Dissecting a pressure
advertisement

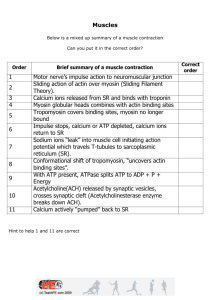
MSP PHYSIO PROBLEM SET #1 1) a. As capacitance vessels, veins contain the majority of blood volume at rest. How does venular structure contribute to this property? Answer: Not only do veins have a smaller wall thickness relative to arteries, but they also contain less smooth muscle and more collagen in comparison. As a result, veins are very compliant (“less stiff”) which allows them to substantially increase their volume with an increase in pressure. In other words, veins easily expand, thus serving as a reservoir (or sink) for the vasculature’s blood. b. During stress/exercise, autonomic regulation constricts veins. How does this affect central venous pressure and the relative distribution of blood in the vascular tree (i.e. relative volume in arterial vs. venous system)? Answer: Upon constriction, the venous pressure increases and vessel capacitance decreases, hence a portion of “storage” blood is now distributed into the arterial system (for delivery to tissues). (via increased preload) 2) One day while in his office, your preceptor (an internist) decides to test your knowledge of cardiac physiology. He hands you a copy of the “wigger’s diagram” and asks the followinga. “Immediately following S1, which valve opens first and why?” Answer: A glance at the diagram shows that pulmonary artery pressure begins to rise before aortic pressure, thus the pulmonary valve must open first. Reason: the diastolic pressure in the pulmonary valve is smaller than that of the aorta. b. “A distinction is made between electrical systole and mechanical systole. Can you show me which points on the diagram indicate the beginning of each? Also, why don’t the electrical and mechanical events occur simultaneously?” Answer: Electrical systole begins at the letter Q of the ECG, while mechanical systole begins at the isovolumic contraction of the left ventricle. These two events do not coincide for a number of reasons including: a substantial number of cells must be depolarized for the muscle to contract and; delta V must open voltage-dependent Ca channels so that extracellular Ca will lead to release of sarcoplasmic reticulum Ca (Ca-induced release of Ca) which will eventually bind to troponin and lead to contraction. c. “You’re doing very well, so this is the last question.” Suppose that a patient presents with tricuspid insufficiency [due to strep endocarditis ]. Briefly describe changes (if any) which would occur in the right atrial pressure trace?” Answer: assuming there is no stenosis, the a wave should be the same. The c wave will greatly diminish, but the v wave will become gigantic. 3.) Refer to the P-V loop in your notes for the following questions. a. Write the equation for ejection fraction using letters on the diagram (e.g. E.F. = cxa/b-d). Answer: ejection fraction = b-d/b b. According to the diagram, what is this person’s systolic and diastolic pressure? Answer: Since rapid ejection begins at C, this is the diastolic pressure (80 mm Hg). Systolic pressure is equal to the max LV pressure of approx. 110 mm Hg. c. Which letter is closest to the region of aortic valve closure? Answer: The aortic valve closes as isovolumic relaxation begins which is D. 3. You’re talking to a patient who has recently had a heart transplant. The patient relates, “I was warming up to go running during my lunch break when I saw a group of devastatingly good looking students walking down the hall -I think their shirts and jackets said class of 2001 on them. So I notice that a little later my heart starts beating faster, and things get worse when I start running. My heart gets beating super fast, and I start feeling light-headed so I have to stop. I can’t approach those second-year medical students, I get so nervous, so I figured that you might know what’s going on.” Answer: As HR increases, the time to fill the heart (diastole) decreases more than systole. Because of Starling’s Law, the stroke volume decreases. Also, a faster heart rate leads to a shift of blood from veins to arteries, thus decreasing preload and increasing afterload – both of which also contribute to a decreased stroke volume. At high enough heart rates, the stroke volume is very low, as the heart has so little time to fill. Cardiac output decreases, the patient feels light-headed as less bloodflow gets to the brain. 