Orthopaedics 2 – Joints Structure, Function and Healing

Orthopaedics 2 – Joints: Structure, Function and Healing
Anil Chopra
1.
Recall previous knowledge of the different types of joints including diarthroidal, synovial, fibrous and syndesmoses
2.
Describe the function of synovial joints
3.
List the types of motion that can occur, both active and passive
4.
Outline the two main mechanisms involved in the failure of a joint; osteoarthritis and rheumatoid arthritis
Joint: location where two bones meet. They are constructed to allow movement and provide mechanical support.
Functions :
They allow motion between rigid segments (Bones are rigid and bend little) & thus most joints in the limbs (appendicular skeleton) have a large range of motion usually in one plane. Most joints in Axial Limb have limited movement.
Absorbing shock - The joints help reduce the magnitude of the deceleration from bone to bone e.g. on rapid decelerations of part of the skeleton - as when the foot hits the ground
Allow Growth
Key requirements in a joint:
Mechanisms to reduce wear
Mechanisms to reduce friction
Mechanisms for lubrication
Componants of joints:
Bone Ends
Ligaments
Synovial membrane
Cartilage
Meniscus
Blood vessels
Nerves
Muscles
Functional and structural organization:
Articular cartilage
capsule and synovial fluid
ligaments and tendons
muscles and nerves
command centre/Brain
Types of Joints
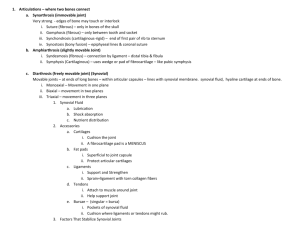
Classifications of joints: a) The Anatomical classification
Joints held by bone - Synostosis e.g. frontal bone of skull
Fibrous Joints – varying degrees of motion. 1) Joints held by fibrous connective Tissue
- Syndesmosis e.g. inferior tibio-fibial joint. 2) Suture - when bones are quite close together with minimum fibrous connective tissue, eg. Joints between cranial bones
Joint held by cartilage tend to be non-movable: 1) Synchondrosis - joints held together by hyaline cartilage e.g. epiphyseal plate. 2)Symphysis – bones held together by disc of fibrocartilage, e.g. pubic symphysis
Joint held by fluid in cavity ( Synovial Joints )
b) The Numbers of bones involved
Simple: 2 articular surfaces, 1 convex (male) the other concave (female)
Compound: More than 2 articular surfaces c) The Shape of bone ends
Hinge joints, e.g. Fingers, knees, elbows, & toes, allow only bending and straightening movements.
Pivot joints, such as the neck joints, allow limited rotating movements.
Ball-and-socket joints, such as the shoulder and hip joints, allow backward, forward, sideways, and rotating movements.
Ellipsoidal joints, e.g. the wrist joint, allows all types of movement except pivotal movements d) The Degrees of freedom
Moves in one plane (elbow) - uniaxial
Moves in two planes - biaxial
Moves in three planes - triaxial e) Classification by function:
Movements at two bone ends are made up of:
Gliding of one surface over another
slide
Angulation of one surface over another
roll
Rotation about bone axis
spin
Limitation of joint movement:
By using up articular surfaces
By adjacent soft tissues
By pain and stretch receptors in ligaments and muscles (Hilton’s law says that joints and muscles share a nerve supply
Muscle paralysis
Spastic paralysis – movement restricted
Assessing joint movement:
Planes of movement, sagittal, coronal, horizontal
Flexion: to bend or make an angle
Extension: to straighten
Abduction: Draw away from median plane
Adduction: move towards median plane
Pronation: Turn hands so palm faces backwards
Supination: Turn the hand so palm faces forwards
Circumduction: A combination of abduction, adduction, flexion and extension
Function of synovial joints
Synovial joints are the most common joints of the body. The key structure is articular cartilage, which is avascular, alymphatic & aneural. It contains:
Cells (5%) - Chondrocytes
Extracellular matrix (95%) – Water (75%), Collagen (mainly type 2 – 5%),
Proteoglycans (20%), Lipids, Adhesives (fibronectin, chondronectin),
Enzymes & Growth Factors (PDGF, TGF beta, FGF, IGF-1).
