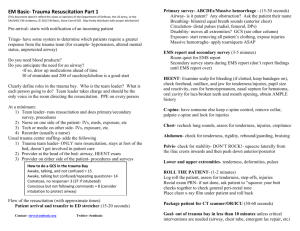
Heart of Texas Regional Advisory Council
advertisement

Heart of Texas Area Regional Advisory Council (HOTRAC) Trauma Service Area (TSA) - M Regional Trauma Plan Heart of Texas Regional Advisory Council (HOTRAC) 405 Londonderry, Suite 201 Waco, TX 76712 Email: info@hotrac.org For the state service delivery area including Bosque, Falls, Hill, Limestone, and McLennan Counties. Phone: (254) 761-7890 Fax: (254) 761-7895 HOTRAC Regional Trauma System Plan Revised May 2010 Page 1 Table of Contents Introduction Organization Service Area/Designated Facilities Regional Plan Board of Directors HOTRAC Bylaws TSA M – EMS Services TSA M – Air Medical Providers TSA M – Hospital Facilities System Participation System Access Communications Regional Medical Oversight & Control Pre-hospital Triage Off-line Medical Control Trauma Triage Criteria Classification of Trauma Patients (Pre-hospital) Helicopter Activation Emergency Department Diversion Facility Bypass Facility Triage Criteria Classification of Trauma Patients (Facility) Inter-hospital Transfers Regional Trauma Alert Form System Performance Improvement (PI) Air Medical PI Form EMS PI Form Trauma PI Form Statement of Confidentiality Appendix A EMS Treatment Guidelines (separate Table of Contents) HOTRAC Regional Trauma System Plan Revised May 2010 3 3 3 4 5 6 20 24 33 34 35 36 38 40 41 41 43 45 45 45 46 49 51 52 54 56 57 58 59 Page 2 Introduction Organization and Service Area Organization The Heart of Texas Regional Advisory Council (HOTRAC) is comprised of the Central Texas counties of Bosque, Falls, Hill, Limestone, and McLennan. The HOTRAC was organized and completed the incorporation process in 1994, and became an approved 501 (c)(3) organization in 1995. The HOTRAC mission is to develop a trauma care network for our five-county area and to improve the level of care provided to injured persons living or traveling through this region. Together, through the work of its standing committees, HOTRAC member organizations (hospitals, first responder organizations, EMS providers, air medical providers, emergency management, public health, etc) work cooperatively to ensure that quality care is provided to ill/injured persons by welltrained, well-equipped pre-hospital and hospital care professionals. The Council provides injury prevention & public awareness education to the public, and trauma and emergency education to health care providers in each of the five counties. Service Area/Designated Facilities The HOTRAC Service Area is comprised of four rural counties (Bosque, Falls, Hill, and Limestone) and one urban county (McLennan). The terrain in this region is primarily Black-land prairie with rolling hills located in the Bosque county area. Interstate 35, a heavily traveled transportation artery, transects McLennan and Hill Counties and is the source of many multi-vehicular crashes annually. Also heavily traveled State Highway 6 traverses McLennan, Falls and Bosque counties, while Limestone counties transportation primarily occurs via farm-to-market roads. Bosque County encompasses 989.3 square miles and has a population of 17,204 lives. Goodall-Witcher Healthcare Foundation in Clifton is a DSHS-designated Level IV Trauma Facility and is located in the south-central portion of the county. Goodall-Witcher is a 40-bed acute care facility located in Clifton, Texas and received Level IV Trauma Facility designation originally in 1995. Goodall-Witcher has surgical capability and was the first hospital to become a designated trauma facility in TSA-M. One EMS service provides pre-hospital care in Bosque County. Hill County is located in the northern portion of the region and encompasses 962 square miles. The county population is 32,321 persons. Hill County contains two acute care hospitals: Hill Regional Hospital (a Level IV DSHS-designated trauma facility), and Lake Whitney Medical Center (a non-designated facility). Lake Whitney Medical Center currently has no plans of seeking trauma facility designation. Hill Regional Hospital is a 92-bed acute care facility with surgical capability, which received its Level IV Trauma Facility designation. Lake Whitney Medical Center is located in the western portion of the county. Lake Whitney Medical Center is a 49-bed acute care facility. Five EMS providers provide pre-hospital care in Hill County. Located in the eastern-most portion of the region, Limestone County includes 909 square miles of primarily farm and ranch land. The population in Limestone County is 22,051 persons. Parkview Regional Hospital received its Level IV designation originally in 1996 and is a 77-bed acute care facility with surgical capability. Limestone Medical Center is a 20-bed acute care facility (which does not have surgical capability) and received its Level IV designation originally in 1996. Pre-hospital care is provided primarily by three EMS services. Falls County is located in the southern most part of this Region and encompasses 769 square miles. The county population is 18,576. Falls Community Hospital in Marlin is a DSHS-designated Level IV Trauma Facility with 44 beds and is centrally located in the county. One EMS service provides pre-hospital care in Falls County. HOTRAC Regional Trauma System Plan Revised May 2010 Page 3 McLennan County is the only urban county in the region and covers 1041.9 square miles of Central Texas and has a total population of 213,517 persons. Waco is the largest city in the county (population approximately 115,000) and contains two acute care hospitals: Hillcrest Baptist Medical Center (a Level II DSHS-designated trauma facility), and Providence Health Center (a non-designated facility). Providence Health Center is a 230-bed acute care facility with surgical capability. Providence Health Center currently has no plans of seeking trauma facility designation. The other three hospitals located in Waco are psychiatric facilities. These facilities are Central Texas Veterans Healthcare System – Waco Campus, the Waco Center for Youth (a state facility) and the DePaul Center. Hillcrest Baptist Medical Center, in Waco, Texas is a 237-bed acute care facility. HBMC has had a functional trauma program since 1996 and currently has three (3) trauma surgeons on staff, providing 24-hour per day trauma care. Hillcrest Baptist Medical Center is the lead trauma facility for the HOTRAC region. There are five EMS services and multiple First Responder Organizations in McLennan County. Regional Plan This Plan has been developed in accordance with Texas Department of State Health Services Bureau of Emergency Management guidelines and procedures for implementation of a comprehensive Emergency Medical Services (EMS) and Trauma System plan. This plan does not establish a legal standard of care, but rather is intended as an aid to decisionmaking in general patient care scenarios. It is not intended to supersede the physician’s prerogative to order treatment. HOTRAC Regional Trauma System Plan Revised May 2010 Page 4 Heart of Texas Regional Advisory Council TSA - M 2010 Board of Directors Executive Committee 1. 2. 3. 4. Chair Vice Chair Secretary Treasurer Lori Boyett, HBMC Steve Clinkscales Joyce McDowell, G-W Tracy Brand, HBMC (expires 12/2010) (expires 12/2011) (expires 12/2010) (expires 12/2011) Other Members 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Immediate Past Chair Anita Diebenow, Goodall-Witcher Hillcrest representative Dr. Ted Smith, HBMC Providence representative Eileen Bohanon, Providence Rural Hospital representative Marcy McFarland, Parkview Primary EMS agency for City of Waco representative Dale Yates, ETMC-EMS Rural EMS representative Linda Catena, North Bosque EMS FRO representative Tommy Womack, East Lake Limestone VFD Emergency Management Member-at-Large Frank Patterson, Waco-Mclennan County OEM Physician-at-Large Dr. John Hamilton, Providence Community Member-at-Large Diane Fraley HOTRAC Regional Trauma System Plan Revised May 2010 (expires 12/2010) (expires 12/2011) (expires 12/2011) (expires 12/2011) (expires 12/2011) (expires 12/2011) (expires 12/2011) (expires 12/2010) (expires 12/2011) (expires 12/2011) Page 5 THE HEART OF TEXAS REGIONAL ADVISORY COUNCIL Trauma Service Area (TSA) M BYLAWS Article I – Name This organization shall be known as the Heart of Texas Regional Advisory Council (HOTRAC). The HOTRAC Trauma Service Area includes the counties of Bosque, Falls, Hill, Limestone, and McLennan. The HOTRAC Trauma Service Area is also referred to as TSA M. Article II – Mission Statement To provide the infrastructure and leadership necessary to sustain an inclusive trauma & emergency medical system within our Trauma Service Area by the following actions: A. Assist member organizations in achieving the highest level of trauma and emergency care they are capable of providing, which will result in a decrease in morbidity and mortality and ultimately improve the injured patient’s outcome. B. Encourage activities designed to promote cooperation between member organizations and provide a forum to resolve conflicts regarding the care of the injured patient. C. Provide and facilitate educational programs for the public to increase awareness regarding an inclusive trauma system with a heavy emphasis on prevention activities. D. Assist in the development, acquisition, and operation of facilities to enhance the provision of emergency, trauma, and acute care in TSA M. To provide coordination of acute medical services in the mass casualty and disaster settings. A. Coordinate emergency and disaster preparedness and response activities between area hospitals, EMS providers, public health, and other healthcare entities. B. Provide resources to the Office(s) of Emergency Management regarding acute medical services. C. Participate in the Regional Medical Operations Center and/or the HOTCOG Regional Coordination Center to coordinate disaster activities between area hospitals and pre-hospital providers. Article III – Purpose Section 1. The purpose of this organization is to: A. Advance and improve access and delivery of healthcare to patients of all ages in TSA M. B. Decrease morbidity and/or mortality which results from traumatic injury and medical emergencies (ie. stroke,AMI). C. Encourage activities designated to promote cooperation and resolve conflicts between member organizations. D. Coordinate funding streams for equipment, education, and programs to assist trauma and emergency care providers in TSA M. HOTRAC Regional Trauma System Plan Revised May 2010 Page 6 E. Maintain Trauma, Stroke, and Cardiac System Plans for HOTRACbased on standard guidelines for comprehensive system development. F. Improve public awareness of the methods of accessing the trauma care system, and preventing injury, stroke awareness, etc. G. Coordinate responses to mass casualty, evacuation, and disaster events. Article IV – RAC Membership Section 1. HOTRAC membership encompasses a wide range of professionals and citizens concerned about the health and well-being of the community as it relates to trauma, emergency services and disaster preparedness. Voting membership requires that the member represent a hospital or disaster service, an individual who is involved with trauma, emergency, or disaster care, an emergency medical service, an educational agency involved in training purposes for trauma, emergency, or disaster preparedness, or a service which provides care to victims of trauma, emergency, and/or disaster. A voting member must practice and/or reside within the boundaries of TSA M. Section 2. Condition of Membership A. A member entity must complete a Member Information Form. B. A member who resigns in good standing may reapply for membership. Resignations must be submitted in writing to the Board of Directors via the Executive Director. C. A member failing to actively participate in HOTRAC activities as defined by by-laws may be removed from the membership by a majority vote of the Board of Directors. Said member may appeal this action for re-instatement to the General Assembly. If re-instatement is approved by two-thirds of voting entities present at the General Assembly, the issue causing removal must be remedied prior to full reinstatement. D. Prior to removal from the membership by the Board of Directors, the Executive Director will notify said member that they are not compliant with HOTRAC bylaws and participation requirements. If participation does not increase, a certified letter will be sent to that member organization at the last known mailing address. If the issue continues, the Executive Director will bring said member’s name to the Board of Directors for removal. Section 3. Member entities will be allowed one vote at the General Assembly meetings. The vote may only be cast by one of the three persons listed on the entity’s Membership Form. Section 4. Members are listed in Appendix A. HOTRAC Regional Trauma System Plan Revised May 2010 Page 7 Section 5. A. Active Participation in the RAC is defined as the following: EMS Provider Agencies 1. 2. 3. 4. 5. 6. 7. B. Hospital Members 1. 2. 3. 4. 5. 6. 7. 8. 9. C. Will have representation at 75% of General Assembly Meetings. Will participate in a minimum of one (1) standing committee and will have representation at 75% of that committee meetings. Will submit information into the Trauma Registry and attend any meeting when the agency has a referral on the agenda. Will demonstrate participation in at least one HOTRAC sanctioned prevention activity annually and submit documentation of such. Will submit required Performance Improvement data upon request. Will have physician representation at 75% of the Physician Advisory Committee meetings. Will participate in one community disaster preparedness drill per year. Will have representation at 75% of General Assembly Meetings. Will participate in a minimum of one (1) standing committee and will have representation at 75% of that committee meetings. If applicable, will have Trauma Coordinator attend at least 75% of the Hospital Care & Management Committee as well as participate in the Trauma System Plan development. If applicable, will have Stroke Coordinator attend at least 75% of the Stroke Committee as well as participate in the Stroke System Plan development. Will have physician representation at 75% of Physician Advisory Committee Meetings. Will demonstrate participation in at least one HOTRAC sanctioned prevention activity annually and submit documentation of such. Will submit information into the Trauma Registry and attend any meeting when the agency has a referral on the agenda. Will participate in 75% of scheduled preparedness activities. In the event of emergency healthcare activations, will participate as required by the Health & Medical Annex of the County Emergency Operations Plans and/or the Health & Medical Appendix of the Regional Response Plan. Non-EMS/Hospital Entities 1. 2. 3. Will have representation at 75% of General Assembly Meetings. Will participate in a minimum of one (1) standing committee and will have representation at 75% of that committee meetings. Will participate in at least one (1) scheduled regional preparedness activity. Meeting attendance may be met in person, via conference call, or via webinar. D. Each member entity will complete an annual Regional Needs Assessment by the 1st of March of each year. E. Membership Dues must be paid in full by each member by the 1 st of March of each year. Membership dues is charged as follows: Hospitals - $500.00 HOTRAC Regional Trauma System Plan Revised May 2010 Page 8 9-1-1 EMS Providers (including Air Medical) - $250.00 Other Members (i.e., FROs, Emergency Management, etc.) - $50.00 Individuals - $25.00 F. Exceptions to the above requirements may be considered by the Board on an individual basis. An entity seeking such an exception must submit, in writing, a request for the exception and provide documentation to support the request. Article V – The Board of Directors Section 1. The Board of Directors shall consist of the following: Executive Committee 5. 6. 7. 