File - Wk 1-2
advertisement

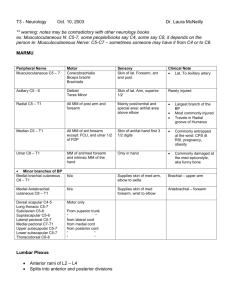
Topographical Anatomy of the Vessels of the Limbs Basic Anatomical Structures & Principles (syllabus) Understand the concepts & associated principles, functional & clinical applications of the topographical anatomy of the vessels of the limbs. UPPER LIMB o ARTERIES Artery Source Branches Supply Additional Info Suprascapular A. thyrocervical trunk Muscular (to supraspinatus and infraspinatus) supraspinatus & infraspinatus, shoulder joint Anastomoses with the circumflex scapular a. and the dorsal scapular a. to form the scapular anastomosis Axillary subclavian (continuation of the subclavian lateral to the 1st rib) 1st part: superior thoracic; 2nd part: thoracoacromial, lateral thoracic; 3rd part: ant. & post. humeral circumflex, subscapular shoulder & upper limb pectoralis minor crosses the axillary artery anteriorly and is used to delineate the 3 parts Subscapular axillary, 3rd part circumflex scapular, thoracodorsal subscapularis, teres major, teres minor, infraspinatus, latissimus dorsi anastomoses with suprascapular, dorsal scapular & deep br. of transverse cervical Anterior circumflex humeral axillary, 3rd part muscular arm muscles neck of humerus Posterior circumflex humeral axillary, 3rd part muscular arm muscles neck of humerus passes through quadrangular space with axillary nerve Brachial axillary (continuation distal to teres major m.) deep brachial, sup. ulnar collateral, nutrient, inf. ulnar collateral; terminal branches are the radial & ulnar arm, forearm & hand normally terminates at the level of the elbow, but high branching may occur Deep brachial brachial ascending br., terminal branches are the middle collateral & radial post. arm collateral Arch, superficial Palmar ulnar a., superficial palmar br. of the radial a. common palmar digital aa. (3) superficial palm, palmar surface of the digits excluding thumb, dorsum of the distal phalangeal segments of digits 2-5 superficial palmar arterial arch receives the majority of its blood supply from the ulnar a. Interosseous, anterior common interosseous a. muscular brs.; a. of the median nerve flexor pollicis longus m., flexor digitorum profundus m., pronator quadratus m., radius, ulna, carpal bones anterior interosseous a. pierces the interosseous membrane at its distal end to reach the dorsal carpal anastomosis Interosseous, common ulnar a. anterior interosseous a., posterior interosseous a. deep structures of the forearm common interosseous a. supplies the deep forearm flexor and deep forearm extensor muscles Interosseous, posterior common interosseous a. interosseous recurrent muscles of the posterior (extensor) forearm compartment: supinator m., abductor pollicis longus m., extensor pollicis longus m., extensor pollicis brevis m., extensor indicis m. posterior interosseous a. passes proximal to the interosseous membrane to reach the extensor compartment of the forearm Radial brachial a. radial recurrent a., palmar carpal br., superficial palmar br., dorsal carpal br., 1st dorsal metacarpal a., princeps pollicis a., radialis indicis a., deep palmar arterial arch posterior elbow, posterior forearm, posterior hand, deep portion of palmar side of the hand, thumb radial a. provides the majority of blood supply to the deep palmar arterial arch; normally it arises at the level of the elbow but high branching of the brachial a. may result in the radial a. arising as proximal as the axilla Ulnar brachial a. anterior ulnar recurrent a., posterior ulnar recurrent a., common interosseous a., palmar carpal br., dorsal carpal br., deep palmar br., superficial palmar arterial arch medial side of the anterior forearm, posterior forearm, superficial palm, fingers ulnar a. supplies the majority of blood to the superficial palmar arterial arch; it normally arises at the level of the elbow, but high branching of the brachial a. may cause the ulnar a. to arise as far proximally as the axilla Arch, deep palmar radial a., deep br. of ulnar a. palmar metacarpal aa. (2nd-4th), perforating brs. deep palm, digits including the dorsum of the distal phalangeal segment deep palmar arterial arch receives the majority of its blood supply from the radial a. Arch, superficial palmar ulnar a., superficial palmar br. of the radial a. common palmar digital aa. (3) superficial palm, palmar surface of the digits excluding thumb, dorsum of the distal phalangeal segments of digits 2-5 superficial palmar arterial arch receives the majority of its blood supply from the ulnar a. Digital, common palmar superficial palmar arterial proper palmar digital aa. (2) palmar aspect two adjacent digits common palmar digital aa. anastomose