Trifecta for Change:
Enhancing Antenatal Care in Ontario
TEC Talk
May 27th, 2013
Mari Teitelbaum
Michael Pluscauskas, Sandra Dunn, Tracy Carr, Brenda Bonner, Douglas Cochen
BORN Ontario
The best possible beginnings
for lifelong health
2
Facilitation of Care: Access to Information
• Sarah, from Toronto, is having
a weekend away with friends,
she is 34 weeks pregnant
• Delivers unexpectedly at the
London Health Sciences Centre
• How will the delivering
obstetrician access her
pregnancy health records?
3
Pregnancy in Ontario
140k women
Cared for by:
Midwife
Family doctor
Community
obstetrician
High risk obstetrician
Nurse practitioner
Delivering:
Pregnancy Care Reminders
Ultrasound
LMP
4
Prenatal
Screening
Newborn Screening
Plan labour
GBS
Prenatal
within 48 hrs of
& birth
Transmit Screening
birth
Education Diabetes
Forms to
Screening
Hospital
Antenatal Forms
Consistent care
Facilitates
communication
Gold standard
5
✗ Up to 10% of the
time the forms
are missing –
early delivery,
unexpected
location or lost
✗ Practices
associated with
the pathway
change regularly
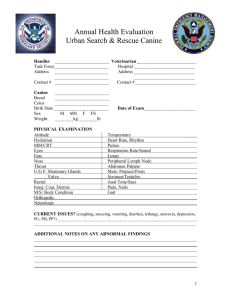
First Visit(s): Early Prenatal Care
Medical History
Pregnancy Summary
LMP:
Certain Y/N
Cycle q:
Regular Y/N
Contraceptive Type
Last Used
Gravida
Term
Premature
Abortuses
Living
EDB by
dates:
Dating Method:
Dates
T1 US
T2 US
ART (e.g. IVF)
Final EDB:
Liver, hepatitis, GI
Y/N Epilepsy / Neurological Y/N Chromosomal disorders
Y/N
Gynaecology / Breast
Hem/Immunology
Y/N Other
Y/N
Y/N
STDs / HSV / BV
Birth Weight
Length of Labour
Place of Birth
Type of Delivery
Tuberculosis risk
Other
Occup / Environ Risks
Dietary restrictions
Calcium adequate
Preconceptual folate
Y/N
Y/N
Y/N
Y/N
At risk population
Family History:
Developmental delay
Congenital anomalies
Y/N
Y/N
Y/N
Y/N
BMI
N / AbN
N / AbN
N / AbN
N / AbN
N / AbN
N / AbN
Wt
External Genitalia
Cervix, vagina
Uterus
Size: _____ weeks
Adnexae
Other
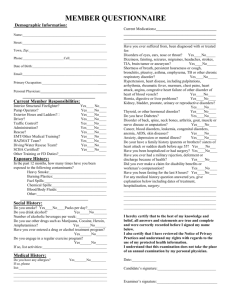
0- 4
5
6
7
8
Laboratory Investigations
Hb
Antibody Screen
MCV
Rubella Immune
ABO
HBsAg
Rh
Rh -ve
Give
Rh-IG
(28wks)
HIV
11
High risk
1 hr
GCT
GC/Chlamydia
12
10-13+6
wks
15
16
17
IPS
FTS
NT
Adjust
EDB
AbN level maternal SOGC Guidelines
Consult OB to
serum marker
establish fetal
surveillance plan
Y/N
Y/N
Y/N
Y/N
Other
Isolated
+ risk >
1/600
At risk population Y/N
Previous C-Section:
Consider VBAC vs.