8. Chair Vice Chair Secretary Treasurer Other Members 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. Immediate Past Chair Hillcrest representative Providence representative Rural Hospital representative Primary EMS agency for City of Waco representative Rural EMS representative FRO representative Emergency Management Member-at-Large Physician-at-Large Community Member-at-Large Employees (including the Executive Director) of the HOTRAC may not serve as a member of the Board of Directors. Section 2. Quorum: A quorum will be established by the presence of two-thirds of the board members in person or by video teleconference and must include at least one (1) Executive Committee member. An alternate representative (as defined in Section 4) will not count towards the constitution of a quorum. Section 3. Meetings (to include face-to-face, audio or video conference calls, and webinars): The Board of Directors shall be held monthly. Additional meetings will be scheduled as needed. The Chair may call a special meeting at any time with a 72 hour advance notice to the Board of Directors. This notice may be sent by the Chair or the Executive Director electronically. A quorum is required for a special called meeting. HOTRAC Regional Trauma System Plan Revised May 2010 Page 9 Section 4. Attendance: Board Members must attend at least 75% of the Board meetings per year. An alternate representative may be designated to attend a Board meeting by the member. Alternate representatives may not cast that entity’s vote and may not attend more than 25% of the scheduled board meetings. Section 5. Resignation/Succession In the event that the Chairperson resigns or is removed from office prior to the term expiration, the Vice Chair will immediately succeed the resigned/removed Chair. A Board Member who does not comply with assigned responsibilities may be relieved of office by a majority vote of the Board. Appointment of a replacement shall be made by the Chair with a majority vote of the Board present at the meeting. Any vacancies shall be filled for the balance of the unexpired term by the Chair with a majority vote of the Board or be deferred to the General Assembly for decision. The Board Member who serves the unexpired term will be eligible for reappointment twice. Section 6. Elections: All Board Members shall serve 2-year terms. Elections shall be held in November or December of each calendar year. Terms shall begin January 1 st of the following year. The Executive Committee will rotate on and off as follows: A. The Chair and Secretary positions will be elected in even numbered years. B. The Vice-Chair and Treasurer positions will be elected in odd numbered years. C. Election of Board members will be done by roll call at General Assembly Nominations for all open board positions can be submitted to the Executive Director beginning thirty (30) days prior to the November/December General Assembly. Additional nominations will also be accepted from the floor the night of the elections. Section 7. The Board of Directors shall be empowered to employ personnel to conduct the business of the HOTRAC. Section 8. HOTRAC Regional Trauma System Plan Revised May 2010 Page 10 The Board shall establish a Budget & Finance Committee. The Treasurer will serve as Chair of the Budget & Finance Committee. Section 9. The Board of Directors shall develop and maintain policy statements that guide the functioning of the HOTRAC. A policy shall receive final approval of the Board with a majority vote of those members present. Copies of such policy statements shall be provided to the General Assembly upon final approval of the Board of Directors at the following General Assembly meeting. Article VI – Duties of Board Members (listed but not limited to) Section 1. Section 2. Section 3. Executive Committee Prepares & performs Executive Director’s evaluation at least annually (with input of Board) Monitors credit card expenditures Develops and reviews policies to present to the Board Serves as the Committee for the Executive Director to take personnel issues Serves as employee dispute arbitration Approves grant application submission (Board would continue to approve contracts for signature) Is responsible for interviewing an Executive Director when needed Board of Directors: Defines “active participation” of membership Determines removal of RAC membership status Reviews and accepts resignations of membership Recommends & approves items for Executive Director’s evaluation Accepts proposed bylaw revisions from membership Serves as Fund Raising Committee Reviews the Articles of Incorporation for any changes Initiates bylaw changes as necessary Is responsible for choosing an Executive Director when needed The Chair shall: Preside at all meetings of the General Assembly, Board of Directors, and any special meetings. Facilitate development and achievement of organizational goals. Make interim appointments as needed with the approval of the Board of Directors. Sign all contracts, agreements, and other legal documents as needed after approval of the Board of Directors. Represent this organization at the Texas Department of State Health Services RAC Chair’s Meeting or identifies a designee. HOTRAC Regional Trauma System Plan Revised May 2010 Page 11 Section 4. Section 5. Section 6. The Vice Chair shall: Preside over HOTRAC activities in the absence of the Chair. Perform duties as assigned by the Chair. Assist in preparing any necessary reports or documentation required. The Secretary shall: Present the minutes of all proceedings of the Board and General Assembly meetings. Handle all correspondence of the organization in the absence of the Executive Director. Assist in preparing any necessary reports or documentation required. The Treasurer shall: Review and certify all financial business conducted by the HOTRAC including bank reconciliation. Perform financial duties in the absence of the Executive Director. Serve as Chair of the Board Budget and Finance Committee. Assist in preparing any necessary reports or documentation required. Article VII – Duties of the Executive Director Section 1. The Executive Director shall: Maintain a record of all financial business conducted by the HOTRAC in accordance with HOTRAC polices/procedures and common accounting practice. Prepare and submit financial reports to the Board and General Assembly at each of their meetings, respectively. Ensure that Board of Directors & General Assembly meeting minutes are made available to all RAC membership and the Department of State Health Services EMS & Trauma Systems Coordination as requested. Make available copies of bylaws and the Trauma System Plan annually as requested. Actively assist in seeking funding sources for the activities of the organization. Prepare necessary reports or documentation required by government agencies or grant sponsors. Gather information from the Committee Chairs and present to the Board Prepare and submit annual budget projections to the Board and General Assembly. Preside over meetings in which the Chair and Vice Chair are not available when a quorum is present. Article VIII – Standing and Ad Hoc Committees/Task Forces Section 1. The Committee Chairs shall: Organize and conduct meetings as defined in the bylaws. Facilitate the development and achievement of goals for their committee. Ensure that written agendas and minutes are provided to committee members. Provides the agendas, minutes, and sign-in sheets to the Executive Director for maintenance HOTRAC Regional Trauma System Plan Revised May 2010 Page 12 Section 2. A. Assist in preparing any necessary reports or documentation required. The Standing Committees and their missions are as follows: Pre-hospital Committee B. Hospital Care & Management Committee C. To serve as a liaison for pre-hospital providers within TSA M to include the monitoring of system development, coordination of activities, performance improvement, and pre-hospital training. To serve as a liaison between health care facilities within TSA M to include the monitoring of system development, coordination of activities, performance improvement, and hospital training. Physicians Advisory Committee (a quorum constitutes a majority of serving physicians) To monitor the performance of identified performance improvement indicators as it relates to the quality of patient care. Make recommendations regarding system enhancement and/or improvements. Inter-local liaison committees may be formed to provide comprehensive review of issues with greater local participation. Information/inquiries may be originated at either the Physicians Advisory Committee or the other committees. These meetings are closed since this committee is acting as the HOTRAC’s Quality Improvement Committee. D. Education/Injury Prevention Committee To provide guidance for training within the Region to enhance trauma care standards in this Region. To provide guidance within the Region for injury prevention activities. E. Emergency Preparedness & Response Committee To coordinate preparedness and responses to acute medical mass casualty, evacuation, and disaster situations. F. Stroke Committee a. To serve as a liaison to the acute care facilities and pre-hospital providers for initiatives issued by the State of Texas to include but not limited to stroke care, facility designations, public education, and training. G. Pediatric Committee To serve as a liaison to the acute care facilities and pre-hospital providers for initiatives issued by the State of Texas to include but not limited to pediatric emergency care. HOTRAC Regional Trauma System Plan Revised May 2010 Page 13 To provide oversight and guidance for the Region regarding the Pediatric Objectives issued by the State of Texas. H. Cardiac Committee Section 3. To serve as a liaison to the acute care facilities and pre-hospital providers for initiatives issued by the State of Texas to include but not limited to cardiac care, STEMI, public education, and training. Election of Committee Chairs and Vice Chairs Each standing committee shall have an identified Chair and Vice Chair which will be selected by the membership of that committee each year. This process will occur in November/December of each year in conjunction with the election of open positions on the Board of Directors. A. Each entity present will only have one vote. B. Nominated individuals must leave the room during the voting process. Section 4. Each standing committee shall have at least 4 meetings per year and keep minutes of each meeting. Meeting minutes may be obtained by any HOTRAC member from the Executive Director. The minutes may be provided either in hard copy or electronically. Section 5. Each Standing Committee shall have a standing agenda item for Emergency Healthcare System Issues. Section 6. Ad Hoc Committees/Task Forces may be established and/or dissolved at the discretion of the Board. Ad Hoc Committees/Task Forces are utilized to address issues that are limited in duration or cyclic in nature. Article IX – General Assembly Meetings Section 1. Quorum At least five (5) hospitals and six (6) EMS providers must be represented in addition to the one (1) Executive Committee member and three (3) Board of Directors to constitute a quorum for a General Assembly meeting. Section 2. Meetings The General Assembly shall meet at least four (4) times per year on the Thursday following the Governor’s EMS & Trauma Advisory Council (GETAC) meetings. When the General Assembly meeting falls on a federal holiday, the meeting will be held the following Thursday. HOTRAC Regional Trauma System Plan Revised May 2010 Page 14 Any member of the Executive Committee or the Executive Director may call a special meeting with a majority vote of the Board of Directors. A minimum of a two (2) week notice will be provided electronically to all members on the General Assembly email list serve. Section 3. Attendance See Article IV, Section 5 for the attendance requirements. Article X – Funding Section 1. State mandated funds shall be allocated according to contract received by HOTRAC from the Department of State Health Services. Any entity eligible according to State guidance must be classified as an active participant as stated in Article IV, Section 5, in order to receive any funding. Section 2. Any grant funds received by the HOTRAC will be made available to those only member entities that are active participants in HOTRAC as stated in Article IV, Section 5, in order to receive any funding. Section 3. Any member entity receiving funds through and/or from HOTRAC must provide required reports, support documents, etc. as stated at the time the funds are received by the member entity. Failure to comply will result in ineligibility of funding through and/or from HOTRAC for a period of not less than one (1) fiscal year funding cycle. Section 4. Failure to comply with Article IV, Section 5 shall cause a member entity to become ineligible for funding through and/or from HOTRAC for a period of not less than six (6) months and not more than twelve (12) months. Section 5. All grant funds shall be considered “restricted”. “Restricted funds” are defined as those funds that must be utilized as provided in a fully executed contract, grant application and/or award notice, or directed donation. Any funds received that have not been “restricted” shall be considered “unrestricted” and may be utilized for any type of expenditure. “Unrestricted funds” shall include but not limited to dues, donations, etc. Article XI - Finance and Fiscal Responsibility Standards Section 1. The Heart of Texas Regional Advisory Council’s fiscal and operational years shall follow the calendar year. HOTRAC Regional Trauma System Plan Revised May 2010 Page 15 Section 2. Budget preparation is achieved through needs assessments provided by the HOTRAC committees as well as strategic direction provided by the Board. The Budget will be completed by the Executive Director and the Board Budget and Finance Committee then presented for ratification at the November General Assembly meeting. Section 3. All Checks must have two signatures. These signatures may be any combination of the Chair, Vice Chair, Secretary, Executive Director, and one additional Board member to be determined by a majority vote of the Board. The HOTRAC will maintain a minimum of two (2) checking accounts (“restricted” & “unrestricted”) and may establish additional accounts as needed with approval of the Board of Directors. Section 4. Approval of expenditures must conform to the following schedule: Amount Approval Required A. $ 0 - $ 10,000.00 Executive Committee B. $ 10,000.01 – 100,000.00 Board only C. $ 100,000.01 or more General Assembly Any purchases and/or leases of real property, land, buildings, and vehicles shall be approved by a majority vote of the General Assembly present at the meeting. Section 5. The Executive Director shall have the authority to establish charge accounts with advance approval the Board of Directors. The Executive Director shall have authority to maintain and utilize HOTRAC’s secured credit card with a limit not to exceed $ 5,000.00 (five thousand dollars). A report must be provided upon request of the Executive Committee. A report shall be provided to the Board and General Assembly as a part of the financial statements. Section 6. The Executive Director may authorize expenditures associated with a specific grant if a budget was submitted as part of the grant application process and the grant application was approved by the Board of Directors upon completion or at notice of award. Section 7. Distribution of funds will be in accordance with State and Federal regulations. HOTRAC Regional Trauma System Plan Revised May 2010 Page 16 Section 8. Annually an external audit shall be completed in accordance with State and Federal regulations. Article XII – Alternative Dispute Resolution (ADR) Process Section 1. A. Any provider or individual representing a provider, service, or hospital that has a dispute in connection with another provider or the HOTRAC itself (e.g., bylaws, trauma system plan, guidelines and protocols, etc.) may formally voice its disapproval in writing. The written document will be addressed by the Chair of the HOTRAC and/or the Executive Director. B. A formal protest must contain the following information: a specific statement of the situation that contains the description of each issue and a proposed solution to resolve the matter(s). C. A neutral or impartial group with no vested interest in the outcome of the dispute will be assembled to review the issue. This group may solicit written responses to the dispute from interested parties. If the dispute is not resolved by mutual agreement, the group will issue a written determination, within thirty (30) days of receipt of all pertinent data. D. Party or parties may appeal the determination by the group and ask that the issue be brought before the General Assembly for a final determination. The party or parties have no later than ten (10) working days after the determination to submit the request for secondary review. The secondary review will be limited to the original determination. The appeal must be mailed or hand-delivered in a timely manner. In the event the appeal is not timely in delivery, it will not be considered. If not considered, the party or parties will be notified in writing. The request must be submitted in writing to the following address: HOTRAC 405 Londonderry, Suite 201 Waco, TX 76712 Article XIII - Amendments Section 1. Bylaws Proposed amendments and revisions to the bylaws must be submitted to the Executive Director and approved by a majority vote of the Board of Directors in order for them to be submitted to the General assembly. All proposed bylaw revisions and/or changes will be submitted to the General Assembly Membership via United States Postal Service and/or electronically (30) days prior to action. The proposed bylaws will also be submitted to all individuals that participate in the HOTRAC email list-serve. A roll-call vote shall be taken and there must be an affirmative vote of two-thirds of the General Assembly present for the revisions to the bylaws to be ratified. HOTRAC Regional Trauma System Plan Revised May 2010 Page 17 The bylaws shall be reviewed/amended/revised at least once per calendar year. Section 2. Trauma System Plan The HOTRAC will maintain a Trauma System Plan Workgroup that will annually update the HOTRAC Regional Trauma System Plan. This Workgroup shall have membership from hospitals and pre-hospital providers and will be presided over by the Executive Director. The Trauma System Plan shall be provided to the Department of State Health Services (DSHS) EMS & Trauma Systems Coordination by November 1st of each year. The Plan shall be approved by the Physicians Advisory Committee, the Board of Directors, and General Assembly. A majority vote of Physicians Advisory Committee and a majority vote of the Board of Directors shall constitute approval of the Trauma System Plan. And a majority vote of the General Assembly members shall constitute their approval of the Trauma System Plan. Article XIV – Administrative Operations Section 1. Robert’s Rules of Order shall be used as a guide for all meetings administered by the HOTRAC. Section 2. HOTRAC members may obtain copies of financial records, 990s, audit findings, etc. from the Executive Director or Chair. A request must be submitted in writing. The request must include what items wish to be reviewed and when the member would like to schedule a time to review requested documents. Original documents may not be removed from the HOTRAC offices without written approval of the Chair and/or Executive Director. Some documents may not be available for copying. RAC Chair Date Executive Director Date HOTRAC Regional Trauma System Plan Revised May 2010 Page 18 APPENDIX A (of Bylaws) Members Members (those completing a Member Information Sheet and in good-standing) include but are not limited to: Air Evac Lifeteam Bellmead Fire Department Blum VFD Bosque County Emergency Management Bruceville-Eddy EMS First Responders Capital Ambulance CareFlite City of Waco Clifton VFD Crawford EMS, Inc. Dennis, Wayne DePaul Center ETMC-EMS East Lake Limestone VFD Elm Mott Fire/ Rescue Falls County Volunteer Firefighters Association Falls County Emergency Management Falls County EMS Falls Community Hospital & Clinic Fraley, Diane Goodall-Witcher Healthcare Foundation Groesbeck VFD