with palmar arch metacarpal aa. Digital, proper palmar common palmar no named branches digital a. palmar aspect of each digit proper palmar digital aa. supply the dorsum of the distal phalangeal segment and nail bed Princeps pollicis radial a. two brs. to the thumb palmar aspect of the thumb including the dorsum of the distal phalangeal segment arteria princeps pollicis is similar in function to a proper digital aa.; this artery has a large pulse which can be felt when attempting to take the pulse of a patient use fingers to feel for the patient's pulse Radialis indicis radial a. no named branches lateral (radial) side of the index finger Radialis indicis is equivalent to a proper digital a. Recurrent, anterior ulnar ulnar a. unnamed muscular brs. medial side of elbow and anterior ulnar recurrent a. proximal ends of forearm often arises in common with flexor mm. the posterior ulnar recurrent a. Superficial ulnar ulnar a. no named branches palm continues as the superficial palmar arch UPPER LIMB o Vein Cephalic v. VEINS Tributaries lateral side of the dorsal venous arch of the hand; Drains Into axillary vein Regions Drained superficial parts of the lateral hand and Additional Info median cubital vein usually shunts some of the blood superficial veins of the forearm lateral forearm collected by the cephalic v. to the basilic v. unites with brachial vein(s) to form the axillary vein superficial parts of medial hand & medial forearm connects with deep veins of the forearm via perforating veins Median cubital cephalic basilic superficial parts of hand & forearm a median antebrachial vein is possible and, when present, it may drain into the median cubital vein Dorsal venous network of hand medially into basilic v. and laterally into cephalic v. superficial, dorsal aspect of digits unlike the foot, a distinct arch may be absent in the hand, replaced by a dorsal venous network of veins Basilic dorsal veins of hand medially; superficial veins of forearm, median cubital vein dorsal metacarpal veins UPPER LIMB o Structure LYMPHATICS Location Axillary nodes axilla Pectoral nodes lateral border of pectoralis major Lateral axillary along distal axillary v. Posterior axillary anterior to subscapularis m. Central axillary along axillary v. posterior to pectoralis minor m. Apical axillary along axillary v. medial to pectoralis minor m. at apex of axilla Afferents from Efferents to Regions drained efferents form subclavian trunk upper limb, most of breast, some anterolateral chest wall most of breast, anterolateral chest wall & muscles central axillary nodes anterolateral thoracic wall and muscles, including most of the mammary gland small nodes in cubital fossa central axillary nodes upper limb central axillary nodes posterior shoulder lateral, anterior & posterior axillary nodes apical axillary nodes upper limb, breast, posterior shoulder, lateral chest wall central axillary nodes subclavian lymph trunk upper limb, breast, posterior shoulder, lateral chest wall Additional Info axillary nodes are grouped as: 1) pectoral/anterior nodes, along lower border of pectoralis major; 2) lateral nodes, distal on axillary v 3) central nodes, centrally located along axillary v.; 4) subscapular/ posterior nodes, along subscapular v. & tributaries; 5) apical nodes, at apex of axilla, receiving lymph from all other groups LOWER LIMB o Artery ARTERIES Source Branches Supply Additional Info Femoral external iliac superficial epigastric a., superficial circumflex iliac a., superficial & deep external pudendal aa., deep femoral, descending genicular, popliteal thigh, leg & foot the femoral a. is continuous with the popliteal a.; the name change occurs at the adductor hiatus Femoral, deep femoral medial & lateral circumflex femoral aa., perforating aa. (~3 or 4) hip joint, proximal thigh, posterior thigh the primary blood supply to muscles of the posterior compartment of the thigh Iliac, external common iliac inferior epigastric, deep circumflex iliac, femoral lower limb external iliac a. is continuous with the femoral a.; the name change occurs at the inguinal ligament; the common iliac artery bifurcates anterior to the sacroiliac articulation Obturator internal iliac, anterior division pubic br., acetabular br., anterior br., posterior br. medial thigh & hip anterior & posterior brs. pass on anterior and posterior sides of adductor brevis m. Circumflex femoral, medial deep femoral (or femoral) ascending & descending brs. medial thigh & hip Circumflex femoral, lateral deep femoral (or femoral) ascending, transverse & descending brs. lateral thigh & hip Popliteal femoral anterior & posterior tibial; 5 genicular brs. knee, leg & foot the