RPKPS SPESIALIT HN - Fakultas Farmasi Unand
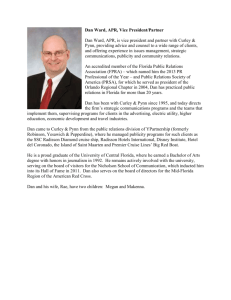
advertisement

RENCANA PROGRAM DAN KEGIATAN PEMBELAJARAN SEMESTER MATA KULIAH SPESIALIT DAN ALKES Oleh Hansen Nasif, S.Si., Apt., Sp.FRS Najmiatul Fitria, M.Farm, Apt. FAKULTAS FARMASI UNIVERSITAS ANDALAS 2014 A. PERENCANAAN PEMBELAJARAN 1. Nama Mata Kuliah : Spesialit dan Alkes 2. Kode Mata kuliah : FAR 363 3. SKS :2 4. Sifat : Wajib 5. Prasyarat : Farmakologi 6. Semester :V 7. Perkiraan banyaknya peserta : 120 mhs 8. Deskripsi singkat mata kuliah Spesialit dan Alkes : Mata Kuliah ini merupakan mata kuliah yang diberikan setelah mahasiswa mendalami farmakologi dengan baik. Pada Spesialit dan Alkes diberikan materi pokok pengenalan dan penggunaan rasional obat-obatan bebas, bebas terbatas, dan obat wajib apotik serta pengenalan dan penggunaan alat kesehatan baik yang habis pakai maupun yang tidak habis pakai. 9. Tujuan Pembelajaran: Tujuan pembelajaran Spesialit dan Alkes adalah mahasiswa memahami dan menguasai Setelah menyelesaikan kuliah ini, diharapkan mahasiswa penggunaan rasional obat obat bebas, bebas terbatas dan obat wajib apotik serta penggunaan alat kesehatan agar nantinya mampu melakukan tugas sebagai seorang farmasis. 10. Tujuan Pembelajaran khusus Setelah mengikuti perkuliahan ini, mahasiswa diharapkan dapat : 1. Mengetahui dan memahami penggunaan rasional obat – obat yang tidak diresepkan. 2. Memahami macam-macam jenis dan penggunaan alat kesehatan B. PELAKSANAAN PEMBELAJARAN Minggu ke (1) Topik (Pokok Bahasan) (2) Pendahuluan dan ruang lingkup Spesialit dan alkes 1 Substansi Materi Penggunaan antasida pada tukak peptik 2 3 Penggunaan DMP, (3) Batasan Spesialit dan Alkes Ruang lingkup Spesialit dan alkes Perkembangan spesialit dan alkes Konsep obat rasional pada obat bebas, bebas terbatas dan wajib apotik. Manfaat ilmu Spesialit dan alkes Antasida dan sediaanya Keadaan tukak peptik Keluhan yang biasanya terjadi Penggolongan antasida Pilihan penggunaan antasida Keadaan yang membatasi penggunaan antasida Keamanan penggunaan antasida Obat batuk dan sediaanya Metode Pembelajaran (4) Ceramah, Tanya jawab Fasilitas (5) Laptop, LCD viewer Persentasi, diskusi Laptop, LCD viewer Persentasi, Laptop, Ket (6) GG dan Bromhexine sebagai antitusive dan ekspektoran pada batuk Penggunaan oralit dan atapulgit pada diare 4 Penggunaan Bisakodil, dan laktulosa pada konstipasi 5 Penggunaan theophilin pada asma 6 Penggunaan Chlorpheniramin dan Brompheniramina ntihistamin pada alergi 7 8 Penggunaan Etinilestradiol Keadaan batuk dan jenisnya Keluhan yang biasanya terjadi Penggolongan obat batuk Profil DMP, GG, Bromhexine Pilihan penggunaan antitusive dan ekspektoran Keamanan penggunaan antitusive dan ekspektoran Oralit, atapulgit dan sediaanya Keadaan diare Keluhan yang biasanya terjadi Profil Oralit dan Attapulgit Pilihan penggunaan oralit dan atapulgit Keadaan yang membatasi penggunaan oralit dan atapulgit Keamanan penggunaan oralit dan atapulgit Obat konstipasi dan sediaanya Keadaan konstipasi Keluhan yang biasanya terjadi Penggolongan obat konstipasi Profil Bisakodil dan Laktulosa. Pilihan penggunaan obat konstipasi Keadaan yang membatasi penggunaan obat konstipasi Keamanan penggunaan obat konstipasi Theophilin dan sediaanya Keadaan Asma Keluhan yang biasanya terjadi Penggolongan obat asma Profil Theophilin Pilihan penggunaan theophilin Keadaan yang membatasi penggunaan theophilin Keamanan penggunaan theophilin Antihistamin dan sediaanya Keadaan alergi Keluhan yang biasanya terjadi Penggolongan antihistamin Profil Chlorpheniramin dan Brompheniramin Pilihan penggunaan Chlorpheniramin dan Brompheniramin Keadaan yang membatasi penggunaan Chlorpheniramin dan Brompheniramin Keamanan penggunaan Chlorpheniramin dan Brompheniramin Kontrasepsi oral dan sediaanya Penggolongan kontrasepsi oral diskusi LCD viewer Persentasi, diskusi Laptop, LCD viewer Persentasi, diskusi Laptop, LCD viewer Persentasi, diskusi Laptop, LCD viewer Persentasi, diskusi Laptop, LCD viewer Persentasi, diskusi Laptop, LCD dan progestin sebagai kontrasepsi oral Penggunaan Preparat sebagai antianemia besi 9 Penggunaan alat kesehatan habis pakai. 10 Penggunaan alat kesehatan tidak habis pakai 11 Peralatan infus dan penggunaanya. 12 13 Peralatan operasi, ortopaedi dan penggunaanya Profil Etinilestradiol dan progestin Pilihan penggunaan Etinilestradiol dan progestin Keadaan yang membatasi penggunaan Etinilestradiol dan progestin Keamanan penggunaan Etinilestradiol dan progestin Antianemia dan sediaanya Keadaan anemia Keluhan yang biasanya terjadi Penggolongan antianemia Profil Fe Pilihan penggunaan Fe sebagai antianemia Keadaan yang membatasi penggunaan Fe sebagai antianemia Keamanan penggunaan Fe Pembagian alat kesehatan Penggunaaan alat kesehatan habis pakai Peran alat kesehatan habis pakai dalam diagnosa Macam” Spiut dan iv kateter, mask dan nebulizer Pilihan penggunaan dan permasalahannya Keamanan penggunaan spuit dan iv keteter Macam-macam alat kesehatan tidak habis pakai Peran alat kesehatan habis pakai dalam diagnosa Macam” alat kesehatan habis pakai dari linen maupun bahan lainnya Pilihan penggunaan dan permasalahannya Keamanan penggunaanya Macam –macam peralatan infus, infus set dan pompa infus. Peran peralatan infus dalam suatu terapi Pilihan penggunaan dan permasaalahannya. Keamanan penggunaan peralatan infus Macam-macam peralatan pisau operasi, alat ortopaedi untuk operasi dan sesudah operasi Pilihan penggunaan macammacam peralatan operasi. Keamanan penggunaan peralatan operasi viewer Persentasi, diskusi Laptop, LCD viewer Persentasi, diskusi Laptop, LCD viewer Persentasi, diskusi Laptop, LCD viewer Persentasi, diskusi Laptop, LCD viewer Persentasi, diskusi Laptop, LCD viewer 14 Peralatan radiodiagnostik dan penggunaannya 15 Peralatan kesehatan lainnya Macam-macam peralatan Rontgen, USG, Endoskopi untuk radiodiagnostik Pilihan penggunaan macammacam peralatan peralatan radiodiagnostik Keamanan penggunaan peralatan radiodiagnostik Persentasi, diskusi Laptop, LCD viewer Macam” benang bedah dan kegunaannya Alat kesehatan lainnya penyimpanan alat kesehatan di gudang farmasi Persentasi, diskusi Laptop, LCD viewer 2. Metode pembelajaran dan bentuk