HOTCOG Hill County ESD #2 Hill County Emergency Management Hill Regional Hospital Hillcrest Baptist Medical Center Hillsboro Fire & Rescue Hillsboro Office of Emergency Management Kosse VFD & First Responders Lake Mexia VFD Lake Whitney Medical Center EMS LifeStar Limestone Medical Center HOTRAC Regional Trauma System Plan Revised May 2010 Limestone Medical Center EMS Limestone County Emergency Management McLennan County McGregor Volunteer EMS Mart EMS, Inc. Mexia Fire/EMS Mexia State School North Bosque EMS PHI Air Med 6/STAT I Parkview Regional Hospital Prairie Hill VFD & First Responders Providence Health Center Rural Hill EMS Tarbet, Robert Tehuacana VFD Waco, City of West EMS West Lake Limestone VFD West Shore FRO/VFD Whitney VFD Page 19 TSA M – EMS PROVIDERS (Ground) CareFlite EMS Mark Kessler – Title Local Office Address City, State ZIP Phone Fax Geographic Service Area – Hill County with the exception of the Cities of Hillsboro, Whitney, Hubbard and Mt. Calm Level of Service – ALS/MICU Medical Director – Number of Vehicles Primary Radio Frequency Crawford EMS Marilyn Judy, President P.O. Box 341 Crawford, Texas 76638 (254) 486-2101 Fax – 486-2198 Dispatch – Through McGregor PD Geographic Service Area – Western corner of McLennan County – Approximately 250 square miles. Level of Service - BLS Medical Director – Dr. George Smith Number of Vehicles - 1 Primary Radio Frequency – 154.250 Falls EMS Jim Lyon - Owner 403 Bridge Marlin, TX 76661 (254) 883-5445 Fax – (254) 803-2320 Dispatch – (254) 803-3745 (non-emergency) Geographic Service Area – Falls County Level of Service – BLS w/ MICU capability Medical Director – Dr. Karlan Downing Number of Vehicles – 4 Primary Radio Frequency – UHF Hillsboro Fire Dept. & EMS Greg Markwardt, Operations Chief P.O. Box 568 Hillsboro, Texas 76645 (254) 582-2401 Fax – (254) 582-9155 Dispatch – (254) 582-2141(emergency number) or 911 Geographic Service Area – 6 miles in each direction from Hillsboro. HOTRAC Regional Trauma System Plan Revised May 2010 Page 20 Level of Service – BLS with ALS Medical Director – Dr. Richard Jackson Number of Vehicles – 2 Primary Radio Frequency – 154.325 (Receive) 155.950 (Transmit) ETMC – EMS Dale Yates – Regional Director 1501 Hogan Lane, Ste. H Waco, TX 76705 (254) 799-7718 Fax – (254) 799-2363 Dispatch (800) 255-2011 Geographical Service Area – mainly central McLennan County Level of Service – MICU Medical Director – Dr. William Moore Number of vehicles – 13 Primary Radio Frequency – 800 MHz Lake Whitney Medical Center EMS Jimmy Hoskins – Director 103 N. Colorado Street Whitney, Texas 76692 (254) 694-9706 Fax –(254) 694-9708 Dispatch – Through the 911 System. Geographic Service Area – City of Whitney Level of Service - BLS with MICU capabilities Medical Director – Dr. Richard Jackson Number of Vehicles - 3 Primary Radio Frequency – 155.340 Limestone Medical Center EMS Shelton Chapman - Director 701 McClintic Dr. Groesbeck, Texas 76642 (254) 729-3097 Fax – (254) 729-3532 Dispatch – Through 911 Service. Geographic Service Area – ½ mile north of Navasota River to FM 164 and from FM 114 to just this side of Mart (see map attached). Level of Service – BLS w/ MICU capabilities Medical Director – Dr. Mark Hoeschele Number of Vehicles - 3 Primary Radio Frequency – 154.160 McGregor EMS William Heath, President PO Box 237 McGregor, Texas 76657 HOTRAC Regional Trauma System Plan Revised May 2010 Page 21 (254) 840-2528 Fax – (254) 840-4362 Dispatch – 911 or by McGregor Police Dept. Geographic Service Area – 139.6 square miles Level of Service – BLS with MICU capability Medical Director – Dr. Jon Daniell Number of Vehicles - 2 Primary Radio Frequency – 154.250 Mart EMS Tonja Vogt P.O. Box 335 Mart, Texas 76664 (254) 876-3322 Fax – (254) 876-3332 Dispatch – 911 System Geographic Service Area - McLennan County, Limestone County and half of Falls County Level of Service - MICU Medical Director – Dr. Jon Daniell Number of Vehicles - 2 Primary Radio Frequency – 365.250 Mexia Fire Dept & EMS Mike Clements – EMS Director P.O. Box 207 Mexia, Texas 76667 (254) 562-4188 Fax – (254) 562-2569 Dispatch – Limestone S.O. dispatches county 911 Mexia Police Department dispatches city of Mexia 911 Mexia Fire Department dispatches itself after receiving calls from the above two agencies. Geographic Service Area – See map attached. Level of Service – BLS with MICU capabilities Medical Director – Dr. Yong Chin Number of Vehicles – 3 Ambulances Primary Radio Frequency – 154.205, PL 100 fire North Bosque EMS Linda Catena – EMS Director P.O. Box 119 Meridian, Texas 76665 (254) 435-2070 Fax – (254) 435-2560 Dispatch – Through the 911 System Geographic Service Area – Approximately 1000 square miles Level of Service – BLS with MICU capabilities Medical Director – Dr. Kevin Blanton Number of Vehicles – 3 Ambulances; 2 reserve Primary Radio Frequency – 155.250 HOTRAC Regional Trauma System Plan Revised May 2010 Page 22 Rural Hill EMS Vicki Roberts – EMS Director PO Box 363 Hubbard, TX 76648 (254) 576-1543 Fax – (254) Dispatch – Hill County Sherriff’s Office Geographic Service Area – City of Hubbard & southeast Hill County Level of Service – BLS with some ALS Medical Director – Dr. William Mitchell Number of Vehicles – 3 Primary Radio Frequency – Scott & White EMS Charles Pearson 2401 S. 31st Street Temple, TX 76508 (254) 724-8080 Fax – (254) 724-0019 Dispatch – Geographical Service Area – Cities of Bruceville-Eddy & Moody Level of Service – BLS with MICU capabilities Medical Director – Dr. Robert Greenberg Number of vehicles- 16 (total) Primary Radio Frequency West Volunteer Ambulance Service Tom Marek – Supervisor P.O. Box 461 West, Texas 76691 (254) 826-3779 Fax – (254) 826-3231 Dispatch – (254) 826-3778 Geographic Service Area – From Abbott to Gholson and as far out as Ross Road – They also assist ETMC –EMS when needed in the Waco area. Level of Service – BLS with MICU capabilities Medical Director – Dr. George Smith Number of Vehicles - 3 Primary Radio Frequency – 155.295 HOTRAC Regional Trauma System Plan Revised May 2010 Page 23 TSA M – AIR MEDICAL PROVIDERS Air Evac LifeTeam – West (AEL 51) Steven Clinkscales, Regional Manager Cell (417) 293-2626 Base – (254) 826-0521 Fax – Dispatch – Geographic Service Area – see attached map Level of Service - MICU Medical Director – Dr. Brian Price Primary Radio Frequency – Air Evac LifeTeam – Fairfield (AEL 53) Steven Clinkscales, Regional Manager Cell (417) 293-2626 Base Fax – Dispatch – Geographic Service Area – see attached map Level of Service - MICU Medical Director – Dr. Brian Price Primary Radio Frequency – Air Evac LifeTeam – Ennis (AEL 74) Steven Clinkscales, Regional Manager Cell (417) 293-2626 Base Fax – Dispatch – Geographic Service Area – see attached map Level of Service - MICU Medical Director – Dr. Brian Price Primary Radio Frequency – Air Evac LifeTeam - Glenrose (AEL 69) Martha Nichols, Base Manager Cell – (417) 274-8722 Base – (254) 897-2691 Fax – (254) 897-2693 Dispatch – 800-568-6806 Geographic Service Area – see attached map Level of Service - MICU Medical Director – Dr. Robert Genzel Primary Radio Frequency – HOTRAC Regional Trauma System Plan Revised May 2010 CareFlite Base Fax – Dispatch – Geographic Service Area – see attached map Level of Service - MICU Medical Director – Dr. Primary Radio Frequency – PHI STAT Air 1 – Killen Skylark Field Brittany Misercola, Business Relations Supervisor Base - (254) 680-3644 Fax – (254) 680-3573 Dispatch – 800-456-7477 Geographic Service Area – see attached map Level of Service - MICU Medical Director – Dr. Primary Radio Frequency – PHI STAT Air 2 – Georgetown Traci Forister, Business Relations Supervisor Base (512) Fax – Dispatch – 800-456-7477 Geographic Service Area – see attached map Level of Service - MICU Medical Director – Dr. Primary Radio Frequency – PHI Air Medical 6 – Corsicana Dawn Traylor Base (903) Fax – Dispatch – 877-435-9744 Geographic Service Area – see attached map Level of Service - MICU Medical Director – Dr. Roy Yamada Primary Radio Frequency – PHI Air Medical 12 – Bryan Billy Rice, Base Supervisor Base (936) Fax – Dispatch – Geographic Service Area – see attached map Level of Service - MICU Medical Director – Dr. Primary Radio FrequencyPage 24 Air Evac LifeTeam – 51 (West) HOTRAC Regional Trauma System Plan Revised May 2010 Page 25 Air Evac LifeTeam – 53 (Fairfield) HOTRAC Regional Trauma System Plan Revised May 2010 Page 26 Air Evac LifeTeam – 74 (Ennis) HOTRAC Regional Trauma System Plan Revised May 2010 Page 27 Air Evac LifeTeam – 69 (Glen Rose) HOTRAC Regional Trauma System Plan Revised May 2010 Page 28 PHI STAT Air 1 (Killeen Skylark Airfield) *divide the air miles by 2 for approximate ETA in minutes (i.e., 30 miles = 15 min ETA). HOTRAC Regional Trauma System Plan Revised May 2010 Page 29 PHI STAT Air 2 (Georgetown) *divide the air miles by 2 for approximate ETA in minutes (i.e., 30 miles = 15 min ETA). HOTRAC Regional Trauma System Plan Revised May 2010 Page 30 PHI Air Medical 6 (Corsicana) *divide the air miles by 2 for approximate ETA in minutes (i.e., 30 miles = 15 min ETA). HOTRAC Regional Trauma System Plan Revised May 2010 Page 31 PHI Air Medical 12 (Bryan) *divide the air miles by 2 for approximate ETA in minutes (i.e., 30 miles = 15 min ETA). HOTRAC Regional Trauma System Plan Revised May 2010 Page 32 Heart of Texas Regional Advisory Council – TSA M TSA-M Hospital Facilities Facility DePaul Center (254) 776-5970 Fax: (254) 751-4769 ATTN: Kent Keahey Falls Community Hospital (254) 803-3561 Fax: (254)883-6066 Goodall-Witcher Healthcare Foundation (254) 675-8322 FAX- (254) 675-2246 Hill Regional Hospital (254) 582-8500 FAX- (254) 582-2144 Hillcrest Baptist Medical Center (254) 202-5300 FAX-(254) 202-8879 Lake Whitney Medical Center (254) 694-3165 FAX-(254) 694-3299 Limestone Medical Center (254) 729-3281 FAX-(254) 729-3080 Parkview Regional Hospital (254) 562-5332 FAX-(254) 562-9279 Location 301 Londonderry Drive Waco, TX 76712 McLennan County 60 beds PO Box 60 Marlin, TX 76661 Falls County 44 beds PO Box 549 101 South Ave. T Clifton, TX 76634 Bosque County 40 Beds 101 Circle Drive Hillsboro, Texas 76645 Hill County 92 Beds 100 Hillcrest Medical Blvd McLennan County 237 Beds PO Box 458 Whitney, Texas 76692 Hill County 49 Beds 701 McClintic Groesbeck, TX 76642 Limestone County 20 Beds 600 S Bonham Mexia, Texas 76667 Limestone County 59 Beds Providence Health Center (254) 751-4000 Fax: (254) 751-4769 ATTN: Kent Keahey 6901 Medical Parkway Waco, TX 76712 McLennan County 230 beds Waco VA (254) 752-6581 Fax – (254) 756-5215 4800 Memorial Drive Waco, TX 76711 McLennan County 346 beds HOTRAC Regional Trauma System Plan Revised May 2010 AVERAGE DAILY CENSUS HOSPITAL-BASED EMS SERVICE Trauma MEDICAL DIRECTOR ED MEDICAL DIRECTOR Administrator DESIGNATION Status Trauma Coordinator 20 No N/A N/A Kent Keahey President & CEO N/A N/A 15-20 No Dr. Dileep Bhateley Dr. Dileep Bhateley Willis Reese CEO Designated Level IV Tammy Samford, RN 12 No Dr. Kevin Blanton Dr. Kevin Blanton Clarence Fields President & CEO Designated Level IV Casandra Cox, RN, BSN 30 No Dr. Michael Charles Dr. Jeffrey Sterling Jan McClure CEO Designated Level IV Janice Markwardt, RN 160 No Dr. Ted Smith Dr. --- Glenn A. Robinson President & CEO Level II Trauma Center Lead Facility Lori Boyett, RN, BSN 10-15 Yes Dr. Aman Shah Dr. Aman Shah Ruth Ann Crow Administrator Non-designated N/A 10 Yes Dr James Wood Dr James Wood Penny Gray CEO Designated Level IV Temperance Johnson, RN 30 No Dr Jeremy Chester Dr Jeremy Chester Jimmy Stewart CEO Designated Level IV 175 No N/A Dr. John Hamilton Kent Keahey President & CEO Non-designated Eileen Bohannon, RN ED Director Not given No N/A N/A N/A N/A N/A Page 33 Marcy McFarland, RN System Participation All HOTRAC General Assembly meetings are open to any interested persons. Meeting notices and reminders are emailed to the membership well in advance of all meetings, and meeting notices are posted on the HOTRAC website. Minutes of all meetings are emailed and provided at each meeting, along with a meeting agenda. Active Participation in the RAC is defined as the following: A. EMS Provider Agencies 1. 2. 3. 4. 5. 6. 7. B. Hospital Members 1. 2. 3. 4. 5. 6. 7. 8. 9. C. Will have representation at 75% of General Assembly Meetings. Will participate in a minimum of one (1) standing committee and will have representation at 75% of that committee meetings. Will submit information into the Trauma Registry and attend any meeting when the agency has a referral on the agenda. Will demonstrate participation in at least one RAC sanctioned prevention activity annually and submit documentation of such. Will submit required Performance Improvement data upon request. Will have physician representation at 75% of the Physician Advisory Committee meetings. Will participate in one community disaster preparedness drill per year. Will have representation at 75% of General Assembly Meetings. Will participate in a minimum of one (1) standing committee and will have representation at 75% of that committee meetings. If applicable, will have Trauma Coordinator attend at least 75% of the Hospital Care & Management Committee as well as participate in the Trauma System Plan development. If applicable, will have Stroke Coordinator attend at least 75% of the Stroke Committee as well as participate in the Stroke System Plan development. Will have physician representation at 75% of Physician Advisory Committee Meetings. Will demonstrate participation in at least one RAC sanctioned prevention activity annually and submit documentation of such. Will submit information into the Trauma Registry and attend any meeting when the agency has a referral on the agenda. Will participate in 75% of scheduled preparedness activities. In the event of emergency healthcare activations, will participate as required by the Health & Medical Annex of the County Emergency Operations Plans and/or the Health & Medical Appendix of the Regional Response Plan. Non-EMS/Hospital Entities 1. 2. 3. Will have representation at 75% of General Assembly Meetings. Will participate in a minimum of one (1) standing committee and will have representation at 75% of that committee meetings. Will participate in at least one (1) scheduled regional preparedness activity. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 34 Meeting attendance may be met in person, via conference call, or via webinar. D. Each member entity will complete an annual Regional Needs Assessment by the 1st of March of each year. E. Membership Dues must be paid in full by each member by the 1 st of March of each year. Membership dues is charged as follows: Hospitals - $500.00 9-1-1 EMS Providers (including Air Medical) - $250.00 Other Members (i.e., FROs, Emergency Management, etc.) - $50.00 Individuals - $25.00 Participation from each organization is encouraged. The Bylaws are reviewed each year and revised as appropriate. Each component of the Regional Trauma Plan is presented, discussed, and approved by the HOTRAC General Assembly, Board of Directors, and Physicians Advisory Committee. All revisions are reviewed and approved through the same process. Once approved, complete copies of the Regional Trauma Plan will be distributed to the HOTRAC membership. System Access Goal The Goal for System Access within TSA-M is two-fold. First, rapid access to notification of the need for emergency and trauma care at any location within TSA-M must be available to all persons in the Region. Second, Emergency Medical Services (EMS) must be rapidly available to provide quality health care to injured or ill persons in each HOTRAC Community. In portions of this Region, First Responder Organizations (FRO) may provide initial treatment pending EMS arrival. Objectives 1. To ensure that all persons located in Trauma Service Area M will have the availability to access Emergency Dispatch for EMS services. 2. To ensure emergency healthcare providers have communication equipment available. 3. To strive to maintain an adequate number of First Responders and EMS providers that have the knowledge, skills, and equipment needed to provide emergency care to persons requesting assistance within the Region. Discussion The 9-1-1 communications system provides a dedicated phone line allowing direct routing of emergency calls through a telephone company central office to a Public Safety Answering Point (PSAP). Routing is based on the specific telephone exchange area rather than municipal boundaries. Enhanced 9-1-1 can include Automatic Number Identification (ANI) and/or Automatic Location Identification (ALI). Enhanced 9-1-1 also automatically routes emergency calls to a pre-selected answering point based upon the geographical location from which the call originated. Each of the five HOTRAC counties has enhanced 9-1-1 with ANI/ALI capability. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 35 The 9-1-1 Advisory Committee of the Heart of Texas Council of Governments is responsible for the development, performance evaluation, and administration of the 9-1-1 system in rural HOTRAC counties. Representatives from each county meet on a regular basis to discuss system problems, plan educational activities, and work cooperatively to develop and implement the 9-1-1 Strategic Plan. In McLennan County, the McLennan County 9-1-1 District provides the same services to the entire McLennan County area. There is free public access to 9-1-1 throughout TSA-M. Public education programs such as the Red E. Fox program are used to educate consumers. Training sessions are provided at Community Health Fairs, schools, Auxiliaries, hospitals, Sheriff’s departments, and EMS providers. Emergency Care providers for accessing emergency communications use a variety of methods, such as 800 MHz, VHF, and UHR frequencies. HOTRAC strives to ensure interoperable communications at all times. Communications Goal The Goal for Communications within TSA-M is to ensure communication capability between EMS providers, medical control, receiving facilities; and other First Responders entities. Rapid dispatch and notification of the need for emergency and trauma care at any location within TSA-M must be available to all persons in the region. Objectives 1. To facilitate regional communications, all EMS & First Responder Units as well as hospital emergency personnel will have a list of the communication devices & operating frequencies of the EMS and emergency care providers operating in the HOTRAC region. 