popliteal a. is the continuation of the femoral a.; the name change occurs at the adductor hiatus Gluteal, inferior internal iliac, anterior division Gluteal, superior internal iliac, posterior division superficial br., deep br. gluteus maximus, medius & minimus, hip joint Internal pudendal internal iliac a., anterior division inferior rectal a., perineal a., artery of the bulb of the clitoris/penis, urethral a., deep clitoral/penile a., dorsal clitoral/penile a. anus, muscles of the superficial and deep perineal spaces, clitoris/penis, posterior aspect of the scrotum/labium majus internal pudendal a. is the primary blood supply to the perineum Femoral, deep femoral medial & lateral circumflex femoral aa., perforating aa. (~3 or 4) hip joint, proximal thigh, posterior thigh the primary blood supply to muscles of the posterior compartment of the thigh anterior tibial a., posterior tibial a., 5 genicular brs. knee, leg and foot the popliteal a. is the continuation of the femoral a.; the name change occurs at the adductor hiatus cruciate ligaments & deep structures of knee anastomoses with other genicular brs. of popliteal a., circumflex fibular a. & anterior tibial recurrent a. to form genicular anastomosis lateral aspect of knee anastomoses with other genicular brs. of popliteal a., circumflex fibular a. & anterior tibial recurrent a. to form genicular anastomosis medial aspect of knee anastomoses with other genicular brs. of popliteal a., circumflex fibular a. & anterior tibial recurrent a. to form genicular anastomosis fibular (peroneal), circumflex fibular, nutrient a. of tibia, communicating br., posterior medial malleolar brs., medial calcaneal brs., lateral & medial plantar aa. posterior & lateral leg, plantar aspect of foot posterior tibial bifurcates on the medial side of the foot to give rise to the medial and lateral plantar aa. nutrient br., lateral malleolar br., communicating br., perforating br. lateral leg & ankle anastomoses at ankle with anterior & posterior tibial aa. anterior & posterior tibial recurrent; anterior, medial & lateral malleolar; dorsalis pedis anterior leg, dorsal & deep foot anterior tibial a. becomes continuous with the dorsalis pedis a.; name change occurs at the level of the ankle joint Popliteal femoral a. Genicular, middle popliteal Genicular, superior lateral popliteal Genicular, superior medial popliteal Tibial, posterior Fibular Tibial, anterior gluteus maximus, hip joint popliteal posterior tibial popliteal participates in the formation of the cruciate anastomoses of the hip Plantar, medial digital brs. (3) superficial foot medially becomes continuous with the plantar arch; proper plantar digital a. to lateral side of 5th digit deep foot; the plantar arterial arch and its brs. supply the toes, including the distal phalangeal segment dorsally plantar metatarsal aa. (4) deep foot; its plantar metatarsal brs. and their brs. supply the toes, including the distal phalangeal segment dorsally lateral & medial tarsal aa., arcuate a., 1st dorsal metatarsal a., deep plantar a. dorsal aspect of foot; the anterior tibial artery anastomoses with plantar continues as the dorsalis pedis; arterial arch the name change occurs at the level of the ankle posterior tibial Plantar, lateral posterior tibial Arch, plantar arterial lateral plantar Dorsalis pedis anterior tibial a. Plantar, deep deep foot dorsalis pedis anastomoses with plantar metatarsal aa., but does not usually participate in formation of the plantar arch anastomoses with the deep plantar br. of the dorsalis pedis a. anastomoses with lateral plantar a. to form the plantar arterial arch LOWER LIMB o Vein Dorsal venous arch of foot Saphenous, greater VEINS Tributaries dorsal digital vv. and dorsal metatarsal vv. medial end of dorsal venous arch of foot, perforating communications, superficial epigastric, superficial Drains Into Regions Drained great saphenous v. medially, small saphenous v. laterally dorsum of digits & superficial structures of dorsum of foot femoral v. superficial structures of medial lower limb; lower abdominal wall, Additional Info frequently used as graft material in coronary bypass surgery circumflex iliac, superficial external pudendal Epigastric, superficial none Saphenous, lesser Popliteal perineal region greater saphenous v. superficial fascia and skin of the lower abdominal wall lateral end of dorsal venous arch of foot popliteal v. superficial lateral foot & leg anterior & posterior tibial vv., lesser saphenous v. continues as femoral v. foot & leg superficial epigastric v. communicates with paraumbilical vv. and may enlarge in portal hypertension, producing the sign called caput medusae lies posterior