Audit steps
advertisement
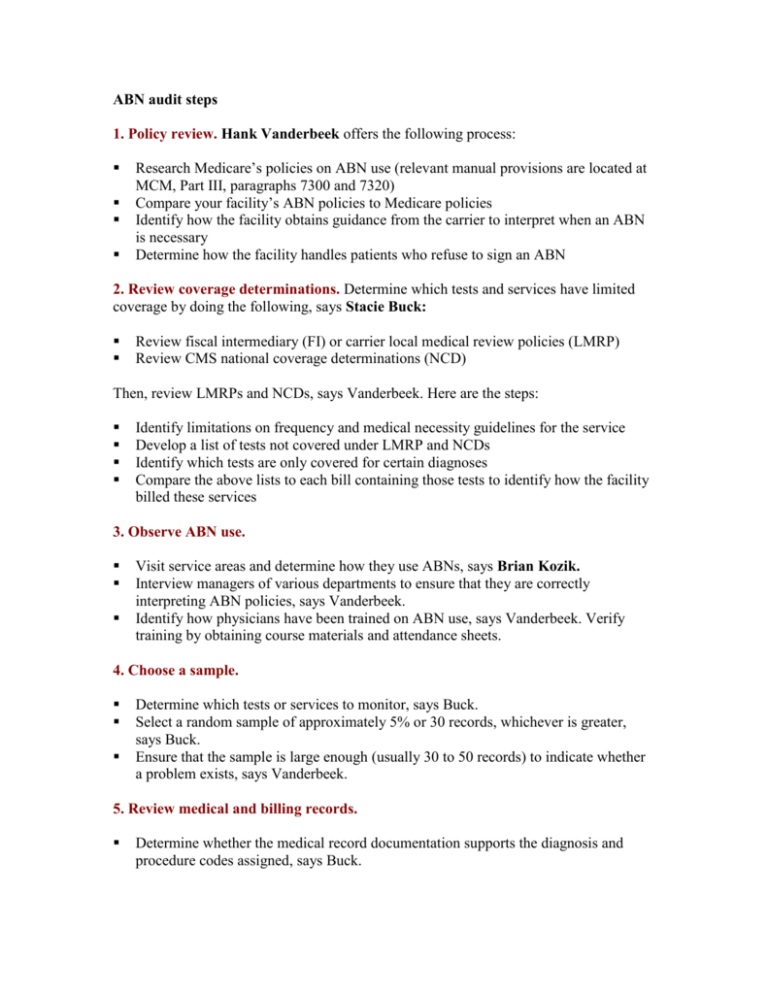
ABN audit steps 1. Policy review. Hank Vanderbeek offers the following process: Research Medicare’s policies on ABN use (relevant manual provisions are located at MCM, Part III, paragraphs 7300 and 7320) Compare your facility’s ABN policies to Medicare policies Identify how the facility obtains guidance from the carrier to interpret when an ABN is necessary Determine how the facility handles patients who refuse to sign an ABN 2. Review coverage determinations. Determine which tests and services have limited coverage by doing the following, says Stacie Buck: Review fiscal intermediary (FI) or carrier local medical review policies (LMRP) Review CMS national coverage determinations (NCD) Then, review LMRPs and NCDs, says Vanderbeek. Here are the steps: Identify limitations on frequency and medical necessity guidelines for the service Develop a list of tests not covered under LMRP and NCDs Identify which tests are only covered for certain diagnoses Compare the above lists to each bill containing those tests to identify how the facility billed these services 3. Observe ABN use. Visit service areas and determine how they use ABNs, says Brian Kozik. Interview managers of various departments to ensure that they are correctly interpreting ABN policies, says Vanderbeek. Identify how physicians have been trained on ABN use, says Vanderbeek. Verify training by obtaining course materials and attendance sheets. 4. Choose a sample. Determine which tests or services to monitor, says Buck. Select a random sample of approximately 5% or 30 records, whichever is greater, says Buck. Ensure that the sample is large enough (usually 30 to 50 records) to indicate whether a problem exists, says Vanderbeek. 5. Review medical and billing records. Determine whether the medical record documentation supports the diagnosis and procedure codes assigned, says Buck. 6. Verify ABN validity. Ensure that ABNs contain the following, says Buck: Model language as provided by CMS in the two ABN-approved forms: CMS-R-131G and CMS-R-131-L Specific information about the test or service that Medicare may not pay for A specific reason the facility believes Medicare may not pay for the test or service A signature by the patient or the patient’s representative 7. Review the use of the GA modifier. Do the following, says Buck: Verify that an ABN is on file Identify whether the facility has attached the GA modifier to each procedure listed on the ABN Note: If the facility does not sue the GA modifier, Medicare will issue a contractual denial, leaving the facility liable for the payment, says Buck. 8. Monitor compliance on an ongoing basis. Use the following tips, says Buck: Perform this audit at least quarterly to identify and correct issues Review claims denials to assess ABN compliance