Review of Physiology II
advertisement

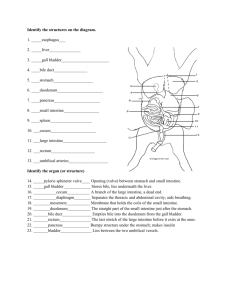
GI 2 #4 2/23 11am Gwirtz Margaret Veach for Robert Abbate Page 1 of 11 Review of Physiology II I. Motility in the Small Intestine 2 forms: Mixing and Propulsive A. Mixing or Segmentation Contractions Most important and common contraction in the stomach • Distention (the chyme against the wall is the stimulus) • Breaks up chyme to increase surface area • Mixes chyme with secretions and presents digestive materials to mucosa to be absorbed • Rate related to electrical slow waves initiated by interstitial cells of Cajal (pacemaker cells) in longitudinal layer: • duodenum 12-14/min • ileum 8-9/min • Myenteric plexus will occur in absence of extrinsic or parasymp. nerves B. Propulsive (Peristaltic) Contractions – Distention (stretch) initiates – Usually weak »die out after few cm – Parasympathetic and myenteric nerves – Influenced by nervous signals, hormonal factors influence the relative degree of depolarization or hyperpolarization of sm. muscle cell. C. Law of the Intestine – chyme moves analward b/c the rate of contractions is faster at duodenum than at the terminal ileum. II. Secretions of Small Intestine For Test: the Small intestine does NOT secrete enzymes, there are enzymes adhered to the microvilli brushborder, but they are not secreted into the lumen. 1-2 liters daily Stimulus: distension or irritation by hypertonic or acidic chyme Isotonic; mostly water, some mucous; enzyme poor Brunner’s Glands – lst few cm of duodenum – Secrete alkaline mucus Crypts of Lieberkuhn – mucous from goblet cells and serous secretion from epithelial cells secrete an extracellular fluid, 1800 ml daily – watery vehicle for absorption of substances, actions of the enzymes of the pancreas and brush border enzyme A. Small Intestine - Enzymes GI 2 #4 2/23 11am Gwirtz Margaret Veach for Robert Abbate Page 2 of 11 Located on brush border Peptidases break peptides into a.a., sucrase, maltase, iosmaltase, lactase these 4 break disaccharides into glucose, galactose, and fructose intestinal lipase, enterokinase-the brush border enzyme which activates trypsinogen to tyrpsin Digestion/absorption disorders when absent. Dz like Celica Sprue which damages the brush border and you get malabsorption from the loss of enzymes and nutrients can’t be adequately digested/absorbed.. Also, the genetic disorder” Lactate Deficient: lactose goes to the colon, where it’s fermented and you get gas and diarrhea. III. Pancreatic Exocrine Secretion 1-1.5 liters daily Digestive Enzymes: Acini secretes the enzymes Proteases: secreted in inactive form; requires enterokinase for activation; trypsin inhibitor prevents autodigestion of pancreas: trypsin, chymotrypsin, etc… Amylases (cannot digest cellulose) starches Lipases, cholesterol esterase lipids, triglycerides Bicarbonate Ions, Water: Epithelial cells of ducts. The bicarb is essential for the buffering of gastric acid. If the acid wasn’t buffered, then all the enzymes would be inactivated. Slide 33: Pancreatic Secretions: See the acinus(at the top), enzymes are released and the secretions travel through the pancreatic ductal cells, where the secretion is modified. There is an active Cl-Bicarb exchange in the main collecting duct. And there is a Secretin-stimulated secretion of Na, K, HCO3, Cl. When the ductal cells are stimulated by secretin, then bicarb secretion is stimulated. When the solution sits in the duct, there is an exchange of bicarb for Cl. During max stimulation, there is less time to modify the secretions, so there is a high secretion of bicarb and enzymes. Slide 34 Trypsinogen (inactive)----membrane-bound enterokinase activatesTrypsin (active) Trypsin autoactivates itself and other proteolytic enzymes to digest protein: Chymotrypsinogen-----trypsin activates Chymotrypsin (active) Procarboxypeptidase (inactive) trypsin activates Carboxypeptidase Slide 35: During cephalic and gastric phases, stimulation by vagal nerve fibers cause release of pancreatic juice 1. Acidic chyme enters duodenum, causes the enteroendocrine cells of the duodenal wall to release secretin, whereas fatty, protein-rich chyme induces release of cholecytokinin. 