kegiatan Perkuliahan diberikan dalam bentuk penjelasan oleh dosen di depan kelas dengan berbagai alat bantu seperti LCD viewer, Laptop, dan white board. Selain itu juga diterapkan casebased learning di mana dipresentasikan berbagai contoh kasus untuk dibahas di dalam kelas. C. PERENCANAAN EVALUASI PEMBELAJARAN 1. Hasil pembelajaran Kriteria penilaian mengacu pada beberapa kriteria berikut ini : - mahasiswa dapat memahami prinsip-prinsip dalam materi perkuliahan Spesialit dan Alkes, Serta menjelaskan kembali materi perkuliahan tersebut, - Kemampuan mahasiswa menganalisis dan mempresentasikan kasusnya di depan kelas Penilaian tersebut akan dilakukan melalui ujian tertulis dan aktivitas diskusi. Ujian tertulis dilakukan pada akhir semester. Adapun prosentase unsur penilaian dan kriterianya adalah sbb: Unsur - unsur Tugas Quiz Ujian tengah Semester Ujian Semester Total Persentase ( %) 15 15 20 50 100 - Kriteria penilaian untuk mata kuliah ini sesuai dengan yang berlaku pada universitas andalas yaitu dari yang terendah nilai E sampai yang tertinggi nilai A+ 2. Evalusi Proses pembelajaran dari mahasiswa Untuk mendapatkan masukan dari mahasiwa mengenai keseluruhan proses pembelajaran, akan dibagikan kuesioner yang berupa SKALA KEPUASAN MENGAJAR. D. DAFTAR PUSTAKA 1) AHFS Drugs Informations 2008 2) BNF, 57 editions, 2009 3) USPDI, Drugs Information for health care proffesionals, in Harisson Principles of Internal Medicines, 15 th edition CD-ROM, Micromedex, ( www. Harissononline.com) 4) Dipiro, JT, et all, Pharmacotherapy : a pathophisiologic approach, 7 th ed,McGrawHill Company, USA 2008 5) MIMS terbaru KONTRAK PERKULIAHAN Nama Mata Kuliah Kode Mata kuliah Pengajar SKS Semester Hari Pertemuan/Jam Ruang Kuliah : Spesialit dan Alkes : FAR 363 : Hansen Nasif, S.Si., Apt., Sp.FRS Najmiatul Fitria, M.Farm, Apt :2 : VII : Kamis/ 08.00-09.40 WIB : Lokal C 1.Manfaat Mata Kuliah Mata kuliah ini diberikan pada mahasiswa agar dapat memahami dan menguasai penggunaan rasional obat obat bebas, bebas terbatas dan obat wajib apotik serta penggunaan alat kesehatan agar nantinya mampu melakukan tugas sebagai seorang farmasis. 2. Deskripsi Perkuliahan Mata Kuliah ini merupakan mata kuliah yang diberikan setelah mahasiswa mendalami farmakologi dengan baik. Pada Spesialit dan Alkes diberikan materi pokok pengenalan dan penggunaan rasional obat-obatan bebas, bebas terbatas, dan obat wajib apotik serta pengenalan dan penggunaan alat kesehatan baik yang habis pakai maupun yang tidak habis pakai. 3. Tujuan Instruksional Setelah mengikuti perkuliahan ini, mahasiswa diharapkan dapat Mengetahui dan memahami penggunaan rasional obat – obat yang tidak diresepkan dan Memahami macam-macam jenis dan penggunaan alat kesehatan 4. Organisasi Materi Organisasi materi dapat dilihat pada jadwal perkuliahan 5. Strategi Perkuliahan Strategi Instruksional yang digunakan pada mata kuliah ini terdiri dari : a. Urutan kegiatan instruksional berupa : Pendahuluan (TIU dan TIK, cakupan materi pokok bahasan, dan relevansi ), penyajian ( uraian,contoh, diskusi , evaluasi ) dan penutup ( umpan balik, ringkasan materi, petunjuk tindak lanjut, pemberian tugas di rumah, gambaran singkat tetang materi berikutnya ) b. Metode Instruksional menggunakan : metode ceramah, demonstrasi, tanya-jawab, diskusi kasus dan penugasan 1. Ceramah berupa penyampaian bahan ajar oleh dosen pengajar dan penekanan-penekanan pada hal-hal yang penting dan bermanfaat untuk diterapkan 2. Tanya jawab dilakukan sepanjang tatap muka dengan memberikan kesempatan mahasiswa untuk memberikan pendapat atau pertanyaan tentang hal-hal yang tidak mereka mengerti atau bertentangan dengan yang mereka pahami sebelumnya. 3. Diskusi kasus dilakukan dengan memberikan contoh kasus/kondisi pada akhir pokok bahasan, mengambil tema yang sedang aktual di masyarakat dan mengajak mahasiswa menganalisisnya 4. Penugasan diberikan untuk membantu mahasiswa memahami bahan ajar, membuka wawasan, dan memberikan pendalaman materi c. Media Instruksionalnya berupa LCD Projector, Laptop, spidol, Whiteboard,artikel ilmiah di surat kabar/ internet, jurnal ilmiah, handout, dan kontrak perkuliahan. D Waktu : 5 menit pada tahap pendahuluan, 40 menit pada tahap penyajian, dan 5 menit pada tahap penutup. 6. Materi/ Bacaan Perkuliahan 1. AHFS Drugs Informations 2008 2. BNF, 57 editions, 2009 3. USPDI, Drugs Information for health care proffesionals, in Harisson Principles of Internal Medicines, 15 th edition CD-ROM, Micromedex, ( www. Harissononline.com) 4. Dipiro, JT, et all, Pharmacotherapy : a pathophisiologic approach, 7 th ed,McGrawHill Company, USA 2008 5. MIMS terbaru 7. Tugas Dalam perkuliahan, diberikan beberapa tugas sebagai berikut : 1. Materi perkuliahan sebagaimana disebutkan dalam jadwal perkuliahan harus sudah dibaca sebelum mengikutitatap muka. Apabila ada, handout sudah akan diserahkan pada mahasiswa sbelum hari kuloiah 2. Evaluasi mahasiswa dilakukan dengan mengadakan quis dengan waktu yang tidak ditentukan, ujian mid semester dan ujian semester dengan format soal essay 3. Penugasan, jika ada yang sesuai dengan pokok bahasan harus sudah diselesaikan sebelum ujian semester dimulai 8. Kriteria Penilaian Nilai Akhir Nilai Mutu Angka Mutu Sebutan Mutu Sangat cemerlang ≥85-100 A 4,00 ≥80<85 A- 3,50 Cemerlang ≥75<80 B+ 3,25 Sangat baik ≥70<75 B 3,00 Baik ≥65<70 B- 2,75 Hampir baik ≥60<65 C+ 2,25 Lebih dari cukup ≥55<60 C 2,00 Cukup ≥50<55 C- 1,75 Hampir cukup ≥40<50 D 1,00 Kurang <40 E 0,00 Gagal 1. Pembobotan nilai adalah sebagai berikut : Unsur - unsur Tugas Quiz Ujian tengah Semester Ujian Semester Total Persentase ( %) 15 15 20 50 100 2. Bagi mahasiswa yang sudah pernah mengikuti mata kuliah ini sebelumnya namun mengambil mata kuliah ini selanjutnya harus mengikuti perkuliahan ini seluruhnya 3. Untuk memacu kreativitas mahasiswa dan mendapatkan update dalam keilmuan ini maka semua quiz dan ujian pada mata kuliah ini, adalah open book dan dibolehkan melakukan koneksi internet. BAHAN AJAR Dyspepsia Dyspepsia covers pain, fullness, early satiety, bloating, and nausea. It can occur with gastric and duodenal ulceration and gastric cancer but most commonly it is of uncertain origin. Urgent endoscopic