2. To ensure that all EMS providers, First Responders, and hospital facilities in the HOTRAC region have functional communications equipment in order to communicate information related to the patient’s condition, the need for medical, EMS, or helicopter back-up, and to receive and communicate information related to patient care and disposition. 3. To ensure that emergency dispatch within the HOTRAC region is accomplished by persons who have the knowledge, skills, and equipment necessary to rapidly mobilize the appropriate level of emergency care to persons requesting assistance throughout the region. Discussion The communications network in TSA-M is comprised of UHF, VHF, and 800 MHz radio devices combined with telephone links, both cellular and base site. In some instances individual EMS providers utilize UHF, VHF, 800 MHz, and cellular phones to ensure communications capability. The use of multiple communications systems ensures regional communications are maintained between public and private EMS agencies, police, fire, and hospital entities. Dispatch - Emergency dispatch in each of the five HOTRAC counties is accomplished through various methods (i.e., sheriff’s office, local police department, or county 911 service). Many rural providers utilize alpha pagers to notify emergency personnel of dispatch communications. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 36 Pre-hospital Care Providers – Most of the EMS Providers utilize the VHF frequency while ETMC-EMS in McLennan County utilizes 800 MHz. Hospital Care Providers - All HOTRAC hospital facilities maintain communications capability with pre-hospital care providers through the use of UHF emergency radios, cellular phones, or standard phone lines. HOTRAC purchased each facility a HAM radio that is programmed as follows: HAM Radio Frequencies: CH Alpha/Numeric Out In Tone Location Type Service 0 W5BEC - ???? 147.140 147.740 123.0 Bell Amateur 1 W5BCR - Clifton 147.180 147.780 123.0 Bosque Amateur 2 KC5QHO - Comanche 146.680 146.080 110.9 Comanche Amateur 3 N5DDR - Gatesville 146.960 146.360 Coryell Amateur 4 WD5DDH - Waxahachie 145.410 144.810 Ellis Amateur 5 KB5TPP - Stephenville 147.360 147.960 110.9 Erath Amateur 6 WB5YJL - Fairfield 145.110 144.510 146.2 Freestone Amateur 7 WM5L - Hillsboro 146.780 146.180 123.0 Hill Amateur 8 WD5GIC - Granbury 147.080 147.680 110.9 Hood Amateur 9 KC5PGV - Cleburne 145.490 144.890 88.5 Johnson Amateur 10 W5ZMI - Mexia 145.390 144.790 146.2 Limestone Amateur 11 W5ZDN - Hewitt 146.890 146.290 123.0 McLennan Amateur 12 W5ZDN - Moody 145.150 144.550 123.0 McLennan Amateur 13 AA5RT - Waco 146.660 146.060 123.0 McLennan Amateur 14 W5ZDN - Waco 146.880 146.280 123.0 McLennan Amateur 15 WA5BU - Waco 147.160 147.760 McLennan Amateur 16 AA5RT - Waco 147.360 147.960 123.0 McLennan Amateur 17 N5DDC -Corsicana 145.290 144.690 146.2 Navarro Amateur 18 WD5GND - Glen Rose 145.270 144.670 110.9 Somervell Amateur 19 WD5GIC - Glen Rose 147.020 147.620 110.9 Somervell Amateur 25 Simplex Point to Point 146.400 Amateur 26 Simplex Point to Point 146.410 Amateur 27 Simplex Point to Point 146.420 Amateur 28 Simplex Point to Point 146.430 Amateur 29 Simplex Point to Point 146.440 Amateur 30 Simplex Point to Point 146.450 Amateur 31 Simplex Point to Point 146.460 Amateur 32 Simplex Point to Point 146.470 Amateur 33 Simplex Point to Point 147.480 Amateur 34 Simplex Point to Point 146.490 Amateur 35 Simplex Point to Point 146.500 Amateur 36 Simplex Point to Point 146.510 Amateur 37 National Calling Frequency 146.520 Amateur 38 Simplex Point to Point 146.530 Amateur 20 24 HOTRAC Regional EMS Guidelines Rev. 5.10 Page 37 39 Simplex Point to Point 146.540 Amateur 40 Simplex Point to Point 146.550 Amateur 41 Simplex Point to Point 146.560 Amateur 42 Simplex Point to Point 146.570 Amateur 43 Simplex Point to Point 146.580 Amateur CH Alpha/Numeric Out In Tone Location Type Service 49 50 Simplex Point to Point 147.420 Amateur 51 Simplex Point to Point 147.430 Amateur 52 Simplex Point to Point 147.440 Amateur 53 Simplex Point to Point 147.450 Amateur 54 Simplex Point to Point 147.460 Amateur 55 Simplex Point to Point 147.470 Amateur 56 Simplex Point to Point 147.480 Amateur 57 Simplex Point to Point 147.490 Amateur 58 Simplex Point to Point 147.500 Amateur 59 Simplex Point to Point 147.510 Amateur 60 Simplex Point to Point 147.520 Amateur 61 Simplex Point to Point 147.530 Amateur 62 Simplex Point to Point 147.540 Amateur 63 Simplex Point to Point 147.550 Amateur 64 Simplex Point to Point 147.560 Amateur 65 Simplex Point to Point 147.570 Amateur 66 85 86 TX Fire 3 154.2950 NOTE: Receive only Public Service 87 TX Fire 2 154.2650 88 TX Fire 1 154.2800 89 TX Air 2 151.3850 90 TX Med 1 155.3400 Public Service 91 TX Law 3 155.4750 Public Service 92 TX Law 2 155.3700 Public Service 93 TX Law 1 154.9500 Public Service 94 Freestone EOC 155.7975 Public Service 95 Limestone EOC 155.9325 Public Service 96 Falls EOC 154.0025 Public Service 97 McLennan EOC 158.7750 Public Service 98 Hill EOC 155.6925 Public Service 99 Bosque EOC 155.8875 Public Service on Public Service Bands Public Service Public Service 127.3 Public Service HOTRAC is an active participant in the interoperability planning efforts being address by the Heart of Texas Regional Council of Governments. HOTRAC strives to remain at Level 4 interoperability. HOTRAC follows the HOTCOG Regional Communications Plan. Please see that specific plan for additional detailed information regarding communications in the Region. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 38 Regional Medical Oversight & Control Goal The goal for Regional Medical Control in TSA-M is multifaceted. - to ensure strong physician leadership and supervision for pre-hospital care providers in both on-line and off-line functions. - to secure medical involvement in regional planning and educational program development. - Provide for the development and implementation of regional guidelines and system plan components, as well as in systems evaluation. . Objectives 1. To evaluate regional trauma care from a systems perspective, under the direction of representatives of HOTRAC medical staff throughout the region. 2. To involve HOTRAC medical staff in all phases and at all levels of the leadership and planning activities of regional development. 3. To ensure appropriate medical oversight of all pre-hospital care providers through a Performance Improvement (PI) process and other administrative processes. 4. To identify and educate regional medical control resources, standardize treatment guidelines, and analyze accessibility of medical control resources. 5. To identify and educate HOTRAC EMS providers and sources of on-line and off-line medical control. Discussion The HOTRAC region includes both rural and urban hospital and emergency care providers with varying levels of medical capability. There is no single EMS medical director for EMS providers; however there is one EMS medical director for multiple EMS providers within each county. All EMS medical directors are members of the HOTRAC Physician Advisory Committee, which meets on a quarterly basis. Physician Involvement in Regional Plan Development - The Physician Advisory Committee meets on a quarterly basis to conduct its usual business and to review and approve regional planning components, policies, and guidelines related to medical care. Each EMS medical director, trauma surgeon, and physician from each HOTRAC hospital has representation on this standing committee. Any interested HOTRAC physician is invited to attend committee meetings. Medical Direction of Pre-hospital Care Providers - In accordance with DSHS guidelines, all HOTRAC prehospital care providers function under medical control. Regional EMS guidelines are printed and distributed to all EMS providers for incorporation into local protocols. (Please see the Appendix for ALS and BLS guidelines). Periodic reviews and updates are completed and upon approval are distributed as necessary. These guidelines serve as a baseline and individual Medical Directors may adapt for their local community. A tiered system of patient care based on severity of injury utilizes First Responder Organizations and EMS providers with varying level of capability to ensure the rapid assessment and initial care of the trauma patient and transport to the appropriate level of care. Off-line medical control guidelines direct EMS provider interventions. On-line medical control from the receiving HOTRAC facility is also utilized when the patient’s condition or scene conditions cannot be addressed by off-line protocols. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 39 Regional Performance Improvement - The Physician Advisory Committee meets quarterly to conduct its usual business and to carry out regional Performance Improvement activities. The Trauma Coordinators/ED Directors/EMS representatives meet in conjunction with the Physician Advisory Committee to review patient care and evaluate outcomes from a systems perspective. (Please see System PI section for more details). PI indicators include a review of all deaths, transfers out of region, and pediatric filters. (See forms) Hospitals and EMS Providers have separate PI indicator tools but many of the indicators are utilized for both areas. Pre-hospital Triage Goal Patients will be identified, rapidly and accurately assessed, and based on identification of their actual or potential for serious injury, will be transported to the nearest appropriate TSA-M trauma facility. Purpose In order to ensure the prompt availability of medical resources needed for optimal patient care, each patient will be assessed for the presence of abnormal vital signs, obvious anatomic injury, mechanism of injury, and concurrent disease/predisposing factors. Definition Trauma Patient—the patient is a victim of an external cause of injury that results in major or minor tissue damage or destruction caused by intentional or unintentional exposure to thermal, mechanical, electrical, or chemical energy, or by asphyxia, submersion, or hypothermia. System Triage 1. Unless immediate stabilization (ABC’s, cardiac arrest, etc.) is required, patients in TSA-M with the following injuries, with significant mechanism of injury, should be taken directly to Hillcrest Baptist Medical Center or another appropriate trauma facility offering resources not available to Hillcrest Baptist Medical Center: Penetrating injuries to head, neck, and torso Respiratory Compromise/obstruction GCS less than 13 O2 sat less than 90% Adult Patients with a SBP less than 100 Child less than one year with SBP less than 70 or heart rate less than 100 or more than 190 Child 1-9 years with SBP less than 70 + 2 x age in years or heart rate less than 80 or more than 150 Suspected Amputation proximal to the wrist or ankle Suspected Two or more proximal long bone fractures (Femur, Humerus) Suspected Pelvic fractures Burns more than or equal to 20% BSA or more than 10% if under 6 years old HOTRAC Regional EMS Guidelines Rev. 5.10 Page 40 Temperature less than or equal to 95◦F Patients with traumatic paralysis 2. If ground transport time to Hillcrest Baptist Medical Center is greater than 30 minutes or if lifesaving interventions (e. g. airway stabilization, chest tube insertion, etc.) are required for safe transport, contact medical control and/or take the patient to the nearest medical facility and call for the helicopter transport to meet you at the closest agreed upon landing zone. Off-line Medical Control Trauma Triage Criteria Goal Patients will be identified, rapidly and accurately assessed, and based on identification of their actual or potential for serious injury, will be transported to the nearest appropriate TSA-M trauma facility where the patient can best receive definitive care. When on-line medical control is needed but unavailable, EMS personnel will proceed to the nearest appropriate Trauma facility without delay. CLASSIFICATION OF TRAUMA PATIENTS for PRE-HOSPITAL Patients in TSA-M are classified according to severity of injury in order to determine the medical resources which may be required. EMS personnel will triage and transport trauma patients in TSA-M according to the following guidelines: Category 1. Trauma Patients with the most severe injuries are classified as Category 1 patients. Patients with the following problems are included in this category and will require the medical resources available at a TSA-M Level II Trauma Facility. When EMS personnel are unable to establish on-line medical control, these patients should be transported directly to Hillcrest Baptist Medical Center (or another more appropriate Level I or Level II Trauma facility) unless the patient’s condition requires resuscitation and stabilization at the nearest appropriate acute care facility. Gun Shot Wound to head, neck or torso Respiratory Compromise/obstruction GCS less than 8 O2 sat less than 85% Adult Patients with a SBP less than 90 Child less than one year with SBP less than 70 or heart rate less than 100 or more than 190 Child 1-9 years with SBP less than 70 + 2 x age in years or heart rate less than 80 or more than 150 Category 2. Trauma Patients with the serious injuries are classified as Category 2 patients. Patients with the following problems are included in this category and will require the medical resources available at a TSA-M Level II Trauma Facility. When EMS personnel are unable to establish on-line medical control, these patients should be transported directly to Hillcrest Baptist Medical Center (or HOTRAC Regional EMS Guidelines Rev. 5.10 Page 41 another more appropriate Level I or Level II Trauma facility) unless the patient’s condition requires resuscitation and stabilization at the nearest appropriate acute care facility. Penetrating injuries to head, neck, and torso (non-GSW) Suspected Amputation proximal to the wrist or ankle Suspected Two or more proximal long bone fractures (Femur, Humerus) Suspected Open fracture (humerus, femur, tibia) O2 sat less than 90% Suspected Pelvic fractures Burns more than or equal to 20% BSA or more than 10% if under 6 years old Temperature less than or equal to 95◦F GCS less than 13 Adult SBP 90-100 Heart rate more than 140 Patients with traumatic paralysis Category 3. Category 3 trauma patients are those with injuries not classified as Category 1 or Category 2. When EMS personnel are unable to establish on-line medical control, these patients should be transported directly to the nearest appropriate TSA-M trauma facility for physician evaluation. Level IV Trauma Facilities after stabilization should make the decision whether to transfer to the Level II Trauma Facility if the patient has any mechanism listed and one or any findings listed. Mechanism of Injury Motor Vehicle Collision - With ejection - High speed more than 40 mph - Unrestrained more than 20 mph - Death in same car - Extrication more than 20 minutes - Rollover MCC/ATV/Bike/Large animal - Separation of rider - Crash speed more than 20 mph Falls (greater than 10 feet or 2x child’s height if under 6 years old) Assault/child abuse Auto/Pedestrian Burns (partial or full thickness) Hanging/Immersion Crush injury (not hands or feet) Findings Head HOTRAC Regional EMS Guidelines Rev. 5.10 Page 42 - Suspected skull fracture - Documented LOC greater than 5 minutes Neurologic - GCS less than 14 - Focal deficit - Traumatic paresis Musculoskeletal - Suspected Femur fracture - Suspected Spine fracture - Suspected Pelvic fracture - Pulseless extremity Abdomen - Severe abdominal pain - Seat belt “abrasions” Burns - Suspected Inhalation injury - More than or equal to 5% or less than or equal to 20% BSA Chest - O2 sat less than 92% - Suspected Multiple (more than 2) rib fractures - Sub Q air - Suspected Pneumothorax/Hemothorax - Significant neck and/or chest “abrasions” Category 4. Category 4 trauma patients are those with injuries not classified as Category 1, 2, or 3. When EMS personnel are unable to establish on-line medical control, these patients should be transported directly to the nearest TSA-M acute care facility for physician evaluation. GCS less than 15 Falls (less than 10 feet or less than 2x child’s height if under 6 years old) Snakebites Injured diabetic patients taking insulin Injured pregnant patients not classified as 1, 2, or 3 Toxic substance at scene in contact with the patient Helicopter Activation Goal TSA-M regional air transport resources will be appropriately utilized in order to reduce delays in providing optimal trauma care for severely injured trauma patients. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 43 Decision Criteria 1. Helicopter activation/scene response should be considered when it can reduce transportation time for patients meeting the following criteria. Should there be any question whether or not to activate TSA-M regional air transport resources, on-line medical control should be consulted for the final decision. Penetrating injuries to head, neck, and torso Respiratory Compromise/obstruction GCS less than 13 O2 sat less than 90% Adult Patients with a SBP less than 100 Child less than one year with SBP less than 70 or heart rate less than 100 or more than 190 Child 1-9 years with SBP less than 70 + 2 x age in years or heart rate less than 80 or more than 150 Suspected Amputation proximal to the wrist or ankle Suspected Two or more proximal long bone fractures (Femur, Humerus) Suspected Open fracture (humerus, femur, tibia) Suspected Pelvic fractures Burns more than or equal to 20% BSA or more than 10% if under 6 years old Temperature less than or equal to 95◦F Patients with traumatic paralysis 2. Additionally helicopter activation/scene response should be considered when: o Patient extrication time will be prolonged (> 20 minutes). o Multiple patients on scene o Ejection from MVC 3. Patients being transported via helicopter should be taken to the nearest Level I or Level II Trauma Facility. Emergency Department Diversion Goal TSA-M trauma facilities will communicate “Emergency Department diversion” status promptly and clearly to regional EMS and trauma facilities through EMSystem in order to ensure that trauma patients are transported to the nearest appropriate alternate trauma system hospital. System Objectives 1. To ensure that trauma patients will be transported to the nearest appropriate TSA-M trauma facility. 