2. Cholecystokinin and secretin enter bloodstream 3. Upon reaching the pancreas, cholecystokinin induces the secretion of enzyme-rich pancreatic juice; secretin causes copious secretion of bicarb-rich pancreatic juice. CCK leads to acini secretion of enzymes. Secretin leads to the ductal cell secretion of bicarb. A. Cholecystokinin (CCK) GI 2 #4 2/23 11am Gwirtz Margaret Veach for Robert Abbate Page 3 of 11 Secreted by cells in duodenum & upper jejunum in response to fats, proteoses & peptones in chyme cause Enzymes to be secreted from pancreas Effects potentiated by vagal stimulation and secretin CCK also contraction of gallbladder and relaxation of Sphincter of Oddi B. Secretin Secreted by S-cells in duodenum & upper jejunum in response to acid, hyper/hypotonic chyme, and fat Bicarbonate ions, water - stimulated formation of cAMP Effects potentiated by vagal stimulation and CCK Secretin also bile duct secretion of HCO3 and intestinal secretion of fluid Student Question: Is the secretion stimulated primarily by fat or acid? Answer: Mainly by Acid IV. Bile Secretion by the Liver the picture slide of the liver: take home note: The liver has hepatocytes that secrete bile into bile ducts. 600-1200 ml/day Secreted in two stages: Hepatocytes secrete bile This is the bile-dependent fraction Bile ducts secrete water/electrolyte This is the bile-independent fraction high concentration of HCO3-, water, other electrolytes stimulated by secretin Cholesterol primary bile acids secreted by liver into intestine bacteria convert to secondary bile acids in the small intestine Bile acids conjugated to bile salts (ionized) Storage in gallbladder liver produces 900 ml daily while gallbladder can hold 60 ml Bile concentrated 12-20 X by active absorption of Na+ (with Cl- and water) when stored in the gallbladder. A. Enterohepatic Circulation of Bile The liver can’t make enough bile in one day to meet the body’s needs, so the enterohepatic circulation solves that problem. Liver syn and secretes the bile and the bile is stored and concentrated in the gallbladder, during the interdigestive period. During Digestion, the gallbladder contracts and the Sphincter of Oddi relaxes, releasing the bile into the duodenum. The duodenum we have emulsification and digestion of fats. In the terminal ilum, there is active absorption of bile acids by a Na cotransport mechanism. The bile acids return to the liver in portal circulation and the bile acid is resecreted. When you eat a meal that’s high in lipid content, you could be using the same bile 3-4 times! -only 5% of bile acid is lost in feces, the other 95% is recycled. GI 2 #4 2/23 11am Gwirtz Margaret Veach for Robert Abbate Page 4 of 11 Slide 42: Mech promoting secretion of bile and its entry into the duodenum 1. Acidic, fatty chime enters duodenum and causes release of CCK (from fatty) and secretin (from acidic) from duodenal wall enteroendocrine cells. 2. CCK and secretin enter the blood stream. Secretin causes bile ducts to secrete bile salts and water 3. Bile salts and secretin transported via bloodstream, stimulate liver to produce bile more rapidly. 4. Vagal stimulation causes weak contraction os gallbladder 5. CCK (via bloodsteam) causes gallbladder to contract and hepatopancreatic sphincter to relax; bile enters duodenum 6. Bile salts reabsorbed into blood. New Slide: Liver Functions: 1. Bile secretion 2. Metabolism: CHO, Lipids, proteins 3. Detoxification of blood: drugs (inactivation) hormones 4. Plasma protein synthesis 5. Storage: glycogen, Vit A,D, K, B12, Iron Slide 43: Digestive Period: Late Intestinal Phase -No salivation, stomach’s empty Gastrin levels to baseline Pancreatic secretions CCK levels are at baseline ↑ Secretion of bile salt from liver ↑ volume of bile in gallbladder Haustrations, contractions in the large intestine Absorption of water and electrolytes, in proximal colon In distal colon: storage of fecal matter until appropriate time of defecation. Slide 44: Anatomy of colon The long smooth muscle is not continuous around the colon, it is in 3 lengths of teniae coli. Receptors