investigation is required if dyspepsia is accompanied by ‘alarm features’ (e.g. bleeding, dysphagia, recurrent vomiting, or weight loss). Urgent investigation should also be considered for patients over 55 years with unexplained dyspepsia that has not responded to treatment. Patients with dyspepsia should be advised about lifestyle changes (see Gastro-oesophageal reflux disease, below). Some medications may cause dyspepsia—these should be stopped, if possible. Antacids may provide some symptomatic relief. Histamine H -receptor antagonists heal gastric and duodenal ulcers by reducing gastric acid output as a result of histamine H -receptor blockade; they are also used to relieve symptoms of gastro-oesophageal reflux disease. H -receptor antagonists should not normally be used for Zollinger-Ellison syndrome because proton pump inhibitors are more effective. Maintenance treatment with low doses for the prevention of peptic ulcer disease has largely been replaced in Helicobacter pylori positive patients by eradication regimens H -receptor antagonists are used for the treatment of functional dyspepsia . Treatment of uninvestigated dyspepsia with H -receptor antagonists used regularly or on an intermittent basis, may be acceptable in younger patients but care is required in older people because of the possibility of gastric cancer in these patients. H -receptor antagonist therapy can promote healing of NSAID-associated ulcers (particularly duodenal) Treatment with a H -receptor antagonist has not been shown to be beneficial in haematemesis and melaena, but prophylactic use reduces the frequency of bleeding from gastroduodenal erosions in hepatic coma, and possibly in other conditions requiring intensive care. H - receptor antagonists also reduce the risk of acid aspiration in obstetric patients at delivery Antacids (usually containing aluminium or magnesium compounds) can often relieve symptoms in ulcer dyspepsia and in non-erosive gastro-oesophageal reflux; they are also sometimes used in functional (non-ulcer) dyspepsia but the evidence of benefit is uncertain. Antacids are best given when symptoms occur or are expected, usually between meals and at bedtime, 4 or more times daily; additional doses may be required up to once an hour. Conventional doses e.g. 10 mL 3 or 4 times daily of liquid magnesium– aluminium antacids promote ulcer healing, but less well than antisecretory drugs ; proof of a relationship between healing and neutralising capacity is lacking. Liquid preparations are more effective than tablet preparations. Aluminium- and magnesium-containing antacids (e.g. aluminium hydroxide, and magnesium carbonate, hydroxide and trisilicate), being relatively insoluble in water, are long-acting if retained in the stomach. They are suitable for most antacid purposes. Magnesiumcontaining antacids tend to be laxative whereas aluminium- containing antacids may be constipating; antacids containing both magnesium and aluminium may reduce these colonic side-effects. Aluminium accumulation does not appear to be a risk if renal function is normal The acid-neutralising capacity of preparations that contain more than one antacid may be the same as simpler preparations. Complexes such as hydrotalcite confer no special advantage. Sodium bicarbonate should no longer be prescribed alone for the relief of dyspepsia but it is present as an ingredient in many indigestion remedies. However, it retains a place in the management of urinary-tract disorders and acidosis . Sodium bicarbonate should be avoided in patients on salt-restricted diets. Simeticone (activated dimeticone) is added to an antacid as an antifoaming agent to relieve flatulence. These preparations may be useful for the relief of hiccup in palliative care. Alginates, added as protectants, may be useful in gastro-oesophageal reflux disease . The amount of additional ingredient or antacid in individual preparations varies widely, as does their sodium content, so that preparations may not be freely interchangeable. See also section 1.3 for drugs used in the treatment of peptic ulceration. Interactions Antacids should preferably not be taken at the same time as other drugs since they may impair absorption. Antacids may also damage enteric coatings designed to prevent dissolution in the stomach ALUMINIUM HYDROXIDE Indications dyspepsia; hyperphosphataemia , Cautions see notes above; renal impairment Contra-indications hypophosphataemia; neonates and infants Aluminium-only preparations Aluminium Hydroxide (Non-proprietary) Tablets, dried aluminium hydroxide 500 mg. Net price 20 = 28p Dose 1–2 tablets chewed 4 times daily and at bedtime or as required Alu-Capc (3M) Capsules, green/red, dried aluminium hydroxide 475 mg (low Na+). Net price 120-cap pack = £3.75 Dose antacid, 1 capsule 4 times daily and at bedtime; CHILD not recommended for antacid therapy Co-magaldrox Co-magaldrox is a mixture of aluminium hydroxide and magnesium hydroxide; the proportions are expressed in the form x/y where x and y are the strengths in milligrams per unit dose of magnesium hydroxide and aluminium hydroxide respectively Maaloxc (Sanofi-Aventis) Suspension, sugar-free, co-magaldrox 195/220 (magnesium hydroxide 195 mg, dried aluminium hydroxide 220 mg/5 mL (low Na+)). Net price 500 mL Dose ADULT and CHILD over 14 years, 10–20 mL 20–60 minutes after meals and at bedtime or when required CIMETIDINE Indications benign gastric and duodenal ulceration, stomal ulcer, reflux oesophagitis, Zollinger–Ellison syndrome, other conditions where gastric acid reduction is beneficial (see notes above and section Cautions see notes above; also hepatic impairment ;Side-effects see notes above; also alopecia; very rarely tachycardia, interstitial nephritis Dose 400 mg twice daily (with breakfast and at night) or 800 mg at night (benign gastric and duodenal ulceration) for at least 4 weeks (6 weeks in gastric ulceration, 8 weeks in NSAID-associated ulceration); when necessary the dose may be increased to 400 mg 4 times daily; INFANT under 1 year 20 mg/kg daily in divided doses has been used; CHILD 1–12 years, 25– 30 mg/kg daily in divided doses; max. 400 mg 4 times daily Maintenance, 