2. To ensure that diversion of ambulance traffic will occur only by pre-arrangement. 3. To develop system guidelines for regional facility and trauma diversion status (see EMSystem guidelines and protocols): Situations which would require the facility to go on diversion HOTRAC Regional EMS Guidelines Rev. 5.10 Page 44 Notification/activation of facility diversion status Procedure for termination of diversion status 4. Each facility will develop a mass casualty plan. Facility plans will reference the appropriate use of TSAM disaster resources, if needed. 5. Regional trauma care problems associated with facility diversion will be assessed through the Physician Advisory Committee PI process. 6. All facilities and pre-hospital providers will use EMSystem to notify and track diversion statuses. Facility Bypass Goal Patients who have been assessed and determined to be medically unstable, unconscious, or at high risk of multiple and/or severe injuries (Category 1 and 2 patients) will be safely and rapidly transported to the Regional Trauma Center. Category 3 patients will be safely and rapidly transported to the nearest appropriate trauma facility within TSA M. Category 4 patients will be safely and transported to the nearest appropriate acute care facility within TSA M. Decision Criteria Regional transport guidelines ensure that patients who meet the triage criteria for activation of the TSA-M Regional Trauma System Plan will be transported directly to the nearest appropriate trauma facility rather than to the nearest hospital except under the following circumstances: 1. If unable to establish and/or maintain an adequate airway, or in the case of traumatic cardiac arrest, the patient should be taken to the nearest acute care facility for stabilization. 2. A Level III or Level IV trauma facility may be appropriate if the expected scene to Level II Trauma Center transport time is excessive (> 30 minutes) and there is a qualified physician available at the facility’s Emergency Department capable of delivering definitive care. 3. Medical Control may wish to order bypass in any of the above situations as appropriate, such as when a facility is unable to meet hospital resource criteria or when there are patients in need of specialty care. 4. If expected transport time to the nearest appropriate Trauma Center is excessive (> 30 minutes) or if a lengthy extrication time (> 20 minutes) is expected, medical control or the EMS crew on scene should consider activating air transportation resources. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 45 Note: Should there be any question regarding whether or not to bypass a facility, on-line medical control should be consulted for the final decision from the receiving facility. Facility Triage Criteria Goal The goal of establishing and implementing facility triage criteria in TSA-M is to ensure that all regional hospitals use standard definitions to classify trauma patients in order to ensure uniform patient reporting and facilitate inter-hospital transfer decisions. Objectives 1. To ensure that each trauma patient is identified, rapidly and accurately assessed, and based on identification and classification of their actual or potential for serious injury, transferred to the nearest appropriate TSA-M trauma facility. 2. To ensure the prompt availability of medical resources needed for optimal patient care at the receiving trauma facility. 3. To develop and implement a system of standardized trauma patient classification definitions. Discussion Trauma patients in TSA-M are assessed and classified by severity of injury. The classification of trauma patients is based on a standard definition of “the trauma patient” which is applied in a consistent manner in both the pre-hospital and hospital setting. The Trauma Patient - The definition of the trauma patient in TSA-M is derived from the American College of Trauma Surgeon’s definition of trauma. In TSA-M, the trauma patient is defined as one who is a victim of an external cause of injury that results in major or minor tissue damage or destruction caused by intentional or unintentional exposure to thermal, mechanical, electrical, or chemical energy, or by asphyxia, drowning, or hypothermia. Facility Triage Criteria - Trauma patients are assessed in the pre-hospital setting and transferred to the nearest appropriate trauma facility in accordance with the TSA-M Pre-hospital Trauma Triage Criteria. Upon admission to the hospital emergency department, trauma patients receive initial treatment and re-assessment of their condition. The severity of injury and classification of trauma patients in the initial treating emergency department determines the optimal level of trauma care needed. Inter-hospital transfer is initiated as appropriate according to TSA-M facility triage decision criteria. CLASSIFICATION OF TRAUMA PATIENTS for FACILITIES Patients in TSA-M are classified according to severity of injury in order to determine the medical resources which may be required. EMS personnel will triage and transport trauma patients in TSA-M according to the following guidelines: HOTRAC Regional EMS Guidelines Rev. 5.10 Page 46 Category 1. Trauma Patients with the most severe injuries are classified as Category 1 patients. Patients with the following problems are included in this category and will require the medical resources available at a TSA-M Level II Trauma Facility. When EMS personnel are unable to establish on-line medical control, these patients should be transported directly to Hillcrest Baptist Medical Center (or another appropriate Level I or Level II Trauma facility) unless the patient’s condition requires resuscitation and stabilization at the nearest appropriate acute care facility. Gun Shot Wound to head, neck or torso Respiratory Compromise/obstruction Trauma patient receiving blood or blood products GCS less than 8 O2 sat less than 85% Adult Patients with a SBP less than 100 Child less than one year with SBP less than 70 or heart rate less than 100 or more than 190 Child 1-9 years with SBP less than 70 + 2 x age in years or heart rate less than 80 or more than 150 Category 2. Trauma Patients with the serious injuries are classified as Category 2 patients. Patients with the following problems are included in this category and will require the medical resources available at a TSA-M Level II Trauma Facility. When EMS personnel are unable to establish on-line medical control, these patients should be transported directly to Hillcrest Baptist Medical Center (or another appropriate Level I or Level II Trauma facility) unless the patient’s condition requires resuscitation and stabilization at the nearest appropriate acute care facility. Penetrating injuries to head, neck, and torso (non-GSW) Amputation proximal to the wrist or ankle Two or more proximal long bone fractures (Femur, Humerus) Open fracture (humerus, femur, tibia) O2 sat less than 90% Pelvic fractures with displacement Burns more than or equal to 20% BSA or more than 10% if under 6 years old Temperature less than or equal to 95◦F GCS less than 13 Adult SBP 90-100 or heart rate more than 130 Patients with traumatic paralysis Injury to extremity with absence of a pulse Category 3. Category 3 trauma patients are those with injuries not classified as Category 1 or Category 2. When EMS personnel are unable to establish on-line medical control, these patients should be transported directly to the nearest appropriate TSA-M trauma facility for physician evaluation. Level IV Trauma Facilities after stabilization should make the decision whether to transfer to the Level II Trauma Facility if the patient has one or more mechanism listed and one or more positive finding. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 47 Mechanism of Injury Motor Vehicle Collision - With ejection - High speed more than 40 mph - Unrestrained more than 20 mph - Death in same car - Extrication more than 20 minutes MCC/ATV/Bike/Large animal - Separation of rider - Crash speed more than 20 mph Falls Assault/child abuse Auto/Pedestrian Burns (partial or full thickness) Hanging/Immersion Crush injury (not hands or feet) Positive Findings Head - Any skull fracture - Abnormal brain CT Neurologic - GCS less than 14 - Focal deficit - Traumatic paresis Musculoskeletal - Femur fracture - Spine fracture - Pelvic fracture without displacement Abdomen - Solid organ injury - Gross hematuria - Abnormal abdominal/pelvic CT Burns - Inhalation injury - More than or equal to 5% or less than 20% BSA Chest - O2 sat less than 92% - Multiple (more than 2) rib fractures - Sub Q air - Pneumothorax - Hemothorax HOTRAC Regional EMS Guidelines Rev. 5.10 Page 48 Category 4. Category 4 trauma patients are those with injuries not classified as Category 1, 2, or 3. When EMS personnel are unable to establish on-line medical control, these patients should be transported directly to the nearest TSA-M acute care facility for physician evaluation. GCS less than 15 Same heights falls Snakebites Injured diabetic patients taking insulin Injured pregnant patients less than 23 weeks that are not classified as 1, 2, or 3 Toxic substance at scene in contact with the patient Inter-Hospital Transfers Goal The goal for establishing and implementing inter-hospital transfer criteria in TSA-M is to ensure that those trauma patients requiring additional or specialized care and treatment beyond a facility’s capability are identified and transferred to an appropriate facility as soon as possible. Objectives 1. To ensure that all regional hospitals make transfer decisions based on standard definitions which classify trauma patients according to TSA-M facility triage criteria. 2. To identify trauma treatment and specialty facilities within and adjacent to TSA-M. 3. To establish treatment and stabilization criteria and time guidelines for TSA-M patient care facilities. Discussion Hillcrest Baptist Medical Center is the Lead Trauma Facility in TSA-M and accepts all Category 1, 2, and 3 transfer patients from any requesting TSA-M facility. A toll-free number has been established and distributed to all TSA-M emergency medical and hospital providers: Hillcrest Trauma Transfer Phone Line: 1 – 888 – 872 – 8626 Medical personnel calling this number receive an “automatic acceptance” for these trauma patients. The time guideline for trauma patient transfers in TSA-M is to transfer Category 1 & 2 trauma patients immediately to the TSA M Lead Level II Trauma Facility. Category 3 trauma patients should be initially transported to the closest trauma facility for stabilization. If admission is necessary, the patient should be transferred to the Lead Level II Trauma Facility within four (4) hours from the time the patient arrived at that facility. Category 4 trauma patients HOTRAC Regional EMS Guidelines Rev. 5.10 Page 49 should be transported to the closest acute care facility for treatment and can be admitted to that facility if necessary. These criterions (see attached Regional Trauma Alert Form) are monitored through the regional PI program. Identification of Trauma Patients & Trauma Transfers - Trauma patients and their treatment requirements for optimal care are identified in the TSA-M facility triage criteria and pre-hospital triage criteria. Written transfer agreements are available between all TSA-M hospital facilities, and hospital facilities in adjacent regions. Trauma patients with special needs may be transferred to the Lead Trauma Facility for assessment and initial treatment by the trauma team. When resources beyond its capability are needed, transfer to another trauma designated facility outside TSA M should be expedited. The TSA-M initial-receiving hospitals may also choose to transfer patients with special needs directly to these facilities, bypassing the Lead Level II Trauma Facility when appropriate. Below are lists of possible facilities that may be utilized outside TSA M: Baylor University Medical Center (Level I Trauma) – TSA E Children's Medical Center of Dallas (Level I Trauma/Pediatric) – TSA E John Peter Smith Hospital (Level I Trauma) – TSA E Parkland Health & Hospital System (Level I Trauma/Burn) – TSA E Scott and White Memorial Hospital (Level I Trauma/Pediatric) – TSA L Dell Children’s Medical Center of Central Texas (Level I Trauma/Pediatric) – TSA O Trauma Patient Transport - Trauma patients in TSA-M are transported according to patient need, availability of air transport resources, and environmental conditions. Ground transport via BLS, ALS, or MICU ground ambulance is available throughout the Region. Air Medical transport (fixed and roto wing) is also available in this Region. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 50 HOTRAC Regional EMS Guidelines Rev. 5.10 Page 51 HOTRAC Regional EMS Guidelines Rev. 5.10 Page 52 System Performance Improvement Goal The goals for system performance improvement in TSA-M are to establish a method for monitoring and evaluating system performance over time and to assess the impact of trauma system development on regional morbidity and mortality. Objectives 1. To ensure that all TSA-M hospital and pre-hospital care providers are uploading the essential trauma data set to the state trauma registry. 2. To identify regional trauma data filters which reflect the process and outcome of trauma care in TSA-M. 3. To provide a multidisciplinary forum for trauma surgeons and trauma care providers to evaluate trauma patient outcomes from a system perspective and to assure the optimal delivery of trauma care. 4. To facilitate the sharing of information, knowledge, and scientific data. 5. To provide a process for medical oversight of regional trauma and EMS operations. Discussion In order to assess the impact of regional trauma development, system performance must be monitored and evaluated from an outcomes perspective. A plan for the evaluation of operations is needed to determine if system development is meeting its stated goals. Direction - The direction for the development of a HOTRAC Regional Trauma PI program is derived from the Texas EMS Rules: Section 157.124 Regional EMS Trauma Systems: (3)(K) of the EMS Rules (effective 2/17/92) requires the development of a “performance management program that evaluates outcome from a system perspective”. Authority - The authority and responsibility for regional performance improvement rests with the Regional Advisory Council. This will be accomplished in a comprehensive, integrated manner through the work of the Physician Advisory, Hospital Care and Management, and Pre-hospital Care committees. Scope & Process - The Physician Advisory Committee with the Hospital Care and Management Committee serves as the oversight committee for regional performance improvement. Referrals for follow-up and feedback to & from the Pre-hospital Care Committee and providers ensure system-wide, multidisciplinary performance improvement. The Physicians Advisory Committee approves, with input from other committees, the type of data and manner of collection, set the agenda for the PI process within the regularly-scheduled quarterly meetings of the committee, and identify the events and indicators to be evaluated and monitored. Indicator identification will be based on high risk, high volume, and problem prone parameters. Indicators will be objective, measurable markers that reflect trauma resources, procedural/patient care techniques, and or systems/process outcomes. Occurrences will be evaluated from a system, outcomes prospective and sentinel events will be evaluated on a case by case basis. Activities and educational offerings will be presented to address knowledge deficits and HOTRAC Regional EMS Guidelines Rev. 5.10 Page 53 case presentations or other appropriate mediums will be designed to address systems and behavioral problems. All actions will focus on the opportunity to improve patient care and systems operation. The results from committee activities will be summarized and communicated to the RAC membership. Problems identified that require further action will be shared with the persons and entities involved, for follow-up and loop closure. Summary reports will be communicated on a standard format to the appropriate committee (see attached). The functions and effectiveness of HOTRAC performance improvement process will be evaluated on an annual basis in conjunction with the annual evaluation of the HOTRAC bylaws. All PI activities and committee proceedings are strictly confidential. Individuals involved in performance management activities will not be asked to review cases in which they are professionally involved, but will be given the opportunity to participate in the review process. Data Collection - PI data will be collected by the Trauma Coordinators, ED Directors, and 9-1-1 EMS Providers as well as from the state trauma registry when operational. Quarterly reports are submitted for each HOTRAC facility and 9-1-1 EMS Provider. Sentinel events will be used to focus attention on specific situations/occurrences of major significance to patient care outcomes. TSA-M providers upload the required data set directly to the state trauma registry. Confidentiality - All information and materials provided and/or presented during PI meetings are strictly confidential. See attached form. HOTRAC facility and 9-1-1 EMS Provider data related to the following PI indicators are reviewed during the quarterly Physician Advisory meetings. See attached PI forms. The PI Forms are reviewed and updated annually. Reporting Quarters. HOTRAC regional PI data-reporting quarters are as follows: First Quarter: Second Quarter: Third Quarter: Fourth quarter: Jan-Feb-Mar April-May-June July-August-Sep Oct-Nov-Dec HOTRAC Regional EMS Guidelines Rev. 5.10 Reporting at: Reporting at: Reporting at: Reporting at: May meeting August meeting November/December meeting February meeting Page 54 HOTRAC Regional EMS Guidelines Rev. 5.10 Page 55 HOTRAC Regional EMS Guidelines Rev. 5.10 Page 56 HOTRAC