<v1
advertisement

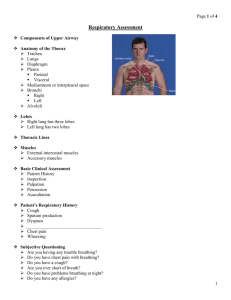
Physical Exam Introduction Physical examination employs the use of inspection, palpation, percussion, and auscultation to determine patients’ clinical status and their response to therapy. Each examination is modified according to the purpose of the examination. Physical examination skills develop over time with practice. Examination of the Head and Neck Head Facial Expression Look for evidence of cyanosis around the lips and oral mucosa. Patients may use pursed-lip breathing when COPD is present. Eyes Pupillary Response Ptosis Neck The trachea should be midline. The status of the jugular veins in the neck is important. Use of accessory muscles Lung Topography Imaginary Lines Anterior chest Lateral chest Posterior chest Thoracic Cage Landmarks The angle of Louis Posterior chest Lung Fissures The oblique fissure The right lung also has a horizontal fissure. Tracheal Bifurcation At T4 on posterior chest At sternal angle on anterior chest Diaphragm The diaphragm is a dome-shaped muscle. The top of the dome rests at about the fifth rib anteriorly and at T9 on the posterior chest normally. Lung Borders On the anterior chest the upper border of the lung extends 2 to 4 cm above the medial third of the clavicles. The inferior border of the lung is at rib six normally. On the lateral chest the lower margin of the lung is at rib eight. On the posterior chest the superior border of the lung extends to T1. The inferior border varies with breathing but is usually at about T10. Examination of the Thorax Inspection The thoracic configuration is determined by inspection. Barrel Chest Kyphoscoliosis Pectus carinatum Pectus excavatum Breathing pattern is important to identify when lung disease is present. Rapid and shallow breathing A prolonged expiratory time Retractions are seen as inward depression of the skin around the rib cage with inspiration Abdominal paradox Hoover’s sign Inspection for cyanosis is done when oxygenation problems are suspected. The lack of cyanosis is not to be interpreted as a sign of adequate oxygenation because anemia could be present. Palpation Vocal fremitus Increased vocal fremitus Decreased vocal fremitus Percussion Percussion Increased resonance Decreased resonance Auscultation of the Lungs Chest auscultation is performed with a stethoscope. The diaphragm portion is used most often for lung auscultation. The technique calls for beginning at the lung bases and comparing side to side. At least one full respiratory cycle should be evaluated at each location. The normal sounds of breathing are called breath sounds. Tracheal breath sounds are heard directly over the trachea. Bronchovesicular breath sounds are heard around the sternum and between the scapulae. The most common breath sound evaluated is the vesicular or normal breath sounds. They are heard over lung parenchyma and are primarily an inspiratory sound. The vesicular breath sound is called diminished when it is barely heard. It is called harsh or bronchial when louder than normal. Abnormal lung sounds superimposed on the breath sounds are termed adventitious lung sounds (ALS). Most ALS can be classified as continuous or discontinuous. Discontinuous ALS are to be called crackles. Continuous ALS are termed wheezes. Stridor is a continuous ALS heard over the neck. The mechanisms responsible for creating normal and abnormal lung sounds are of interest. Normal breath sounds Bronchial breath sounds Diminished or absent breath sounds Crackles Wheezes Stridor Examination of the Precordium The precordium is the surface of the chest wall overlying the heart. It is examined to assess the condition of the heart. Review of Heart Topography The base of the heart (upper portion) lies directly beneath the middle portion of the sternum. The apex points downward and to the left, extending to the midclavicular line near the fifth rib. Inspection and Palpation The precordium is inspected and palpated to determine the position of the point of maximal impulse (PMI) Abnormal heaves are also looked for on the precordium. Right ventricular hypertrophy often causes a heave near the lower left sternal border. Auscultation of Heart Sounds The first heart sound (S1) The second heart sound (S2) A split S1 or S2 occurs when the two sides of the heart are not in sync. S3 and S4 can occur when the left ventricle is distended and as blood rapidly fills the ventricle during diastole. A loud P2 is heard when the pulmonic valve closes with force. Murmurs are heard when heart valves are incompetent, or stenotic, and are produced by rapid blood flow through the narrow valve. Systolic murmurs are heard when the semilunar valves are stenotic or when the A-V valves are incompetent. Diastolic murmurs are heard when the A-V valves are stenotic or when the semilunar valves are incompetent. Neurologic Examination The neurologic exam is done by the physician when brain or spinal cord injury is suspected. RTs need to be familiar with the results of this exam because it has implications for the pulmonary system. Anatomy and Physiology The central nervous system is made up of the brain and spinal cord. The brain stem is the most important part of the CNS regarding breathing. It is where breathing is regulated and controlled. The spinal cord serves the purpose of connecting the brain to the peripheral body parts for sensory and motor function. The peripheral nervous system is made up of 12 cranial nerves and 31 spinal cord nerves. Assessment of the CNS The level of consciousness Coma The Glasgow Coma Scale is often used to document the level of neurologic impairment. The patient’s response to pain is also used to assess the CNS. The patient’s breathing pattern often provides clues about the level of brain stem function. o Cheyne-Stokes breathing o Ataxic breathing Assessment of the Peripheral Nervous System Evaluation of spinal cord function is done by using a variety of motor and sensory tests. For example, the physician may check the patient’s reflexes. Cranial nerve IX Examination of the Abdomen An enlarged liver is known as hepatomegaly. Severe abdominal distension often causes impairment of the diaphragm. Examination of the Extremities Clubbing Although the cause of clubbing is unknown, it is often seen in patients with chronic cardiopulmonary disease. Cyanosis Peripheral cyanosis Pedal Edema Pedal edema The ankles are prone to edema because they are dependent most of the day. Capillary Refill A slow capillary refill is a sign of low cardiac output. Peripheral Skin Temperature Cool extremities are a sign of poor perfusion.