400 mg at night or 400 mg morning and night . Reflux oesophagitis, 400 mg 4 times daily for 4–8 weeks . Zollinger–Ellison syndrome (but see notes above), 400 mg 4 times daily or occasionally more (max. 2.4 g daily) . Prophylaxis of stress ulceration, 200–400 mg every 4– 6 hours . Gastric acid reduction (prophylaxis of acid aspiration; do not use syrup), obstetrics 400 mg at start of labour, then up to 400 mg every 4 hours if required (max. 2.4 g daily); surgical procedures 400 mg 90–120 minutes before induction of general anaesthesia . Short-bowel syndrome, 400 mg twice daily (with breakfast and at bedtime) adjusted according to response . To reduce degradation of pancreatic enzyme supplements, 0.8–1.6 g daily in 4 divided doses 1–1½ hours before meals 1Cimetidine (Non-proprietary)A Tablets, cimetidine 200 mg, net price 60-tab pack = £1.48; 400 mg, 60-tab pack = £1.61; 800 mg, 30-tab pack = £1.88 Oral solution, cimetidine 200 mg/5 mL, net price 300 mL = £14.24 Excipients may include propylene glycol (see Excipients, p. 2) 1. Cimetidine can be sold to the public for adults and children over 16 years (provided packs do not contain more than 2 weeks’ supply) for the short-term symptomatic relief of heartburn, dyspepsia, and hyperacidity (max. single dose 200 mg, max. daily dose 800 mg), and for the prophylactic management of nocturnal heartburn (single night-time dose 100 mg) Tagametc (Chemidex)A Tablets, all green, f/c, cimetidine 200 mg, net price 120-tab pack = £19.58; 400 mg, 60-tab pack = £22.62; 800 mg, 30-tab pack = £22.62 Syrup, orange, cimetidine 200 mg/5 mL. Net price 600 mL = £28.49 Adsorbents and bulk-forming drugs The priority in acute diarrhoea, as in gastro-enteritis, is the prevention or reversal of fluid and electrolyte depletion. This is particularly important in infants and in frail and elderly patients. For details of oral rehydration preparations, . Severe depletion of fluid and electrolytes requires immediate admission to hospital and urgent replacement. Antimotility drugs relieve symptoms of acute diarrhoea. They are used in the management of uncomplicated acute diarrhoea in adults; fluid and electrolyte replacement may be necessary in case of dehydration. However, antimotility drugs are not recommended for acute diarrhoea in young children. Antispasmodics are occasionally of value in treating abdominal cramp associated with diarrhoea but they should not be used for primary treatment. Antispasmodics and antiemetics should be avoided in young children with gastro-enteritis because they are rarely effective and have troublesome side-effects. Adsorbents such as kaolin are not recommended for acute diarrhoeas. Bulk-forming drugs, such as ispaghula, methylcellulose, and sterculia (section 1.6.1) are useful in controlling diarrhoea associated with diverticular disease. KAOLIN, LIGHTU Indications diarrhoea but see notes above Cautions interactions: Appendix 1 (kaolin) Kaolin Mixture, BPU (Kaolin Oral Suspension) Oral suspension, light kaolin or light kaolin (natural) 20%, light magnesium carbonate 5%, sodium bicarbonate 5% in a suitable vehicle with a peppermint flavour. Dose 10–20 mL every 4 hours Laxatives Before prescribing laxatives it is important to be sure that the patient is constipated and that the constipation is not secondary to an underlying undiagnosed complaint. It is also important for those who complain of constipation to understand that bowel habit can vary considerably in frequency without doing harm. Some people tend to consider themselves constipated if they do not have a bowel movement each day. A useful definition of constipation is the passage of hard stools less frequently than the patient’s own normal pattern and this can be explained to the patient. Misconceptions about bowel habits have led to excessive laxative use. Abuse may lead to hypokalaemia. Thus, laxatives should generally be avoided except where straining will exacerbate a condition (such as angina) or increase the risk of rectal bleeding as in haemorrhoids. Laxatives are also of value in druginduced constipation, for the expulsion of parasites after anthelmintic treatment, and to clear the alimentary tract before surgery and radiological procedures. Prolonged treatment of constipation is sometimes necessary. Children Laxatives should be prescribed by a healthcare professional experienced in the management of constipation in children. Delays of greater than 3 days between stools may increase the likelihood of pain on passing hard stools leading to anal fissure, anal spasm and eventually to a learned response to avoid defaecation. If increased fluid and fibre intake is insufficient, an osmotic laxative containing macrogols or lactulose can be used. If there is evidence of minor faecal retention, the addition of a stimulant laxative may overcome withholding but may lead to colic or, in the presence of faecal impaction in the rectum, an increase of faecal overflow. In children with faecal impaction, an oral preparation containing macrogols is used to clear faecal mass and to establish and maintain soft well-formed stools. Rectal administration of laxatives may be effective but this route is frequently distressing for the child and may lead to persistent withholding. If the impacted mass is not expelled following treatment with macrogols, referral to hospital may be necessary. Enemas may be administered under heavy sedation in hospital or alternatively, a bowel cleansing solution may be tried. In severe cases or where the child is afraid, a manual evacuation under anaesthetic may be appropriate. Long-term regular use of laxatives is essential to maintain well-formed stools and prevent recurrence of faecal impaction; intermittent use may provoke relapses. For children with chronic constipation, it may be necessary to exceed the licensed doses of some laxatives. Parents and carers of children should be advised to adjust the dose of laxative in order to establish a regular pattern of bowel movements in which stools are soft, well-formed, and passed without discomfort. Pregnancy If dietary and lifestyle changes fail to control constipation in pregnancy, moderate doses of poorly absorbed laxatives