in the rectum are sensitive to the consistency of the feces, can detect solid, liquids, gases. The External Sphincter is skeletal muscle and the internal sphincter is smooth muscle. Skeletal muscles associated with the GI tract: tongue, VES, upper regions of esophagus, external anal sphincter V. Large Intestine Secretions Crypts of Lieberkuhn: serous secretion Mucous cells secrete mucus with large concentration of bicarbonate ions to buffer acid from bacterial digestion of unabsorbed material in the colon. No villi No enzymes GI 2 #4 2/23 11am Gwirtz Margaret Veach for Robert Abbate Page 5 of 11 Stimuli - tactile, pelvic nerves (parasympathetic) Irritation results in secretion of large volume of water and electrolyes, causing diarrhea, ex. lots of bile salt is an irritant VI. Movements of the Colon A. Mixing Movements - Haustrations Bulging out like bag-like sacs Move slowly analward Myogenic; myenteric plexus Sluggish (4-6 per min) Dig into fecal material to allow maximal absorption of water and electrolytes: the majority of the water is absorbed in the SI, the colon has a huge capacity to absorb H20. -Rate increases as you go along the length of the colon, with contractions greater in the rectum. Impt b/c: If you fail to defecate, the fecal matter can back up into the distal colon and not sit in the rectum. Propulsive “Mass” Movements: which is a peristaltic contraction Usually occur 1-3 times daily, especially 15 min after eating breakfast Initiated by gastrocolic, duodenocolic reflexes, irritation Transmitted through parasympathetic (pelvic) nerves and myenteric plexus Modified type of peristalsis Persists 10-20 min: if defecation does not occur, new set of mass movements might not recur for another half day or day Moves material through the transverse distal colon and into rectum. If you feel the time for defecation is no appropriate, then you can inhibit the defecation reflex. The longer you inhibit the defecation reflex, the weaker the mass movements become. B. Skipped slide 48 C. Defecation Reflexes Mass movement forces feces into rectum, initiated desire to defecate Includes reflex contraction of the rectum and relaxation of the internal (involuntary) and external (voluntary) anal sphincters Intrinsic defecation reflex – weak, internal anal sphincter Parasympathetic defecation reflex-forceful contraction via pelvic nerves -there is also conscious control over the external anal sphincter skeletal muscle. If you relax the external sphincter and have contractions of the smooth muscle in the sigmoid colon, rectum = defecation. D. Bacterial Action in Colon Numerous bacteria, especially colon bacilli Most bacteria killed by lysozyme, defensins, HCl, proteases in colon Substances formed by bacteria: – vitamin K (important for blood coagulation) GI 2 #4 2/23 11am Gwirtz Margaret Veach for Robert Abbate Page 6 of 11 – vitamin B complex – thiamin – riboflavin – various acids & gases by fermenting indigestible CHOs (dimethyl sulfide, H2, N2, CH4, CO2) dimethyl sulfide give feces that “smell” E. Composition of Feces Water 95% Solid matter: of the remaining 5% – Dead bacteria 30% – Fat 10-20% – Inorganic matter 10-20% – Protein 2-3% – Undigested fiber – Bile Pigments – Sloughed epithelial cells Color due to stercobilin and urobilin Odor due to indole, skatole, mercaptans and hydrogen sulfide Slide 52: Get some digestion in the mouth, stomach, but most is in the small intestine. That’s all she said about this slide. Slide 53: Digestion of Carbs. This slide is good, for those of you who like to look at pathways. Digestion begins in the mouth via salivary amylase to break down starch to oligosaccharides. Small intestine: pancreatic amylase ---breaks starch into oligosaccharides Small intestine: Intestinal (brush border) enzymes: dextrinase and glucoamylase ---breaks starch into oligosaccharides Small intestine: Intestinal (brush border) enzymes: lactase, maltase and sucrase: Lactose glucose and galactome Maltose glucose Sucrose glucose and fructose Slide 54: CHO digestion and Absorption in the Small Intestine Glucose and Galactose must be bound to a carrier before they can