4. On your first preceptor visit after Christmas break, your preceptor’s office is busier than the return/exchange lines the day after Christmas. While running down the halls and almost out of breath, your preceptor quickly asks, “Are you taking cardiac physiology yet?” You nod your head, and your preceptor says, “Good. I gotta go to the bathroom – gotta cut back on the coffee -- but if you could figure out this patient’s stroke volume before I get back, that’d be great. All the information you need should be on the front page of the chart. Use the Fick, Luke!” Before you can confess how little you’ve studied, your preceptor is gone. You look at the patient’s chart and see: Hb: 15 gm/dl x 1.36 ml O2 / gm Hb x 10 = 204 mL O2 / L blood Pulmonary Vein O2 saturation: 95% Pulmonary Artery O2 saturation: 60% VO2 = 250 mL/min (Vo2 is a measure of O2 consumption) HR = 100 You concentrate and hear “Use the Fick, Luke…” echoing in your head. Your preceptor returns and says, “Well, my young jedi student doctor, what is the patient’s stroke volume? You respond in your best Yoda voice: Answer: Fick’s says that CO = VO2/ (arterial-venous O2 difference) a-v difference = 204 mL O2/L blood (.95 - .6) = 71.4 mL O2/L blood CO = (250 mL O2/min) / (71.4 mL O2/L blood) = 3.5 L/min SV = CO/HR = (3.5L/min)/(100 min-1) = .035 L or 35mL (normal stroke volume is ~ 75 mL) also be prepared to discuss sampling sites for venous blood Dissecting a pressure-volume curve D C B A 6) a. What sets the upper boundary of these loops (the upper dotted line)? This line represents the Frank-Starling mechanism. It is set by the systolic pressure that would be produced in a purely isovolumetric contraction from a given end diastolic end-diastolic volume (EDV). The larger the EDV, the greater the stretch of the ventricle and subsequently the greater the tension and pressure which develops. A normal intact ventricle only operates on the ascending limb of the length-tension curve. b. What sets the lower border of the loops (lower dotted line)? The lower border is set by the passive pressure-volume curve of the relaxed ventricle. c. Which of the four loops (A,B,C,D) represents the greatest stroke volume? Stroke volume = EDV – ESV. It is represented by the width of the loop, thus loop B reflects the greatest volume change. d. What happened physically between loop A (the control state) and loop B? Loop B shows the effect of increasing the end-diastolic volume; stroke volume increases provided the arterial pressure (afterload) does not change. e. What can cause the loop to change from B to C? There is an increase in arterial pressure in loop C. The stroke volume decreases, provided the EDV does not change. f. How can you explain “loop” D? Loop D depicts a purely isovolumetric contraction. 7) Considering all the free time you have in med school, you decide you want to start marathon training. On one of those long training runs you start thinking about your heart. You remember from physiology that your heart becomes more efficient, and the "muscle pump" increases the return of the blood to your heart. Describe the mechanism and effect of this increase . The concept we are dealing with is increased preload. Increased blood return to the heart increases the end diastolic pressure which causes stretching of the myocardium. The stretched myocytes have increased force of contraction. Maximum force of contraction develops at sarcomere lengths of 2.2-2.3um. The sarcomere length of the heart at normal enddiastolic pressure is below this optimal value. Beyond 2.2-2.3 um the contraction force decays, but it is difficult to stretch sarcomeres beyond this point even in vitro. Part of the explanation is that at sarcomere lengths below 2.0 um, the opposing actin filaments overlap each other or buckle and this interferes with the formation of actin-myosin crossbridges. Also important in cardiac muscle is the length-dependent calcium sensitivity. The mechanism of this is unknown but experimentally it has been measured that there is a substantial reduction in the calcium concentration needed to produce 50% of maximal tension in the stretched heart. All these concepts relate to Starling's Law of the heart, which simply states that the greater the stretch of the ventricle in diastole, the greater the stroke work achieved in systole. 8) At your preceptor's office you encounter a heavy set middle aged man who complains that he loses his breath after climbing one flight of stairs, and it seems to be getting worse. During the course of HEADS, you find that he smokes 50 pack years (2 packs a day for 25 years). In addition you find out that he enjoys drinking a "couple" beers with his buddies after work, and then goes home and has a "couple" more while eating fried chicken and watching TV. In addition, he does not like doctors, and has not seen a physician since his discharge from the Navy 15 years ago. After taking blood pressures all first semester, you expertly find that his blood pressure is 200/120. Illustrate how this history will affect the output of the heart. 1. This man has hypertension. Initially his high diastolic pressure will lead to pathology. This man is feeling a huge afterload. The ejection phase of the heart can only occur after the ventricular pressure rises higher than the arterial diastolic pressure. Much of the energy of the heart will be wasted in isometric contraction just to reach pressures high enough to exceed the arterial pressure. This will reduce the stroke volume and the ejection fraction of the heart. Initially the body will maintain cardiac output by increasing the heart rate. (this is about as much as the MSP students need to know right now) Further information below. 