may be used. A bulk-forming laxative should be tried first. An osmotic laxative, such as lactulose, can also be used. Bisacodyl or senna may be suitable, if a stimulant effect is necessary. The laxatives that follow have been divided into 5 main groups. This simple classification disguises the fact that some laxatives have a complex action. Bulk-forming laxatives Bulk-forming laxatives relieve constipation by increasing faecal mass which stimulates peristalsis; patients should be advised that the full effect may take some days to develop. Bulk-forming laxatives are of particular value in those with small hard stools, but should not be required unless fibre cannot be increased in the diet. A balanced diet, including adequate fluid intake and fibre is of value in preventing constipation. Bulk-forming laxatives are useful in the management of patients with colostomy, ileostomy, haemorrhoids, anal fissure, chronic diarrhoea associated with diverticular disease, irritable bowel syndrome, and as adjuncts in ulcerative colitis . Adequate fluid intake must be maintained to avoid intestinal obstruction. Unprocessed wheat bran, taken with food or fruit juice, is a most effective bulk-forming preparation. Finely ground bran, though more palatable, has poorer waterretaining properties, but can be taken as bran bread or biscuits in appropriately increased quantities. Oat bran is alsoused. Methylcellulose, ispaghula, and sterculia are useful in patients who cannot tolerate bran. Methylcellulose also acts as a faecal softener. BISACODYL Contra-indications see notes above, acute surgical abdominal conditions, acute inflammatory bowel disease, severe dehydration Dose . Constipation, by mouth, 5–10 mg at night; CHILD (but see section 1.6) 4–10 years (on medical advice only) 5 mg at night, over 10 years, adult dose By rectum in suppositories, 10 mg in the morning; CHILD (but see section 1.6) under 10 years (on medical advice only) 5 mg, over 10 years, adult dose . Before radiological procedures and surgery, by mouth, 10–20 mg the night before procedure and by rectum in suppositories, 10 mg the following morning; CHILD 4–10 years by mouth, 5 mg the night before procedure and by rectum in suppositories, 5 mg the following morning; over 10 years, adult dose Note tablets act in 10–12 hours; suppositories act in 20–60 minutes The brand names Dulcolax Liquid and Dulcolax Perles are used for sodium picosulfate preparations The selective beta agonists (selective beta –adrenoceptor agonists, selective beta stimulants) such as salbutamol or terbutaline are the safest and most effective shortacting beta agonists for asthma. Less selective beta agonists such as orciprenaline should be avoided whenever possible. Adrenaline (epinephrine) (which has both alpha- and beta-adrenoceptor agonist properties) is used in the emergency management of allergic and anaphylactic reactions and in the management of croup . Selective beta2 agonists Selective beta agonists produce bronchodilation. A short-acting beta agonist is used for immediate relief of asthma symptoms while a long-acting beta agonist is added to an inhaled corticosteroid in patients requiring prophylactic treatment. Short-acting beta agonists Mild to moderate symptoms of asthma respond rapidly to the inhalation of a selective short-acting beta agonist such as salbutamol or terbutaline. If beta agonist inhalation is needed more often than once daily, prophylactic treatment should be considered, using a stepped approach as outlined in the Management of Chronic Asthma table,. Regular treatment with an inhaled short-acting beta agonist is less effective than ‘as required’ inhalation and is not appropriate prophylactic treatment. A short-acting beta agonist inhaled immediately before exertion reduces exercise-induced asthma; however, frequent exercise-induced asthma probably reflects poor overall control and calls for reassessment of asthma treatment. Long-acting beta agonists Formoterol (eformoterol) and salmeterol are longer-acting beta agonists which are administered by inhalation. Added to regular inhaled corticosteroid treatment, they have a role in the long-term control of chronic asthma and they can be useful in nocturnal asthma. Salmeterol should not be used for the relief of an asthma attack; it has a slower onset of action than salbutamol or terbutaline. Formoterol is licensed for short-term symptom relief and for the prevention of exercise-induced bronchospasm; its speed of onset of action is similar to that of salbutamol. EPHEDRINE HYDROCHLORIDEU Indications reversible airways obstruction, Cautions hyperthyroidism, diabetes mellitus, ischaemic heart disease, hypertension, renal impairment, elderly; prostatic hypertrophy (risk of acute retention); interaction with MAOIs a disadvantage; Side-effects tachycardia, anxiety, restlessness, insomnia common; also tremor, arrhythmias, dry mouth, cold extremities Dose 15–60 mg 3 times daily; CHILD up to 1 year 7.5 mg 3 times daily, 1–5 years 15 mg 3 times daily, 6–12 years 30 mg 3 times daily Theophylline Theophylline is a bronchodilator used for asthma and stable chronic obstructive pulmonary disease; it is not generally effective in exacerbations of chronic obstructivepulmonary disease. It may have an additive effect when used in conjunction with small doses of beta agonists; the combination may increase the risk of side-effects, including hypokalaemia Theophylline is metabolised in the liver; there is considerable variation in plasmatheophylline concentration particularly in smokers, in patients with hepatic impairment or heart failure, or if certain drugs are taken concurrently. The plasma-theophylline concentration is increased in heart failure, cirrhosis, viral infections, in the elderly, and by drugs that inhibit its metabolism. The plasma-theophylline concentration is decreased in smokers and in chronic alcoholism and by drugs that induce liver metabolism. For other interactions of theophylline Differences in the half-life of theophylline are importantbecause its toxic dose is close to the therapeutic dose; particular care is required when introducing or withdrawing drugs that interact with theophylline. In