be absorbed. Fructose is absorbed via facilitated diffusion (there is a carrier, but doesn’t require energy for absorption) she said that was important Again, starch is digested by the amylase; sucrose and lactose are absorbed by brush-border enzymes. So, if you have pancreatic dz, and you lack the α-amylase (can’t absorb starch), you still can absorb some nutrients via the brush-border enzyme. But if you lack the brush-border enzymes, then you can have some serious problems. Slide 55: Digestion of Proteins GI 2 #4 2/23 11am Gwirtz Margaret Veach for Robert Abbate Page 7 of 11 Protein digestion begins in the stomach via pepsin, which breaks proteins into large polypeptides. Small intestine: Pancreatic enzymes: trypsin, chymotrypsin, carboxypeptidase---break down large polypeptides into small polypeptides and small peptides. Small intestine: Intestinal (brush border) enzymes: aminopeptidase, carboxypeptidase, and dipeptidase---breaks the small polypeptides and small peptides into amino acids and dipeptides and tripeptides. Slide 56: The first layer is the intestinal lumen, where digestion is occurring. The brush border has various transporters which will transport the amino acids from the lumen of the stomach into the epithelial cell. Amino acids are mainly absorbed by a Na-cotransport mechanism. Need Na! In the epithelial cell, there are intracellular peptidases which break the dipeptides and tripeptides into amino acids. *Amino acids are the only thing absorbs into the capillary! Slide 57: Proteases and Peptidases in the Small Intestine Skipped Slide 58:Absorption of Di- and Tripeptides Across Brush Border skipped slide 59: Lipid Digestion Have minor lipid digestion in the mouth with lipase. Most of the digestion occurs in the small intestine. In the stomach: there is some emulsification of lipids, from mixing contractions and stomach acid. Small intestine: fats are emulsified by detergent actions of bile salts from the liver, now we have micelles formed. Small intestine: pancreatic lipase—breaks the fats into monoglycerides and fatty acids and glycerol and fatty acids; and can break the cholesterol esters down into cholesterol. Slide 60 In the lumen of the small intestine, we have fat surrounded by bile salts. The micelles transport and release the lipids to the epithelial cell. Slide 61: Inside the Epithelial Cell Once inside the epithelial cell: have reconstitution of free fatty acids to triglycerides, phospholipids, and form cholesterol from cholesterol esters. Add a lipoprotein coat to form a chylomicron, which is a big lipid droplet. It exits the cell via exocystosis. It’s too big to go to a blood capillary, so it goes into a central lacteal. VII. Overall Fluid Balance in GI Tract Gastrin- from the G cells in the antrum, stimulates gastrin receptors in the parietal cells, most GI 2 #4 2/23 11am Gwirtz Margaret Veach for Robert Abbate Page 8 of 11 import function is acid secretion from the parietal cells, increases gastric and intestinal motility, increases pancreatic enzyme secretions. The trophic hormones that promote growth of GI mucosa, the turnover of the cells. What regs gastrin secretion? Distention of the stomach, various enterogastrons. Histamine is a paracrine agent that stimulates H2 receptors. There are mast cells that lie outside of the parietal cells. Vagal stimulation, acid, and gastrin will stimulate the release of histamine. Histamine will then have a large load of material and water that will be digested and absorbed. We injest about 2 L of water a day. 1500mL/day of Saliva 2000mL/day of Gastric secretions 500mL.day of Bile secretion 1500mL/day—Pancreatic Juices secretion Small intestine absorbs-8500mL/day 1500mL/day---intestinal secretions Colon absorbs: 400mL/day ONLY EXCRETING 100 mL/day of water Remember, most of the water is reabsorbed in the small intestine via osmotic gradient by absorption of CHO, lipids, proteins, electrolytes. Slide 63: Na is a co-transport for bile salts in terminal ileum, and glucose, galactose, amino acids in the jejunum. VIII. Water Absorption in the Small Intestine GI 2 #4 2/23 11am Gwirtz Margaret Veach for Robert