report on this today) e. Omit non-essential complaints (e.g., if your patient is upset that his TV is broken, mention this to the appropriate person outside of rounds to help address the problem - this does not need to be presented on rounds) 4) Physical exam a. List vital signs (give ranges when appropriate, T max and current, include ins/outs if important) b. Describe general appearance c. Report “standard” physical exam from that morning. Ask during each clerkship what should be included in a standard follow-up exam d. Emphasize presence/absence of specific exam findings pertinent to major items on problem list (e.g., if CHF is near top of list, need to comment on JVD, crackles, gallops, edema) 5) Labs/Data: a. Report all labs that result in changes in management b. Ask if should present all other data or only abnormals. If want all, ask if a lab is normal if it ok to just say “normal” or if need to give actual number. c. Start with basic labs first. CBC chem 10 LFTs coags other blood labs urine EKG CXR 6) Major Studies: Do not need to report any results already mentioned above. If normal, usually ok just to say so. 7) Current Medications (from Medication Administration Record) a. Include complete, up-to-date list b. Include planned finish date for relevant meds (e.g., day 4/10 of vancomycin) c. Include frequency of use for important as needed medications (e.g., list how much pain medication a patient required) 8) Consider a brief summary statement (if all the above is relatively short, might just skip to #9) a. Name, Age, Reason for admission and/or state the working diagnosis if known for major items on problem list and any major ongoing complications of hospital course (e.g., “Mr. Jones is an 82 year old gentleman here with pneumonia and resolving acute kidney injury.”) 9) Then state, “The assessment and plan by problem list is…” 10) Stick to your problem list! a. Start with the currently most important problem first and report in order of decreasing importance (e.g., “Problem #1, Pneumonia…give assessment and plan for this problem…Problem #2, Resolving AKI…give assessment and plan…”). Order of list might change from day to day. b. Use most specific label you can for each problem. 11) For your assessments: a. Assess and synthesize, do not just summarize. Demonstrate your thinking of the differential diagnosis and the clinical approach to the major problems. b. Include the status of each problem (improving, deteriorating, stable). 12) For your plans: a. Make an actual plan for the day. Do not just make an assessment and then look for help generating a plan on rounds. b. Include work-up and treatment plans based upon differential diagnosis of each problem. c. Review your plans with your intern/resident prior to rounds so that you have the most up to date information and can create plans that will be considered reasonable. d. Include Social Work needs / Discharge planning as last “problem” on list