most individuals a plasma-theophylline concentration of between 10–20 mg/litre is required for satisfactory bronchodilation, although a plasma-theophylline concentration of 10 mg/litre (or less) may be effective. Adverse effects can occur within the range 10–20 mg/ litre and both the frequency and severity increase at concentrations above 20 mg/litre. Theophylline is given by injection as aminophylline, a mixture of theophylline with ethylenediamine, which is 20 times more soluble than theophylline alone. Aminophylline injection is needed rarely for severe attacks of asthma. It must be given by very slow intravenous injection (over at least 20 minutes); it is too irritant for intramuscular use. Measurement of plasma theophylline concentration may be helpful, and is essential if aminophylline is to be given to patients who have been taking theophylline, because serious side-effects such as convulsions and arrhythmias can occasionally precede other symptoms of toxicity. THEOPHYLLINE Indications reversible airways obstruction, acute severe asthma; see also Management of Chronic and Acute Asthma Cautions cardiac disease, hypertension, hyperthyroidism; peptic ulcer; epilepsy; elderly; fever; CSM advice on hypokalaemia risk, ; avoid in acute porphyria ; monitor plasma-theophylline concentration (see notes above); hepatic impairment ; pregnancy ; Side-effects tachycardia, palpitation, nausea and other gastro-intestinal disturbances, headache, CNS stimulation, insomnia, arrhythmias, and convulsions especially if given rapidly by intravenous injection; overdosage: see Emergency Treatment of Poisoning, Note Plasma-theophylline concentration for optimum response 10–20 mg/litre (55–110 micromol/litre); 4–6 hours after a dose and at least 5 days after starting treatment; narrow margin between therapeutic and toxic dose, see also notes above Modified release Note The rate of absorption from modified-release preparations can vary between brands. The Council of the Royal Pharmaceutical Society of Great Britain advises pharmacists that if a general practitioner prescribes a modified-release oral theophylline preparation without specifying a brand name, the pharmacist should contact the prescriber and agree the brand to be dispensed. Additionally, it is essential that a patient discharged from hospital should be maintained on the brand on which that patient was stabilised as an in-patient. Slo-Phyllinc (Merck) Capsules, m/r, theophylline 60 mg (white/clear, enclosing white pellets), net price 56-cap pack = £2.76; 125 mg (brown/clear, enclosing white pellets), 56-cap pack = £3.48; 250 mg (blue/clear, enclosing white pellets), 56-cap pack = £4.34. Label: 25, or counselling, see below Dose 250–500 mg every 12 hours; CHILD 2–6 years 60–120 mg every 12 hours, 6–12 years 125–250 mg every 12 hours Counselling Swallow whole with fluid or swallow enclosed granules with soft food (e.g. yoghurt) AMINOPHYLLINE Note Aminophylline is a stable mixture or combination of theophylline and ethylenediamine; the ethylenediamine confers greater solubility in water Indications reversible airways obstruction, acute severe asthma Cautions see under Theophylline Side-effects see under Theophylline; also allergy to ethylenediamine can cause urticaria, erythema, and exfoliative dermatitis Dose See under preparations, below Note Plasma-theophylline concentration for optimum response 10–20 mg/litre (55–110 micromol/litre); measure plasma-theophylline concentration 4–6 hours after dose by mouth and at least 5 days after starting oral treatment; measure plasma-theophylline concentration 4–6 hours after the start of intravenous infusion; narrow margin between therapeutic and toxic dose, see also notes above Antihistamines All antihistamines are of potential value in the treatment of nasal allergies, particularly seasonal allergic rhinitis (hay fever), and they may be of some value in vasomotor rhinitis. They reduce rhinorrhoea and sneezing but are usually less effective for nasal congestion. Antihistamines are used topically in the eye (section 11.4.2), in the nose , and on the skin Oral antihistamines are also of some value in preventing urticaria and are used to treat urticarial rashes, pruritus, and insect bites and stings; they are also used in drug allergies. Injections of chlorphenamine (chlorpheniramine) or promethazine are used as an adjunct to adrenaline (epinephrine) in the emergency treatment of anaphylaxis and angioedema . For the use of antihistamines (including cinnarizine, cyclizine, and promethazine teoclate) in nausea and vomiting, see section 4.6. Buclizine is included as an anti-emetic in a preparation for migraine . For reference to the use of antihistamines for occasional insomnia, All older antihistamines cause sedation but alimemazine (trimeprazine) and promethazine may be more sedating whereas chlorphenamine and cyclizine may be less so. This sedating activity is sometimes used to manage the pruritus associated with some allergies. There is little evidence that any one of the older, ‘sedating’ antihistamines is superior to another and patients vary widely in their response. Non-sedating antihistamines such as cetirizine, desloratadine (an active metabolite of loratadine), fexofenadine (an active metabolite of terfenadine), levocetirizine (an isomer of cetirizine), loratadine, and mizolastine cause less sedation and psychomotor impairment than the older antihistamines because they penetrate the blood brain barrier only to a slight extent. Cautions and contra-indications Sedating antihistamines have significant antimuscarinic activity and they should therefore be used with caution in prostatic hypertrophy, urinary retention, susceptibility to angle-closure glaucoma, and pyloroduodenal obstruction. Antihistamines should be used with caution in hepatic disease Caution may be required in epilepsy. Children and the elderly are more susceptible to sideeffects. Many antihistamines should be avoided in acute porphyria but some are thought to be safe, see section Side-effects Drowsiness is a significant side-effect with most of the older antihistamines although paradoxical stimulation may occur rarely, especially with high