Regional EMS Guidelines Rev. 5.10 Page 57 HOTRAC Regional EMS Guidelines Rev. 5.10 Page 58 HOTRAC Regional Performance Improvement Statement of Confidentiality Medical Performance Improvement provides an objective mechanism to evaluate trauma and emergency care, facilitates the sharing of information, knowledge, and scientific data, and provides a forum for medical directors and other physicians to review the performance of the regional systems to assure the optimal delivery of trauma and emergency care. The direction of the committee comes from the Texas EMS Rules: Section 157.124 Regional EMS Trauma Systems: (3) (k) of the EMS Rules (effective 2/17/92) requires the development of a “performance management program that evaluates outcome from a system perspective” Committee members engaged in medical care review have protection from disclosure of proceedings, under Section 773.095 RECORDS OF PROCEEDINGS CONFIDENTIAL of the Texas Health and Safety Code as follows: (a) The proceedings and records of organized committees of hospitals, medical societies, emergency medical service providers, or first responder organizations relating to the review, evaluation, or improvement of an emergency medical services provider, a first responder organization, or emergency medical services personnel are confidential and not subject to disclosure by court subpoena or otherwise. (b) The records and proceedings may be used by the committee only in exercise of proper committee functions. (c) This section does not apply to records made or maintained in the regular course of business by an emergency medical services provider, a first responder organization, or emergency medical services personnel. Section 773.096 IMMUNITY FOR COMMITTEE MEMBERS “A member of an organized committee under Section 773.095 is not liable for damages to a person for an action taken or recommendation made within the scope of the functions of the committee if the committee member acts without malice and in the reasonable belief that the action or recommendation is warranted by the facts known to the committee member.” CONFIDENTIALITY As a participant in this HOTRAC regional performance improvement process, I understand and agree that all information and materials provided and/or presented during the meeting are strictly confidential. Meeting & Date: Physicians Advisory Meeting – HOTRAC Regional EMS Guidelines Rev. 5.10 Page 59 APPENDIX A HOTRAC Regional EMS Guidelines Rev. 5.10 Page 60 Treatment Guidelines These guidelines are valid October 1, 2009 Through December 31, 2013 Heart of Texas Regional Advisory Council (HOTRAC) Trauma Service Area M ____FOR HOTRAC Regional EMS Guidelines Rev. 5.10 EMS PROVIDERS _____ Page 61 TABLE OF CONTENTS INTRODUCTION ....................................................................................................................... 5 DEVELOPMENT AND AUTHORITY ........................................................................................ 5 OPERATIONAL POLICIES ...................................................................................................... 5 AUTHORIZATION TO PROVIDE PRE HOSPITAL CARE ...................................................... 5 Purpose ......................................................................................................................................5 Authorization ..............................................................................................................................5 To Obtain Authorization .............................................................................................................6 Deauthorization ..........................................................................................................................6 Geographic Limitations of Authorization ....................................................................................6 Authorization of Non-EMS Personnel ........................................................................................6 RESTRAINTS POLICY ............................................................................................................. 6 Safety Restraint Policy ...............................................................................................................6 Policy for Control of Violent Patients ..........................................................................................6 HELICOPTER ACTIVATION .................................................................................................... 7 Medical Patients .........................................................................................................................7 Trauma Patients .........................................................................................................................7 Decision Criteria .........................................................................................................................7 DESTINATION POLICY ........................................................................................................... 8 PRE-HOSPITAL TRAUMA TRIAGE ........................................................................................ 8 DNR CONDITIONS ................................................................................................................... 9 REFUSAL TO TRANSPORT .................................................................................................. 10 General Statement .................................................................................................................. 10 Procedure For Refusal ............................................................................................................ 11 SPINAL MOTION RESTRICTION GUIDELINES ................................................................... 11 Assessment Guidelines ........................................................................................................... 12 Short Board/KED Use ............................................................................................................. 12 AUTHORIZED MEDICATIONS .............................................................................................. 13 Adenosine ............................................................................................................................... 13 Albuterol .................................................................................................................................. 13 Amiodarone ............................................................................................................................. 13 Aspirin ..................................................................................................................................... 13 Atropine ................................................................................................................................... 14 Dextrose 5% ............................................................................................................................ 14 Dextrose 50% .......................................................................................................................... 14 Diazepam ................................................................................................................................ 14 Diltiazem .................................................................................................................................. 14 Diphenhydramine .................................................................................................................... 14 Dopamine ................................................................................................................................ 15 Epinephrine ............................................................................................................................. 15 Furosemide ............................................................................................................................. 15 Glucagon ................................................................................................................................. 16 Glucose, Instant ...................................................................................................................... 16 Labetalol .................................................................................................................................. 16 Lactated Ringers…………………………………………………………………………………….. 16 Lidocaine ................................................................................................................................. 16 Magnesium Sulfate.................................................................................................................. 17 Midazolam ............................................................................................................................... 18 Morphine Sulfate ..................................................................................................................... 18 Naloxone ................................................................................................................................. 18 Nitroglycerine .......................................................................................................................... 18 Norcuron .................................................................................................................................. 19 Normal Saline .......................................................................................................................... 19 Oxygen .................................................................................................................................... 19 HOTRAC Regional EMS Guidelines Rev. 5.10 Page 62 Promethazine .......................................................................................................................... 19 Succinylcholine........................................................................................................................ 20 Sodium Bicarbonate ................................................................................................................ 20 Terbutaline .............................................................................................................................. 20 Thiamine.................................................................................................................................. 20 PROCEDURES ....................................................................................................................... 21 Automatic External Defibrillator ............................................................................................... 22 Cricothyrotomy ........................................................................................................................ 23 Defibrillation/Cardioversion ..................................................................................................... 23 Drug Administration ................................................................................................................. 23 Esophageal Intubation with a Multilumen Airway.................................................................... 24 Intraosseous Infusion .............................................................................................................. 24 Musculoskeletal Motion Restriction ......................................................................................... 25 Nasotracheal Intubation .......................................................................................................... 26 Needle Chest Decompression ................................................................................................ 26 Orotracheal Intubation ............................................................................................................. 27 Pacing ..................................................................................................................................... 28 Peripheral Venipuncture .......................................................................................................... 29 Rapid Sequence Intubation ..................................................................................................... 30 Spinal Motion Restriction ........................................................................................................ 30 Wound Care ............................................................................................................................ 31 AIRWAY MANAGEMENT ...................................................................................................... 33 General Principles ................................................................................................................... 33 Airway Management Algorithm ............................................................................................... 34 Foreign Body Airway Obstruction ............................................................................................ 35 COMMUNICATIONS GUIDELINES ....................................................................................... 36 ABDOMINAL PAIN/NAUSEA AND VOMITING GUIDELINE ................................................ 37 ALLERGIC REACTION / ANAPHYLAXIS ............................................................................. 39 ALTERED LEVEL OF CONSCIOUSNESS ............................................................................ 40 General Considerations .......................................................................................................... 40 Seizure Activity ........................................................................................................................ 41 Syncope/Fainting..................................................................................................................... 42 With Neuro Signs .................................................................................................................... 43 SUSPECTED ACUTE MYOCARDIAL INFARCTION ............................................................ 44 BRADYCARDIA...................................................................................................................... 45 HYPERTENSIVE CRISIS………………………………………………… ................................... 46 HYPOTENSION/SHOCK…………………………………….. ................................................... 47 ECA/EMT - CARDIAC EMERGENCIES................................................................................. 48 Apneic & Pulseless.................................................................................................................. 48 Tachycardia - Unstable With Pulses ....................................................................................... 49 Tachycardia - Stable ............................................................................................................... 50 Tachycardia - Ventricular Fibrillation/Pulseless V. Tach (VF/VT) .......................................... 51 PARAMEDIC - CARDIAC EMERGENCIES ........................................................................... 52 Tachycardia ............................................................................................................................. 53 Cardiac Arrest - Ventricular Fibrillation/Pulseless V. Tach (VF/VT) ....................................... 54 Asystole ................................................................................................................................... 55 Pulseless Electrical Activity (PEA) .......................................................................................... 56 Post-Resuscitation .................................................................................................................. 57 RESPIRATORY DISTRESS MEDICAL .................................................................................. 58 General Considerations .......................................................................................................... 58 Asthma & COPD ..................................................................................................................... 59 Pulmonary Edema ................................................................................................................... 60 Suspected Epiglottitis .............................................................................................................. 61 VENTILATOR GUIDELINE (for AutoVent 2000/3000 Portable Ventilators)………….………..62 TASER REMOVAL GUIDELINE ............................................................................................ 63 SNAKEBITE............................................................................................................................ 64 HOTRAC Regional EMS Guidelines Rev. 5.10 Page 63 POISONING & OVERDOSE ................................................................................................... 65 INTOXICATION AND BEHAVIORAL EMERGENCIES ......................................................... 66 HYPERTHERMIA.................................................................................................................... 67 Heat Exhaustion ...................................................................................................................... 67 Heat Stroke ............................................................................................................................. 68 HYPOTHERMIA ...................................................................................................................... 69 OBSTETRICS ......................................................................................................................... 70 Normal Delivery & General Considerations ............................................................................ 70 Prolapsed Cord ....................................................................................................................... 71 Nuchal Cord ............................................................................................................................ 