Repeat C-Section
35+ or
MSS +ve
or other
soft
markers
Enlarged
cysterna
magna
Expert review
+ further
evaluation
pyelectasis
Neonatal u/s
N / AbN
N / AbN
Fetal
anatomy
review
Mild
ventriculomegaly
Fetal
karyotyping
18
19
20
Fetal anatomy /
morphology
18-20 wks
Establish Risk +
Counsel
If 1st visit
Second trimester
14-20+6 wks screening (Quad)
CVS / amnio
Expert
review
Grade 2, 3
echogenic
bowel
3rd trimester
scan
pelvis
>10mm
pelvis
≥ 5mm
21
22
23
24
25
26
27
28
Finalize EDB
MSS
> 5 days discrepancy
with LMP estimate
declined or twins
2nd trimester screen for
open neural tube defects
14
Choroid
plexus
cysts
EICF
Subsequent Visits: Ongoing Prenatal Care (see next page)
Dating scan 11-14 wks
(early if larger than dates)
If 2 U/S, use 1st for EDB
SOGC guidelines for
screening options
MSAFP
13
Ultrasound
Urine C&S
If father known,
consider Rh test
6 Genetic
Prenatal
Investigations
10
Last Pap
Sickle Cell VDRL
Father
+ve
9
Thickened
nuchal fold
Y/N
Y/N
Family violence
Parenting concerns
Relig. / Cultural issues
Family violence
BP
N / AbN
N / AbN
N / AbN
Single
umbilical
artery
establish risk + counsel
Psychosocial
Y/N
Y/N Poor social support
Relationship problems Y/N
Y/N
Emotional / Depression Y/N
Y/N Substance abuse
Y/N
Y/N
Family History:
First Visit (s): Identify Risk Factors and Management Plan
W
E
E
K
Soft Markers for Aneuploidy:
Y/N
Genetic disorders
Physical Examination
Ht
Thyroid
Chest
Breasts
Cardiovascular
Abdomen
Varicosities / Extrm.
Current Pregnancy
Y/N
Y/N
Y/N
Y/N
Surgery
Blood Transfusion
Anaesthetic compl.
Psychiatric
Infectious Disease
Comments re: pregnancy and birth
Bleeding
Nausea, vomiting
Smoking___cig/day
Alcohol, street drugs
Y/N
Y/N
Y/N
Y/N
Varicella Susceptible
Obstetrical History
No.
Year
Sex M/F
Gest. Age (weeks)
Genetic History
Hypertension
Endocrine
Urinary tract
Cardiac/Pulmonary
Abnormal
Cervical
Length
Change
Assess preterm
birth risk
Soft Markers
for Aneuploidy
(see box above)
> 10 days discrepancy
Adjust EDB
with LMP date
Consult with specialist
Fetal
and genetic counselor
Structural
Anomaly
Placental
Edge
Overlap
Refer to tertiary
ultrasound unit
Repeat U/S, consider
further imaging
3rd Trimester exam
and follow-up re: need
for C-Section
Diagnostic and
Screening Tests
2nd Test: Hb,
ABO/Rh,
Repeat ABS
1 hr GCT
Administer
Rh-IG
Repeat 1hr GCT
in high risk -ve
Value 7.8-10.3
1 AbN test
2 hr GCT
Glucose
Value >10.3
Level AbN
Diagnose
Gestational
Diabetes
Glucose
intolerance
Follow Canadian
Diabetes
Association
Guidelines
A1A2 Pilot Project
• Launched in 2011, partnership between E-Health
Ontario and BORN, the project had 3 Goals
1.
Improve practitioner use of high quality clinical practice guidelines
(CPGs) and pathways for antenatal care. (partnership of BORN and Centre
for Effective Practice)
2.
3.
Automate the flow of data collected on A1/A2 to facilitate care to
women who may arrive at an Ontario birthing hospital without an
antenatal record
Enhance the quality of data available to support QI, system planning
and surveillance of pregnancy and birth
• Participants
7
– 1 EMR Vendor (OSCAR)
– 4 family health teams
– 3 hospitals
Clinical Input
8
EMR Enhancements
9
System Enhancements
BORN
Registry
10
System Impact
BORN
Registry
Population
Organization
Provider
Individual
11
Trifecta: Pregnancy Pathway
Value to the provider
beyond what is in their
Clinical pathway
chartembedded in
primary care practice
Connection to the
individual patient –
clinical impact and
Patient
information
outcomes
available when and where it
is needed
12
Trusted &
Authoritative
Created by clinicians and
subject matter experts using
OMA standard forms
Pilot Learning
• 573 records in the BORN Information System
• Preliminary evaluation findings: ‘Good’*
– Integration & Coordination of Care
– Evidence-based Care & Patient Safety
– Workflow Efficiency
• Critical Success Factors
– Well defined scope
– Governance
– The Trifecta
• Many new opportunities!
13
So many to Thank
•
•
•
•
•
14
eHealth Ontario
Participating family health teams
OSCAR
Perinatal Services BC
Centre for Effective Practice
Questions
15