Abbate Page 9 of 11 Diffusion, mainly through pores between the epithelial cells – 85-95% absorbed in upper small intestine Follows osmotic gradient created by absorption of nutrients and electrolytes Exception: entry of hyperosmotic chyme from stomach into duodenum results in osmosis of water into the intestinal lumen. This leads to secretion of water 1-3 liters ingested, 7-10 liters secreted by gut, but only 150-200 ml excreted in feces IX. Absorption of Sodium Ions 25-35 g daily; 95% absorbed Several mechanisms at luminal membrane – diffusion through Na+ channel – coupled Na+-Cl– co-transport – Na+-H+ co-transport – Na+-solute co-transport (glucose, galactose, amino acids, bile salts) Active transport through basolateral membrane into intercellular spaces systemic venous blood X. Absorption of Chloride Ions Follows electrochemical gradient created by absorption of Na+ systemic venous blood Exception: Active absorption in distal ileum and large intestine in exchange for HCO3- ions (for buffering acidic products formed by bacteria) XI. Absorption of Bicarbonate Absorbed in jejunum with Na+ ; rapid Exception: Active secretion in distal ileum and large intestine in exchange for Cl- ions XII. Absorption of Ions Potassium – passive, through tight junctions and lateral spaces Calcium (1 gram intake daily) – active – about 40% is absorbed relative to body’s need – modulated by parathyroid hormone and a metabolite of vitamin D (1,25dihydroxycholcalceferol) Slide 70: this is another good pathway slide GI 2 #4 2/23 11am Gwirtz Margaret Veach for Robert Abbate Page 10 of 11 Have a decr. Plasma Ca—so there is a need for Ca This triggers incr. in Parathyroid release. Parathyroid hormone converts 25-hydroxyvitamine D3 1,25-dihydroxyvitamin D3 1,25-dihydroxyvitamin D3—stimulates synthesis of Ca-binding protein and Ca2+ATPase in the enterocyte (epithelial cell) -Ca will then enter the cell and if the Ca-binding protein in the blood is empty, then the Ca will be absorbed in the blood stream. -If the Ca-binding proteins are all full, then the Ca will sit in the cell, bound to another protein. The epithelial cell will be sloughed off, and the Ca will be eliminated in the feces. Iron – 10-20 mg daily intake; 10% absorbed – active – absorbed relative to body’s need – ferric (Fe+++) reduced to ferrous (Fe++) by vit C – duod & jej 2 Sources of Iron: Heme iron from eating meat and the ferrous iron. The Heme Iron is them converted to the ferrous iron. In the epi cell in the small intestine, there is a iron-binding protein: Apoferrin. Apoferrin converts the iron to ferritin. In the bloodstream there is a protein transferrin, if there is no iron bound to that transferrin, then the transport protein takes the ferritin from the epithelial cell to bloodstream. If all the transferrin, are bound to ferritin, then the ferritin stays in the cell and is sloughed off with the cell. Ca and Iron are both actively absorption according to the body’s needs. XIII. Vitamin Absorption C, B1, B2, niacin, B6, biotin, folic acid, B12 Water soluble vitamins – Vitamin B12 requires intrinsic factor; terminal ileum Fat soluble vitamins A, D, E, K – along with lipids, absorbed as part of the chylomicron Slide 73: skipped this slide. It shows how B12 is absorbed XIV. Absorption in Large Intestine 1500 ml enter colon, most of water and electrolyes absorbed, 50-200 ml fluid excreted in feces Proximal colon: active absorption of Na+, Cl (via electrochemical gradient), and water (via osmosis) Distal colon: active secretion of HCO3 in exchange for Cl (buffers acid) XV. Summary of Major Sites of Nutrient Absorption GI 2 #4 2/23 11am Gwirtz Margaret Veach for Robert Abbate Page 11 of 11 A. Carbohydrates, proteins, and lipids - mostly absorbed in the duodenum and jejunum B. Calcium, Iron and Folate - mostly absorbed at the upper duodenum. - Ca is also absorbed at the mid-duodenum and jejunum C. Bile Acid - major site of abs is terminal ileum D. Cobalamin (B12) - major site of abs is terminal ileum -This info is impt for patients who need parts of their small intestine removed. Need to know what nutrient absorption will be affected.