doses or in children and the elderly. Drowsiness may diminish after a few days of treatment and is considerably less of a problem with the newer antihistamines . Side-effects that are more common with the older antihistamines include headache, psychomotor impairment, and antimuscarinic effects such as urinary retention, dry mouth, blurred vision, and gastro-intestinal disturbances. Other rare side-effects of antihistamines include hypotension, palpitation, arrhythmias, extrapyramidal effects, dizziness, confusion, depression, sleep disturbances, tremor, convulsions, hypersensitivity reactions (including bronchospasm, angioedema, and anaphylaxis, rashes, and photosensitivity reactions), blood disorders, liver dysfunction, and angle-closure glaucoma. Non-sedating antihistamines Driving Although drowsiness is rare, nevertheless patients should be advised that it can occur and may affect performance of skilled tasks (e.g. driving); excess alcohol should be avoided. CETIRIZINE HYDROCHLORIDE Indications symptomatic relief of allergy such as hay fever, chronic idiopahtic urticaria Cautions see notes above; also renal impairment Contra-indications see notes above; also pregnancy Dose ADULT and CHILD over 6 years, 10 mg once daily or5mg twice daily; CHILD 1–2 years see BNF for Children, 2–6 years, hay fever, 5 mg once daily or 2.5 mg twice daily Cetirizine (Non-proprietary) Tablets, cetirizine hydrochloride 10 mg, net price 30tab pack = 97p. Counselling, driving Dental prescribing on NHS Cetirizine 10 mg tablets may be prescribed Oral solution, cetirizine hydrochloride 5 mg/5 mL, net price 200 mL = £2.43. Counselling, driving Cough suppressants Cough may be a symptom of an underlying disorder, such as asthma , gastro-oesophageal reflux disease, or rhinitis , which should be addressed before prescribing cough suppressants. Cough may be a side-effect of another drug, such as an ACE inhibitor , or it can be associated with smoking or environmental pollutants. Cough can also have a significant habit component. When there is no identifiable cause, cough suppressants may be useful, for example if sleep is disturbed. They may cause sputum retention and this may be harmful in patients with chronic bronchitis and bronchiectasis. Non-opioid analgesics Aspirin is indicated for headache, transient musculoskeletalpain, dysmenorrhoea and pyrexia. In inflammatory conditions, most physicians prefer anti-inflammatory treatment with another NSAID which may be better tolerated and more convenient for the patient. Aspirin is used increasingly for its antiplatelet properties . Aspirin tablets or dispersible aspirin tablets are adequate for most purposes as they act rapidly. Gastric irritation may be a problem; it is minimised by taking the dose after food. Enteric-coated preparations are available, but have a slow onset of action and are therefore unsuitable for single-dose analgesic use(though their prolonged action may be useful for nightpain). Aspirin interacts significantly with a number of other drugs and its interaction with warfarin is a special hazard, see interactions: (aspirin). Paracetamol is similar in efficacy to aspirin, but has no demonstrable anti-inflammatory activity; it is less irritant to the stomach and for that reason is now generally preferred to aspirin, particularly in the elderly. Overdosage with paracetamol is particularly dangerous as it may cause hepatic damage which is sometimes not apparent for 4 to 6 days (see Emergency Treatment of Poisoning, p. 29). Nefopam may have a place in the relief of persistent pain unresponsive to other non-opioid analgesics. It causes little or no respiratory depression, but sympathomimetic and antimuscarinic side-effects may be troublesome. Non-steroidal anti-inflammatory analgesics (NSAIDs, section 10.1.1) are particularly useful for the treatment of patients with chronic disease accompanied by pain and inflammation. Some of them are also used in the short-term treatment of mild to moderate pain including transient musculoskeletal pain but paracetamol is now often preferred, particularly in the elderly . They are also suitable for the relief of pain in dysmenorrhoea and to treat pain caused by secondary bone tumours, many of which produce lysis of bone and release prostaglandins Compound analgesic preparations Compound analgesic preparations that contain a simple analgesic (such as aspirin or paracetamol) with an opioid component reduce the scope for effective titration of the individual components in the management of pain of varying intensity. Compound analgesic preparations containing paracetamol or aspirin with a low dose of an opioid analgesic (e.g. 8 mg of codeine phosphate per compound tablet) are commonly used, but the advantages have not been substantiated. The low dose of the opioid may be enough to cause opioid side-effects (in particular, constipation) and can complicate the treatment of overdosage yet may not provide significant additional relief of pain. A full dose of the opioid component (e.g. 60 mg codeine phosphate) in compound analgesic preparations effectively augments the analgesic activity but is associated with the full range of opioid side-effects (including nausea, vomiting, severe constipation, drowsiness, respiratory depression, and risk of dependence on long-term administration). For details of the side-effects of opioid analgesics, (important: the elderly are particularly susceptible to opioid side-effects and should receive lower doses). In general, when assessing pain, it is necessary to weigh up carefully whether there is a need for a non-opioid and an opioid analgesic to be taken simultaneously. For information on the use of combination analgesic preparations in dental and orofacial pain, Caffeine is a weak stimulant that is often included, insmall doses, in analgesic preparations. It is claimed that the addition of caffeine may enhance the analgesic effect, but the alerting effect, mild habit-forming effect and possible provocation of headache may not always be desirable. Moreover, in excessive dosage or on withdrawal caffeine may itself induce headache. Co-proxamol tablets (dextropropoxyphene in combination with