to popliteal a. within popliteal fossa UPPER LIMB o Structure Superficial inguinal nodes LYMPHATICS Location in superficial fascia parallel to inguinal ligament & along greater saphenous v. Deep inguinal nodes medial to femoral v. deep to fascia lata & inguinal ligament Popliteal nodes Afferents from popliteal fossa along popliteal vessels superficial inguinal & popliteal nodes Efferents to Regions drained deep inguinal nodes external genitalia; superficial parts of lower limb external iliac nodes lower limb, external genitalia, lower anterior abdominal wall deep & superficial inguinal nodes leg & foot Additional Info the deep inguinal node in femoral canal is called node (or gland) of Cloquet Surface & Functional Anatomy (syllabus) Understand and explain the anatomical basis of the peripheral vascular examination including the relevant surface anatomy of the peripheral arteries, veins and lymphatics. Peripheral Vascular Examination Inspection o Introduce etc....explain, consent, wash hands o Expose the patient from the waist down + exposed upper limbs o Look around the bed for the usual ie “does the patient look sick?”, Oxygen, Inhalers/GTN, Catheters, Drains, Fluids, Dressings, Position, Comfortable o Vital Signs o At the end of the bed - Colour of the Limbs (pale/blue/black), Hair Loss, Ulcers, Scars, Muscle Wasting, skin changes o Closer inspection of the lower limbs - especially lower medial 1/3 as venous insufficiency effects this region first Any signs of gangrene or pre-gangrene such as missing toes or blackening of the extremities. The presence of any ulcers – ensure you check all around the feet including behind the ankle and in between the toes. Ulcers may be venous or arterial. Any skin changes such as pallor, change in colour (eg purple/black from haemostasis or brown from haemosiderin deposition), varicose eczema or sites of previous ulcers. Compare size of both legs especially at ankle level for evidence of oedema. Venous Stars – minute veins radiating from a single feeding vein. Visible sc veins - note distribution, size, tortuosity, any associated erythema or tenderness Presence of any varicose veins – often seen best with the patient standing o Signs of Chronic Venous Insufficiency – eczema, lipodermatosclerosis, inverted champagne bottle legs, cutaneous haemosiderin deposits Palpation o Palpation of the limbs – paying attention to temperature as well as any abnormalities identified in inspection o Check capillary refill by gently pinching the nail bed and counting the return time (normal is < 3 secs) o Palpate pulses Femoral – feel over the medial aspect of the inguinal ligament. Aorta abdominal – placing two fingers either side of umbilicus (expansile) Popliteal – ask the patient to flex their knee to roughly 60º keeping their foot on the bed, place both hands on the front of the knee and place your fingers in the popliteal space. Posterior tibial – felt posterior to the medial malleolus of the tibia. Dorsalis pedis – feel on the dorsum of the foot, lateral to the extensor tendon of the great toe o Listen for bruits at aorta, iliac and femoral artery o Check for radio-femoral delay. Palpate both the radial and femoral pulses on one side of the body. The pulsation should occur at the same time. Any delay may suggest coarctation of the aorta. o o o o o Fascial Defects - Feel along course of veins (Note tension in vein) and any tender fascial defects (usually at 5, 10 and 15 cm above medial malleolus) Pitting Oedema Sc Tissues - Thickening and tenderness Vein - Press on vein from above noting presence of retrograde flow Cough impulses - over saphenofemoral and saphenopopliteal junctions, noting any bulging with increased transmitted pressure Trendelenburg Test o Ask the patient to lie down & raise the leg to empty the veins. o Place 2 fingers over the saphenofemoral junction. o Ask the patient to stand up. o Release pressure at the junction o If the veins remain empty while standing, the saphenofemoral junction is incompetent. Tourniquet Tests Patient Supine with Leg elevated o Sweep veins empty (Note how easily the veins empty - may give signs of occlusion / compression)- if fail to empty this suggests high pressure within them o First place a tourniquet around upper third of thigh to occlude superficial veins Then Patient Standing o If veins above tourniquet distend - Saphenofemoral Junction is incompetent o If veins below tourniquet fill there must be a perforator below level of tourniquet therefore once again elevate the leg and repeat the procedure with the tourniquet at a lower position on leg. (Note: Alternatively – one can use multiple tourniquets and simply release them sequentially)