2. The preload of the heart will increase in the chronic state due to venoconstriction and the renin-angiotensin response which will increase the blood return to the heart. The body increases the volume in the heart because it wants to maintain stroke volume so thinks just add more fluid. (They don’t need to know this yet, but do they do need to know the effects of the increase preload.) They should understand that increased preload will increase the contractility of the heart (Starling’s Law) initially. In the chronic state however the increase ventricular pressure will increase the wall tension (Pressure in Law of Laplace). This will serve to increase the oxygen consumption of the heart, reducing its efficiency. Eventually this will overwhelm the heart muscle causing the ventricle to dilate. Again this will increase the oxygen demand of the heart (radius in Law of Laplace). Also this will remodel the ventricle to a more spherical shape. Levick points out that the more spherical shape of the heart reduces its efficiency because a smaller component of the wall tension is angled towards the cavity, generating less pressure. The curvature of the ventricle wall determines how effectively the active wall tension is converted into intraventricular pressure. Why is this guy short of breath? There are two reasons for his shortness of breath. The first, as discussed above his stroke volume and cardiac output are diminished. This means that he is not efficiently perfusing his working muscles. This man will feel fatigue even after minimal exertion. Secondly, increased end diastolic pressure in the left ventricle will back up and increase the end diastolic pressure in the left atrium, which will back up into the pulmonary capillaries causing pulmonary edema. As they will learn in respiratory lectures (later), water in the longs decreases the efficiency of the gas exchange, decreasing the oxygen saturation in the pulmonary veins. 9) Your good friend at USC medical school brags to you about his discovery of a novel heart that lacks outer membrane calcium channels. He explains to you how this definitively proves that all of the calcium needed for heart function is present in the sarcomplasm reticulum. Defend or counter the credibility of such a heart. A heart like this could never exist. Our friend at USC is partly right most of the calcium for cardiac myocyte contraction does come from the SR (8090%). However external calcium is integral in excitation-contraction coupling. The plateau phase of the heart action potential is due to entry of external calcium into the myocyte. Experimentally it has been shown that the size of plateau currents directly affect the strength of contraction of the cardiac myocytes. The externally derived calcium is integral in facilitating calcium-induced calcium release of the much larger and more important calcium store in the SR. 10) Explain how digoxin works in treating heart failure, given that it inhibits the Na/K pump. Feel free to use diagrams and mention all the channels involved. Digoxin is used to treat heart failure by enhancing the myocardial contractile force. It achieves this by increasing the level of intracellular calcium. Digoxin slows down the sarcolemmal Na/K pump by inhibiting its ATPase activity. This produces a rise in intracellular sodium concentration and a fall in the sodium gradient across the cell membrane. Since the Na/Ca exchanger is driven by the sodium gradient calcium expulsion is slowed and calcium accumulates in the cell. This increases the amount of calcium available to bind to troponin for every excitation. 11) Draw the force curve for isometric contraction and explain the events occurring between the actin and the myosin. _____ | | -------I tried to make it look like a flat curve as seen on page 21 of the Homsher notes. Initially the crossbridge is detached in the bent confirmation with ADP and Pi bound to it. Then the crossbridge collides with an interaction site on the actin molecule and becomes strongly attached to the actin. Then the Pi dissociates from the myosin head prompted by the conformational change associated with the actin binding to the crossbridge. Then a force is applied to the system (holding the barbell up in the air). This causes the myosin neck to assume the straightened form which stretches the S-2 segment. In isometric contraction the force exerted by the S-2 segment to keep the sarcomere from increasing in length by definition has to be equal to the force applied by the environment on the sarcomere. The crossbridge may stay in this conformation for several hundred ms. Then the ADP dissociates, the forms the plateau phase of the force curve (the actin and myosin are still attached in the extended neck form). ATP rapidly binds to the active site. Soon after ATP binds to the catalytic site the crossbridge detaches from the actin and the force between the thick and thin filaments falls to zero. Over the next 10-30 ms the crossbridge hydrolyzes the ATP returning the crossbridge conformation back to the first step so that the cycle can resume.