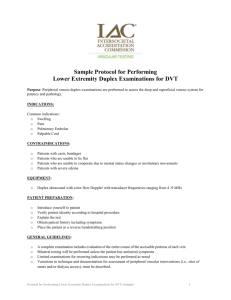
Deep Vein Thrombosis..
advertisement
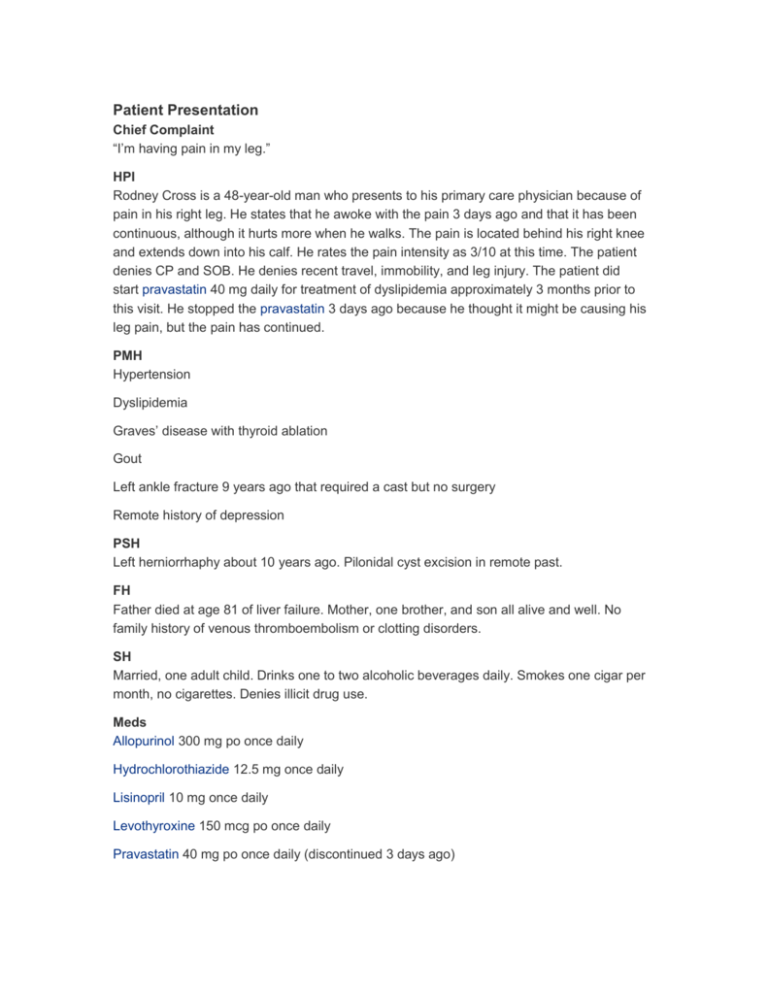
Patient Presentation Chief Complaint “I’m having pain in my leg.” HPI Rodney Cross is a 48-year-old man who presents to his primary care physician because of pain in his right leg. He states that he awoke with the pain 3 days ago and that it has been continuous, although it hurts more when he walks. The pain is located behind his right knee and extends down into his calf. He rates the pain intensity as 3/10 at this time. The patient denies CP and SOB. He denies recent travel, immobility, and leg injury. The patient did start pravastatin 40 mg daily for treatment of dyslipidemia approximately 3 months prior to this visit. He stopped the pravastatin 3 days ago because he thought it might be causing his leg pain, but the pain has continued. PMH Hypertension Dyslipidemia Graves’ disease with thyroid ablation Gout Left ankle fracture 9 years ago that required a cast but no surgery Remote history of depression PSH Left herniorrhaphy about 10 years ago. Pilonidal cyst excision in remote past. FH Father died at age 81 of liver failure. Mother, one brother, and son all alive and well. No family history of venous thromboembolism or clotting disorders. SH Married, one adult child. Drinks one to two alcoholic beverages daily. Smokes one cigar per month, no cigarettes. Denies illicit drug use. Meds Allopurinol 300 mg po once daily Hydrochlorothiazide 12.5 mg once daily Lisinopril 10 mg once daily Levothyroxine 150 mcg po once daily Pravastatin 40 mg po once daily (discontinued 3 days ago) All NKDA ROS Constitutional: No chills, no fatigue. Eyes: No eye pain or changes in vision. ENT: No sore throat. Skin: No pigmentation changes, no nail changes. Cardiovascular: No CP, palpitations, or syncope. Respiratory: No cough, SOB, wheezing, or stridor. GI: No abdominal pain, nausea, diarrhea, or vomiting. Musculoskeletal: No neck pain, back pain, or injury. Neurologic: No dizziness, headache, or focal weakness. Psychiatric/behavioral: Remote history of depression. Not a current problem. Physical Examination Gen Somewhat overweight, Caucasian man who appears comfortable. Cooperative, A & O × 3, normal affect. VS BP 132/76, P 75 regular, R 16, T 98.3°F, O2 sat 97/RA; Wt 194 lb, Ht 6′0″ Skin Warm, dry, normal color. No rash or induration. HEENT Pupils equal and reactive to light. EOM intact. Mucous membranes moist and pink. Neck Normal range of motion with no meningeal signs Lungs/Thorax Breath sounds normal, no respiratory distress CV RRR, no rubs, murmurs, or gallops Abd Nontender, no masses, no distension, no peritoneal signs MS/Ext Upper extremities: Normal by inspection, no CCE, normal ROM. Lower extremities: Right calf tight, warm to touch, and tender with 1+ pretibial pitting edema. LLE without redness, warmth, and swelling. Lower extremity pulses and sensation are normal bilaterally. Normal ROM. Neuro Glasgow coma scale of 15, no focal motor deficits, no focal sensory deficits Labs Na 140 mEq/L K 3.9 mEq/L Cl 103 mEq/L CO2 27 mEq/L BUN 10 mg/dL SCr 0.84 mg/dL Glucose 88 mg/dL Uric acid 5.0 mg/dL CK 117 IU/L WBC 5.9 × 103/μL RBC 4.28 × 106/μL Hgb 13.5 g/dL Hct 39.3% MCV 92.0 fL MCHC 34.4 g/dL RDW 14.3% Platelets 175 × 103/μL Mean platelet volume 7.2 fL Granulocytes, electronic 51.0% Lymphocytes, electronic 38.2% Monocytes, electronic 8.4% Eosinophils, electronic 1.9% Basophils, electronic 0.5% INR 1.0 Lower extremity venous duplex ultrasonography: “Acute DVT of right distal superficial femoral, popliteal, and peroneal veins. No compression or flow in these vessels.” (Note to reader: The “superficial femoral vein” is actually a deep vein, in spite of its name. Use of the name “femoral vein” is preferred because it is less confusing. However, the name “superficial femoral vein” is still encountered, as it is in this patient’s venous duplex report.) Assessment Acute DVT in right distal femoral, popliteal, and peroneal veins