Synovial fluid is a dialysate of plasma without clotting factors secreted by the synovial membrane (found lining the joint). It is viscous, elastic, plastic and provides nutrition to chondrocyte. It contains hyaluronic acid & plasma proteins and acts as an immune system pH buffer and a lubricant.
The joint also has a fibrous capsule to prevent leakage, local joint ligaments and local apertures e.g. bursa.
Function of Muscles
The two main functions of muscle are movement and stability.
Articular Cartilage
Articular cartilage can be damaged causing either:
Deep lacerations - Extend below the tidemark & heal with fibrocartilage though blunt trauma may cause osteo-arthritic changes
Superficial lacerations- Above the tidemark. Chondrocytes proliferate but do not heal due to lack of blood supply, thus immobilisation leads to atrophy while continuous passive motion is beneficial to healing.
Disease of articular cartilage: Osteoarthritis
Degeneration and breakdown of the cartilage, the cartilage surface breaks down.
Fibrils form.
The chondrocyte maintains structure and function of cartilage.
Joints of Upper Limb
» Sternoclavicular joint: fibrous with an interosseous disc
» Acromioclavicular joint: fibrous.
» Shoulder: synovial ball and socket
» Humero-ulnar joint – hinge
» Proximal Radio-ulnar – syndesmosis (interosseous membrane)
» Distal radio-ulnar – pivot joint
» Wrist – synovial
» Fingers – hinge synovial.
Other Joints
» Spinal Vertebrae – inter-membranous discs
» Sacroiliac – between sacrum and ilium
» Hip joint – ball and socket
» Knee Joint – subcutaneous,
» Patello-femoral joint -
» Ankle – hinge joint
Trauma and Joint Failure
Different types of joint damage:
Trauma o Simple or High Energy
Degenerative – bone growth
Inflammatory (Rheumatologists)
Infective
Neoplastic
Examples of trauma:
Elbow dislocation
Shoulder dislocation
Ankle dislocation
Ligament injuries: o Torn medial collateral: results in a valgus deformity (outward deangulation of the bone).
When joints are damaged, abnormal stresses are placed on them which results in bleeding and inflammation.
Osteoarthritis
Primarily occurs because of loss of cartilage mainly due to degradation of collagen.
With Age cartilage becomes increasingly hypocellular and loses elasticity. The chondrocytes increase in size & increase secretions of lysosomal enzymes.
Proteoglycans decrease in mass and size reducing the length of chondroitin sulfate chains but increasing the amount of keratin sulfate. Levels of hyaluronic acid decrease with reduced water content decreases (increases in OA) while the protein content increases.
Osteoarthrits is non inflammatory degenerative disorder.
There is progressive loss of articular cartilage, associated new bone formation and capsular fibrosis.
Mechanisms:
increased stress on normal cartilage – increased load (weight, activity), decreased area (varus knee, dysplastic hip)
Weak cartilage with normal stress – age, stiff (eg – ochronosis), soft (eg – inflammation), abnormal bony support (eg – AVN)
Rheumatoid arthritis
Pathology:
Synovitis – chronic inflammation, synovial hypertrophy, effusion
Destruction – proteolytic enzymes, pannus
Deformity – articular destruction, capsular stretching, tendon rupture
Examination and Investigation
Inspection
Palpation
Examination of movement
Special tests
Examination of radiographs
Arranging further investigations
X-ray
Show bones
CT scan
3D imaging
Reconstructive CT can give further information.
MRI scan
Soft tissue including the inflammatory responses.
Other Scans
Isotope and DEXA
Arthroscopy
Treatment
Osteotomy – bone is cut to re-align, shorten or lengthen it. It is commonest done in hallux valgus.
Arthrodesis – the artificial induction of bone ossification. Not the first choice.
This is done to fuse the bones and stop pain (sub talar or spine)
Excision – hand, carpal-metacarpal joint, psudoarthrodesis. Makes a false joint
(i.e. Kellers in foot), or excision of trapezium in the hand. It may weaken the hand but it is pain free.
Partial or total joint replacement .
Physiotherapy to strengthen muscles
Painkillers