paracetamol) are no longer licensed because of safety concerns, particularly toxicity in overdose. Coproxamol tablets [unlicensed] may still be prescribed for patients who find it difficult to change, because, for example, alternatives are not effective or suitable. ASPIRIN (Acetylsalicylic Acid) Indications mild to moderate pain, pyrexia; antiplatelet Cautions asthma, allergic disease, hepatic impairment , renal impairment, dehydration; preferably avoid during fever or viral infection in children (risk of Reye’s syndrome, see below); pregnancy; elderly; G6PDdeficiency concomitant use of drugs that increase risk of bleeding; Contra-indications children under 16 years and in breast-feeding (Reye’s syndrome, see below; Appendix 5); previous or active peptic ulceration, haemophilia; not for treatment of gout Hypersensitivity Aspirin and other NSAIDs are contraindicated in patients with a history of hypersensitivity to aspirin or any other NSAID—which includes those in whom attacks of asthma, angioedema, urticaria or rhinitis have been precipitated by aspirin or any other NSAID Reye’s syndrome Owing to an association with Reye’s syndrome, the CSM has advised that aspirin-containing preparations should not be given to children under 16 years, unless specifically indicated, e.g. for Kawasaki syndrome Side-effects generally mild and infrequent but high incidence of gastro-intestinal irritation with slight asymptomatic blood loss, increased bleeding time, bronchospasm and skin reactions in hypersensitive patients. Prolonged administration, PARACETAMOL (Acetaminophen) Indications mild to moderate pain, pyrexia Cautions hepatic impairment ; renal impairment , alcohol dependence; Side-effects side-effects rare, but rashes, blood disorders (including thrombocytopenia, leucopenia, neutropenia) reported; hypotension also reported on infusion; important: liver damage (and less frequently renal damage) SILABUS MATA KULIAH FAR 363 Spesialit & Alat Kesehatan Prasyarat : Farmakoogi Mata Kuliah ini merupakan mata kuliah yang diberikan setelah mahasiswa mendalami farmakologi dengan baik. Pada Spesialit dan Alkes diberikan materi pokok pengenalan dan penggunaan rasional obat-obatan bebas, bebas terbatas, dan obat wajib apotik serta pengenalan dan penggunaan alat kesehatan baik yang habis pakai maupun yang tidak habis pakai. Buku Pegangan 6) AHFS Drugs Informations 2008 7) BNF, 57 editions, 2009 8) USPDI, Drugs Information for health care proffesionals, in Harisson Principles of Internal Medicines, 15 th edition CD-ROM, Micromedex, ( www. Harissononline.com) 9) Dipiro, JT, et all, Pharmacotherapy : a pathophisiologic approach, 7 th ed,McGrawHill Company, USA 2008 10) MIMS terbaru SPESIALIT & ALKES Contoh Soal & Jawaban 1.Seorang penderita penderita asma datang meminta informasi kepada saudara yang sedang berasda di apotik tentang aminophilin yang sering dikonsumsinya. Saudara memberikan informasi bahwa theophilin ternyata lebih baik dari ainophilin karena aminophilin anhydrous yang biasa digunakan sebagai obat mengandung ; a. b. c. d. e. 83% theophilin 86% theophilin 74% theophilin 71% theophilin 79% theophilin 2.Efedrin adalah salah satu obat yang dulunya digunakan sebagai obat asma,namunsekarang mulai jarang digunakan lagi karena banyaknya efek samping yang timbul pada penggunaan obat ini. Efek samping efedrin timbul adalah karena kerja obat ini pada reseptor: a. b. Alfa 1, Alfa 2, Beta 1, Beta 2, CNS Alfa 1, Alfa 2, Beta 1, Beta 2 c. d. e. Alfa 1, Alfa 2, Beta 1, CNS Alfa 1, Beta 1, Beta 2, CNS Alfa 2, Beta 1, Beta 2, CNS 3.Antasida adalah obat yang biasa digunakan untuk mengatasi gangguan asam lambung, namun selain itu antasida berguna juga untuk keadaan antihiperfosfatemia ( untuk mengikat kelebihan fosfat) pada gangguan ginjal, antasida yang dipakai adalah : a. b. c. d. e. Magaldrad Magnesium oxide Magnesiun hidroxide Natrium Bicarbonate Calsium Carbonate 4.Seorang pasien penderita konstipasi saudara rekomendasikan untuk menggunakan dulcolax supp untuk mengobati keluhannnya itu, maka saudara harus menerangkan cara penggunaan suppose nya adalah saat : a. b. c. d. e. Berbaring mirring, kaki diangkat Berbaring miring kaki ditekuk Berbaring miring kaki dibuka selebar mungkin Menelungkup dengan pinggul diangkat Jongkok 5.Pendapat saudara jika suatu obat asma dikombinasi dengan bukan obat bronkodilator a. b. c. d. e. Tidak boleh karena tidak bisa dikombinasikan Boleh karena mungkin saja bermanfaat Seharusnya tidak dikombinasikan karena mungkin berbahaya Harus dikombinasi kalau satu obat tdk cukup mengatasi keadaan Semua pendapat diatas salah 6.Penderita diare sering menderita lemah tubuhnya, secara umum ini adalah karena selain kekurangan glukosa juga kekurangan bahan/ senyawa: a. b. c. d. e. Sitrat Natrium Kalium Magnesium Clorida 7.Pemberian suatu obat sering dikaitkan dengan interaksi obat. Kasus yang sering kita jumpai adalah adanya interaksi obat seperti antasida dengan bahan/ senyawa lainnnya. Pada prinsipnya interaksi obat ini kemungkinan bisa terjadi jika pemberian obat yang diberikan bersamaan dengan : a. b. c. d. e. Suatu obat lain Makanan Minuman a dan b benar semua jawaba diatas benar 8.Seorang ibu dengan anak usia 1,5 tahun menderita asma meminta saran saudara tentang theohilin, penyataan yang benar adalah : a. Theohilin tidak boleh digunakan untuk anak ini b. c. d. e. Dosis theophilin untuk anak ini adalah sekitar 260 mg sekali pakai Kalau untuk anak ini mau dipakai sebaiknya bukan theophilin, tapi aminophilin Obat bentuk Inhalasi lebih aman untuk anak ini Sebaiknya gunakan sediaan Sustain Releasenya. 9.Garlic ( Allium sativum ) adalah herbal medicine yang yang diyakini bersifat a. b. c. d. e. Memperbaiki keadaan pada gangguan jantung Antidiabetes antihiperkolesterolemia Neurotonik Antiasmatic 10.Banyaknya kasus konstipasi pada bayi berhubungan dengan beberapa statemen berikut: a. b. c. d. e. Bayi sebaiknya diberikan bisakodil tab saja. Bayi sebaiknya diberi lactulosa Bayi boleh mendapatkan sediaan untuk antikonstipasi yang diberikan via anus Bayi tidak boleh mendapatkan sediaan antikonstipasi via anus Semua penyataan diatas salah. Jawaban : 1. b, 2. c, 3. e, 4. b, 5. b, 6. c, 7.e, 8. b, 9. c, 10. c.