72 Breech Presentation ................................................................................................................ 73 PEDIATRIC NEWBORN RESUSCITATION .......................................................................... 74 OBSTETRICS/GYNECOLOGY .............................................................................................. 75 Vaginal Bleeding ..................................................................................................................... 75 TRAUMA ................................................................................................................................. 76 General Procedures ................................................................................................................ 76 Classification Of Trauma Patients ........................................................................................... 77 Category 1 Trauma ................................................................................................................. 77 Category 2 Trauma ................................................................................................................. 77 Category 3 Trauma ................................................................................................................. 77 Category 4 Trauma ................................................................................................................. 79 Head Injury & Spinal Trauma .................................................................................................. 80 Respiratory Distress With Chest Injury ................................................................................... 81 Abdominal Trauma .................................................................................................................. 82 Amputated Parts...................................................................................................................... 83 Isolated Fractures, Dislocations, & Sprains ............................................................................ 84 Burns ....................................................................................................................................... 85 Near Drowning ........................................................................................................................ 86 APPENDIX .............................................................................................................................. 87 EMS Patient Refusal Checklist (SAMPLE) ............................................................................. 88 Refusal of Care Information Sheet (SAMPLE) ........................................................................ 89 Pre-Hospital Thrombolytic Screen (SAMPLE) ........................................................................ 90 Pediatric & Neonatal Assessment ........................................................................................... 91 ChemPack Standard Delagation Order (SAMPLE) ................................................................ 92 Antidote Administration for ChemPack ................................................................................... 93 HOTRAC Regional EMS Guidelines Rev. 5.10 Page 64 INTRODUCTION These guidelines identify the procedures that may be performed in the field by EMS personnel. The off line medical control for EMS activities are not intended to supersede an emergency physician's prerogative to order treatment. The primary responsibility for the Emergency Care Provider at every level is to render prompt, efficient and proficient care to the ill and injured. The treatments and procedures listed are intended to be carried out without contact with medical control, unless the requirement to "Contact Medical Control" is part of the guideline. At any time that EMS personnel feel the need to clarify or obtain orders, they are encouraged to do so. The pre-hospital healthcare providers in our system have demonstrated an outstanding degree of competence and dedication to one of the toughest jobs imaginable. It is our hope that these guidelines will make their job easier. Development and Authority The Medical Director for each individual agency is responsible for the entire aspect of patient care, which is defined as from the time the call is received in dispatch until the patient arrives at the destination. The Texas State Board of Medical Examiners and the Medical Practice Act mandate this authority. The HOTRAC EMS Guidelines should serve as a basis for EMS agencies. HOTRAC EMS Guidelines will be reviewed as needed or at least every licensure cycle. The individual agency medical directors, clinical staff, and HOTRAC Staff are responsible for the review. An original signature page must be in the front of every Protocol/Standing Delegated Order manual. When singular changes are made they will be signed by the medical director and placed in each EMS Protocol book. These changes will be sent to the Texas Department of State Health Services. Operational Policies 1. 2. 3. 4. 5. 6. 7. History should not be obtained at the expense of delivering urgently needed care. Life-threatening problems noted in the primary survey must be adequately managed first. Trauma cardiac arrest is not treated by medical arrest standards. Trauma arrest patients require immediate transport with control of external hemorrhage, neck immobilization if indicated. IV's are to be established in route. Cardiac arrest drugs may be given if there is a history of heart disease. Orders received from physicians other than those providing Medical Control should be verified with on line Medical Control if they deviate from the protocols. If a licensed physician at the scene properly identifies himself and has established a physician-patient relationship, agrees to accept responsibility for the patient's care and agrees to accompany the patient to the hospital, EMS personnel may accept orders from that physician. A run report must be provided for Medical Control on all runs within 24 hours. If the patient's condition does not seem to fit a Protocol or Protocols, always contact Medical Control. If you are asked to perform a hospital-to-hospital transfer of an unstable patient, call Medical Control. Always maintain Universal Precautions body substance isolation, and personal safety. Authorization to Provide Pre Hospital Care Purpose To ensure that the Provider is in compliance with the Texas State Board of Medical Examiners rule number 197. To define “authorization” to function as Pre-hospital Care Providers within the Medical Control System To ensure that each individual knows the requirements pertaining to obtaining and maintaining authorization Authorization Authorization is separate from certification. Every provider must have a current certification. The Medical Director is responsible for granting authorization. Authorization is required to provide pre-hospital or out-of-hospital care to any patient within the HOTRAC Region. Certification level does not necessarily dictate authorization level. The Medical Director may authorize any provider to function at any level as per DSHS Rule 157. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 65 At no time may any provider provide pre-arrival instructions without prior approval of the Medical Director. This includes personnel at any and all levels. To Obtain Authorization Prior to allowing any provider to function in a patient care delivery or dispatch role, the service shall notify the Medical Director or designee and provide the following information: o The individual’s name, date of birth, address, social security number, and home phone number o The position for which the individual is applying o A copy of the most current DSHS certification o The copy must clearly show the applicant’s name, certification number, and expiration date. o EMT-Paramedic applicants shall also provide legible copies with signatures and expiration or date of course for the following: Advanced Cardiac Life Support (ACLS) course completion card from a nationally accredited program International Trauma Life Support (ITLS) or Pre-hospital Trauma Life Support (PHTLS) may be substituted, may be obtained within 180 days from medical authorization date. Pediatric Education for Pre-hospital Professionals (PEPP) or Pediatric Advanced Life Support (PALS) may be obtained within 180 days from medical authorization date. o EMT-Basic and EMT-Intermediate applicants should provide legible copies with signatures and expiration dates/date of course for: ITLS and/or PHTLS or equivalent within 180 days of medical authorization. o All EMS personnel working within TSA M are required to have the appropriate OSHA and/or CBRNE training required to where the PPE (personal protective equipment) carried on many of the ambulances. Geographic Limitations of Authorization While on duty authorized individuals will retain authorization regardless of location While off duty authorized individuals will retain authorization within the bounds of TSA M This is not intended to encourage off duty personnel to stock their vehicles like an ambulance, but is instead intended to allow some flexibility in the care of patients on scene of an emergency when that individual has responded to render aid to the on duty crew Authorization of Non-EMS Personnel Individuals that are not authorized by the above policy will not be allowed to provide patient care under these EMS Guidelines or under the License of the Medical Director. Licensed Physicians and Registered Nurses as well as other allied health professionals may provide care in situations where they are part of a transport team. They must follow the orders of the transferring physician. This does not negate the requirement to have two authorized personnel on board the ambulance or to have one of those attending the patient. In instances of specialty transport the overall responsibility for the patient falls with the transport team and the transferring physician. RESTRAINTS POLICY To Control Patients with Physical Restraints . . . Restraints are used in two senses during patient transport. The first is for safety in the non-violent patient. The second is for control of the violent patient. Safety Restraint Policy All patients who are transported per stretcher will have lap belt, chest, and shoulder restraints (if available) at all times. All patients who are ambulatory, but being transported by ambulance, must have standard seat belt restraints at all times. Policy for Control of Violent Patients The decision to restrain a violent patient should be made carefully and thoughtfully. Once the decision has been made then it should be done swiftly and completely. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 66 In general, it is important that the patient in restraints can be immediately placed in a position allowing airway control and the possibility of resuscitation. 1. Request help as necessary. 2. Plan your actions ahead of time. 3. Use only the amount of force necessary. Excessive force should never be used. Always maintain control of the situation so that suction can be administered if necessary to prevent aspiration. Never place a patient in restraints of any kind with a lock that requires a key to undo, unless you are in possession of the key and are capable of immediate release of the restraint if necessary. Supine or lateral positions may be elected by EMS personnel and are a matter of judgment at the time. HELICOPTER ACTIVATION POLICY (These recommendations are based on the Air Medical Dispatch Position Paper, National Association of EMS Physicians) Medical Patients Helicopter scene response is appropriate if it can reduce transport time over ground transport in certain circumstances. The same is true if considering time to obtain ALS support. When ground transport time and ALS support is going to be significantly longer (> 20 minutes) than air transport, helicopter "back-up" to scene response may be initiated. The following medical conditions may warrant helicopter dispatch: Heart or Respiratory Patients who require rapid transport to a facility Acute Stroke patients with recent onset of symptoms Trauma Patients The following guideline applies to trauma patients receiving pre-hospital care in TSA-M (McLennan, Bosque, Falls, Hill, and Limestone Counties). The goal in the management of the trauma patient is to appropriately utilize regional air transport resources in order to reduce delays in providing optimal trauma care for severely injured trauma patients. Always contact medical control at the trauma hospital destination if possible. They can also assist in the decision to dispatch the helicopter. Decision Criteria Helicopter activation/scene response should be considered when it can reduce transportation time for TRAUMA patients meeting the following criteria. Should there be any question whether or not to activate TSA-M regional air transport resources, on-line medical control should be consulted for the final decision. Penetrating injuries to head, neck, and torso Respiratory Compromise/obstruction GCS less than 13 O2 sat less than 90% Adult Patients with a SBP less than 100 Child less than one year with SBP less than 70 or heart rate less than 100 or more than 190 Child 1-9 years with SBP less than 70 + 2 x age in years or heart rate less than 80 or more than 150 Suspected Amputation proximal to the wrist or ankle Suspected Two or more proximal long bone fractures (Femur, Humerus) Suspected Any open long bone fracture (femur, tibia, femur) Suspected Pelvic fractures Burns more than or equal to 20% BSA or more than 10% if under 6 years old Temperature less than or equal to 95◦F HOTRAC Regional EMS Guidelines Rev. 5.10 Page 67 Patients with traumatic paralysis Additionally helicopter activation/scene response should be considered when: o Patient extrication time will be prolonged (> 20 minutes). o Multiple patients on scene o Ejection from MVC Patients transported via helicopter should be taken to the nearest Level I or Level II Trauma Facility. DESTINATION POLICY General Guidelines The primary objective to be met is to ensure that each patient is taken rapidly to the nearest appropriate hospital. Patients who have been assessed and determined to be medically unstable, unconscious, or at high risk of multiple and/or severe injuries (Category 1 and 2 patients) will be safely and rapidly transported to the Regional Trauma Center. Category 3 patients will be safely and rapidly transported to the nearest appropriate trauma facility within TSA M. Category 4 patients will be safely and transported to the nearest appropriate acute care facility within TSA M. Regional transport guidelines ensure that patients who meet the triage criteria for activation of the TSA-M Regional Trauma System Plan will be transported directly to the nearest appropriate trauma facility rather than to the nearest hospital except under the following circumstances: If unable to establish and/or maintain an adequate airway, or in the case of traumatic cardiac arrest, the patient should be taken to the nearest acute care facility for stabilization. A Level III or Level IV trauma facility may be appropriate if the expected scene to Level II Trauma Center transport time is excessive (> 30 minutes) and there is a qualified physician available at the facility’s Emergency Department capable of delivering definitive care. Medical Control may wish to order bypass in any of the above situations as appropriate, such as when a facility is unable to meet hospital resource criteria or when there are patients in need of specialty care. If expected transport time to the nearest appropriate Trauma Center is excessive (> 30 minutes) or if a lengthy extrication time (> 20 minutes) is expected, medical control or the EMS crew on scene should consider activating air transportation resources. Note: Should there be any question regarding whether or not to bypass a facility, on-line medical control should be consulted for the final decision from the receiving facility. **Patients that are in active labor and less than 35 weeks gestation should be taken directly to a NICU-capable facility. In TSA M, that facility is Hillcrest Baptist Medical Center. All other pregnant patients shall follow the regional transport guidelines that have been established in TSA M. PRE-HOSPITAL TRAUMA TRIAGE Goal Patients will be identified, rapidly and accurately assessed, and based on identification of their actual or potential for serious injury, will be transported to the nearest appropriate TSA-M trauma facility. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 68 Purpose In order to ensure the prompt availability of medical resources needed for optimal patient care, each patient will be assessed for the presence of abnormal vital signs, obvious anatomic injury, mechanism of injury, and concurrent disease/predisposing factors. Definition Trauma Patient—the patient is a victim of an external cause of injury that results in major or minor tissue damage or destruction caused by intentional or unintentional exposure to thermal, mechanical, electrical, or chemical energy, or by asphyxia, submersion, or hypothermia. System Triage 1. Unless immediate stabilization is required, patients in TSA-M with the following injuries, with significant mechanism of injury, should be taken directly to Hillcrest Baptist Medical Center or another appropriate trauma facility offering resources not available to Hillcrest Baptist Medical Center, unless immediate stabilization is required: Penetrating injuries to head, neck, and torso Respiratory Compromise/obstruction GCS less than 13 O2 sat less than 85-90% Adult Patients with a SBP less than 100 Child less than one year with SBP less than 70 or heart rate less than 100 or more than 190 Child 1-9 years with SBP less than 70 + 2 x age in years or heart rate less than 80 or more than 150 Suspected Amputation proximal to the wrist or ankle Suspected Two or more proximal long bone fractures (Femur, Humerus) Suspected Any open long bone fracture (femur, tibia, femur) Suspected Pelvic fractures Burns more than or equal to 20% BSA or more than 10% if under 6 years old Temperature less than or equal to 95◦F Patients with traumatic paralysis 2. If ground transport time to Hillcrest Baptist Medical Center is greater than 30 minutes with protocols, or if lifesaving interventions (e. g. airway stabilization, chest tube insertion, etc.) are required for safe transport, contact medical control and/or take the patient to the nearest medical facility and call for the helicopter transport to meet you at the closest agreed upon landing zone. 3. When on-scene EMS personnel are unable to establish on-line contact with medical control at the receiving TSA-M facility, off-line medical trauma triage criteria will be followed. DNR CONDITIONS The following procedures are not to be performed on patients with DNR orders: CPR Endotracheal intubation or other advanced airway management Artificial ventilation Defibrillation Transcutaneous cardiac pacing Administration of cardiac resuscitation medications The following conditions are considered to be automatic DNR in which there is no need to contact medical control; if there is any doubt, you may contact Medical Control. It is better to err on the side of resuscitation. Appropriate DNR HOTRAC Regional EMS Guidelines Rev. 5.10 Page 69 documentation should be completed in all cases. Documentation of position patient found in and any other pertinent information should be included. Decapitation Rigor Mortis Total incineration Decomposition Dependent lividity Mass Casualty Incident where triage principles preclude CPR from being initiated on every victim. Traumatic arrest resulting from blunt injury presenting apneic and pulse less DNR order by patients' physician: Direct phone contact* Written DNR order signed by physician State authorized form, properly signed State authorized bracelet or necklace *If you receive DNR orders from a patient's private physician, via direct phone contact, the orders will be honored. (Even if resuscitative efforts are in progress.) The physician, however, must provide to you their full name, a telephone number where they may be reached for the next 60 minutes and their State License Number. This information will be provided to law enforcement on scene and documented in the patient care report. If there is a DNR dispute, contact Medical Control. In QUESTIONABLE DEATH, with Police request, you may draw red and purple top tubes for police investigation. First, DNR orders must have been received and documented. Then, obtain the signature of the officer requesting the lab. The run record should include: Assessment of the patient's condition The method of identification of DNR order or condition Any problems relating to implementation of the DNR order Identification of persons used to identify the patient You may accept an out of state DNR order if there is no reason to question the authenticity of the order. DNR orders do not apply if the patient is pregnant. REFUSAL TO TRANSPORT General Statement The following is an outline of legal principles that may assist with determining an individual’s right to refuse treatment and or transport against medical advice. 1) Consent a) The patient has the responsibility to consent or to refuse treatment. If he is unable to do so, a responsible relative or guardian has this right. b) When waiting to obtain lawful consent from the person authorized to make such consent would present a serious risk of death, serious impairment of health or would prolong severe pain or suffering of the patient, treatment may be undertaken to avoid those risks without consent. In no event should legal consent procedures be allowed to delay immediately required treatment. c) In non-emergency cases, consent should be obtained from the patient or a responsible party prior to undertaking any treatment. d) Age: Patient must be 18 years of age or older, or between 14 and 17 years and "emancipated" (i.e., living apart from parents). e) If the patient is under age, consent should be from a natural parent, adopted parent, or legal guardian. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 70 2) Mental Competence a) A person is mentally competent if he or she: i) Is capable of understanding the nature and consequences of the proposed treatment. ii) Has sufficient emotional control, judgment, and discretion to manage his or her affairs. b) Ascertaining that the patient is oriented, has an understanding of what happened and may possibly happen if treated or not treated, and a plan of action, such as which he will call for transportation home, should be adequate for these determinations. (i.e., patients with impaired cerebral perfusion, in shock, postictal, or under the influence of drugs/alcohol will be unlikely to fulfill these criteria.) c) If the patient is not mentally competent under these guidelines, consent should be obtained from another responsible party, who must be mentally competent and must be 21 years of age, in the following order of preference: i) Spouse ii) Adult son or daughter iii) Parent iv) Adult brother or sister v) Legal guardian d) If the patient is not mentally competent and none of the above persons can be reached, the person should be treated and transported to a medical facility. It is preferable under such circumstances to obtain concurrence of a police officer in this course of action. e) If the patient himself is not competent to consent and a responsible person is present, and if that responsible person is of age and competent, he or she has the same right to consent or refuse treatment as the patient himself. His wishes can not be ignored in a non-life-threatening situation. Procedure for Refusal If a patient wishes to refuse treatment, examination, or transportation, the following steps will be taken: 1) The provider will complete a Patient Refusal Checklist. This includes assessment of the patient's level of orientation, level of consciousness, whether there is a head injury, or whether the patient is under the influence of drugs and/or alcohol. 2) If any of the above conditions are present, and the patient refuses care, medical control will be contacted; the contact and what the orders were will be documented. If unable to contact, document why. 3) The patient will be advised that further harm could result without treatment and evaluation, and that transport by means other than ambulance could be hazardous in light of the patient's injury or illness. 4) The type of refusal that is involved should be documented, whether the patient has used all EMS services, refused transport but accepted field treatment, refused field treatment but accepted transport whether released in the custody of themselves, law enforcement, or others. 5) The patient will be provided with a refusal information sheet. A copy of this sheet will be signed by the patient and kept with the file. It will be noted whether the patient refused this sheet on the checklist. The signed information sheet as well as the refusal checklist will be kept with the patient file. SPINAL MOTION RESTRICTION GUIDELINES Injury to the spine, especially the cervical and thoracic spine can have catastrophic consequences. Because of this, any guidelines for field immobilization criteria must be extremely conservative. The consequences of any other approach can be devastating. Primary Injury to the spinal cord occurs at the time of impact or injury. Secondary injury occurs later from swelling, ischemia, or movement of bony fragments or the cord itself. In the field, we must be sure to do all we can to prevent any secondary injury. There are two reasons only to remove a helmet in the field: 1. Urgent airway problem that requires helmet removal for evaluation & management HOTRAC Regional EMS Guidelines Rev. 5.10 Page 71 2. A helmet that is obviously too large that prohibits the ability to package the patient and restrain the head and neck. Motorcycle helmets may cause airway obstruction and should then be removed per ITLS protocol Note that in other scenarios, helmet removal in the field could lead to delay and to possible medico-legal consequences. Assessment Guidelines 1) Mechanism of Injury a) Positive mechanism is any history or evidence of impact forces that could be capable of damaging the spinal column. b) Negative mechanism is that given the impact and forces involved, there is no reasonable possibility that the spine might be injured. c) Uncertain mechanism is when the actual impact and forces or injury are uncertain. 2) Assessment a) Pain. When asked, the patient can tell you he/she has pain. If there is any other distracting injury, then this is not a valid criterion for assessment. b) Neurologic assessment. Motor and sensory functions including strength and touch and pain sensation reflect injury to the cord. In the field, positive findings are valid. Negative findings may not be valid depending on the field situation. Most of the time, a complete neurologic exam cannot be done in the field. c) Head injury. In any patient with abnormal mental status or level of consciousness, the assessment should be considered unreliable. For all patients with a positive mechanism of injury, full spinal motion restriction is required. In unimpaired patients with a negative mechanism of injury and negative assessment, spinal motion restriction may be omitted. If the mechanism is uncertain, and the patient has any signs or symptoms that could be related to spinal injury, full spinal motion restriction is required. In cases with unreliable history or exam for any reason, full spinal motion restriction is required. Very small children may be immobilized in a car seat with towels, bandage, etc. if possible to maintain immobilization. Sometimes this may prevent unnecessary movement of the spine. Short Board/KED Use The short board / KED should be used for patients who are in a position (such as an automobile) that does not allow for the use of the long backboard and requires full spinal motion restriction. Although this is the best way to extricate anyone with a possible spinal injury, there are certain situations where a more rapid method should be used. Situations Requiring Rapid Extrication The scene is unsafe, for example: Fire or immediate danger of fire Danger of explosion Rapidly rising water Structure in danger of collapse Continuing toxic exposure The primary survey reveals a condition that requires immediate intervention that cannot be done in the vehicle, for example: Airway obstruction that you cannot relieve by jaw thrust or finger sweep Cardiac or respiratory arrest Chest or airway injuries requiring ventilation or assisted ventilation Deep shock or bleeding you cannot control HOTRAC Regional EMS Guidelines Rev. 5.10 Page 72 Authorized Medications ADENOSINE Indications Administration Contraindications Precautions Side Effects and Special Notes First drug for supraventricular tachycardia Wide complex tachycardia after Lidocaine Adult: Rapid IV bolus over 1-2 seconds of 6mg initially, followed immediately by 20ml saline over 5-10 seconds. A second dose of 12mg in 1-2 minutes if needed using the same technique. A third dose of 12mg may be given if necessary after contacting medical control, again using the same technique. Pedi: Rapid IV 0.2 mg/kg initial dose followed immediately with 10ml saline over 10-15 seconds. A second identical dose may be given if necessary. Known hypersensitivity to the drug. Second and third degree heart block. Adverse effects include flushing, dyspnea, chest pain, anxiety, bradycardia, and occasionally hemodynamic disturbances – all of which are short lived. Whenever possible establish the IV at the antecubital. Caffeine and theophylline antagonize adenosine’s effects. Larger doses may be required. Warn patients to expect a brief sensation of chest discomfort. If patient is hemodynamically unstable, use the Tachycardia, Unstable With Pulses guideline. ALBUTEROL Indications Administration Contraindications Precautions Side Effects and Special Notes Asthma, acute wheezing, dyspnea with wheezing Solution Adult: 2.5mg diluted to 3ml with NS nebulizer. May repeat to total of three doses. Pedi: Same as for adult Known hypersensitivity to the drug. Albuterol has sympathomimetic effects. Discontinue immediately if patient develops chest pain or dysrhythmia. Inhaled, Albuterol can result in paradoxical bronchospasm, which can be life threatening. If this occurs, the nebulizer should be discontinued immediately. Monitor blood pressure, heart rate/rhythm closely and contact medical control if any concerns arise. Medications such as MAO inhibitors and tricyclics may potentiate tachycardia and hypertension. AMIODARONE Indications Administration Contraindications Precautions Side Effects and Special Notes Stable wide-complex tachycardia (systolic BP > 80, weakness, no altered LOC) Adult: 150mg Slow IVP over 10 minutes (15mg/min). Mix 150mg with 100cc D5W (infuse at 10ml/min). Pedi: not indicated by these guidelines. Heart block Cardiogenic shock Allergic to Amiodarone Nausea and vomiting are common reactions, be prepared to administer Promethazine as needed. Hypotension is common, monitor blood pressure frequently. Flushing, edema, sinus arrest, hypotension, nausea & vomiting ASPIRIN Indications Administration Contraindications Chest pain of suspected cardiac origin Suspected congestive heart failure Four 81 mg (Total: 324mg) chewable aspirin to chew and swallow only. Known hypersensitivity to Aspirin or other NSAID (Like Motrin®) GI bleeding ATROPINE Indications Administration HOTRAC Regional EMS Guidelines Rev. 5.10 First drug for symptomatic bradycardia. Second drug for asystole or bradycardic PEA. Antidote for some insecticide exposures (i.e. organophosphate with symptoms of excess cholinergic stimulation: salivation, lacrimation, urination, defecation, increased GI motility, and emesis. (SLUDGE) Asystole Adult: 1 mg IV, repeat every 3-5 minutes. Max dose 0.04 mg/kg Pedi: 0.02 mg/kg IV, minimum 0.1 mg Symptomatic Bradycardia Adult: 0.5-1.0 mg IV, repeated if needed at 3-5 minute intervals to a dose of 3 mg; not to exceed 0.04 mg/kg (stop at ventricular heart rate which provides adequate mentation, B/P –aim for HR = 60/minute) Pedi: 0.02 mg/kg IV, minimum 0.1 mg Consider Pacing if bradycardia persists after 2 doses May be given through ET tube at 2 times the IV dose. Max ET dose is 6mg. For symptomatic insecticide exposures: Contact medical control for dosage (usually begin with 1mg Page 73 Contraindications Precautions Side Effects and Special Notes IV and titrate until breath sounds are clear; total required dose may be massive). Known hypersensitivity to the drug Avoid in hypothermia Can cause increased cardiac O2 consumption Remember that in cardiac arrest situations that atropine dilates pupils Will not work in patients with heart transplants DEXTROSE 5% Indications Administration Precautions Side Effects and Special Notes IV solution to keep vein open. Vehicle for mixing medications for IV delivery. Adult: See Amiodarone. Pedi: same as above Patients at risk for elevated I.C.P. Elevated blood glucose concentrations. Local venous irritation. DEXTROSE 50% Indications Administration Precautions Side Effects and Special Notes Blood Glucose concentration < 50 mg/dL; IV solution to keep vein open; Vehicle for mixing medications for IV delivery. Adult: See Amiodarone. Pedi: same as above Use with caution with stroke specific symptoms. (Unilateral weakness, paralysis, and paresis) Extravasations of glucose can cause tissue necrosis. Ensure IV patency before and during administration One bolus should raise the blood sugar 50-100 mg/ml and, therefore, will be adequate for most patients Effect may be delayed in elderly patients with poor circulation Do not administer dextrose to a patient who is seizing due to trauma Dextrose 50% should be diluted 1:1 with normal saline (to create D25) for patients 8 years and younger DIAZEPAM Indications Administration Contraindications Precautions Side Effects and Special Notes First drug for status epilepticus Sedation prior to cardioversion, pacing, or other painful procedure Seizure: Adult: 0.1 mg/kg IV Pedi: 0.1 mg/kg IV Sedation: Adult: 2.5 – 5 mg IVP repeat as necessary. (No more frequently than q 2 min) Pedi: Not given for sedation Known hypersensitivity to drug Shock, coma, and acute alcohol intoxication May cause changes in heart rate and BP May cause respiratory rate or APNEA Headache, over sedation, drowsiness, amnesia, nausea, vomiting, hiccups DILTIAZEM Indications Administration Contraindications Precautions Side Effects and Special Notes Drug of second choice for SVT and rapid atrial fib or flutter after contacting medical control Adult: 5-10 mg IV over 2 minutes Pedi: 0.2 mg/kg do not exceed 10mg over 2 minutes Severe hypotension or cardiogenic shock Second or third degree AV block (except with a functioning pacemaker) Sick sinus syndrome (except with a functioning pacemaker) Severe CHF (unless secondary to SVT) Wolff-Parkinson-White, or Lown-Ganong-Levine syndromes Wide complex tachycardia Known hypersensitivity to drug Do not give with IV beta blockers (Labetalol) May cause hypotension, bradycardia, dizziness, headache, and rarely seizures In elderly patients drug must be given over 3 minutes to reduce untoward effects In controlled studies in the US about 60% of patients with SVT converted to a sinus rhythm within 10 minutes of IV Diltiazem. Uncontrolled studies reported in the world literature describe a conversion rate of about 80%. The effect of a single injection lasts for 30 to 60 minutes when conversion to sinus rhythm does not occur. DIPHENHYDRAMINE Indications Second drug for anaphylaxis and severe allergic reactions First drug to counteract dystonic reactions to antipsychotic drugs HOTRAC Regional EMS Guidelines Rev. 5.10 Page 74 Administration Contraindications Precautions Side Effects and Special Notes Anaphylaxis Adult: 50 mg slow IV push or deep IM Pedi: 1-2 mg/kg slow IV (max 50 mg total) Dystonic reaction Adult: 25 mg slow IV push or deep IM Pedi: 1 mg/kg slow IV (max 25 mg total) Do not administer to newborns and neonates or breast feeding patients May cause drowsiness which may be potentiated by alcohol or depressants Not the first line drug for allergic reactions, but may be useful for long transports. May see CNS stimulation in children Side effects include dry mouth, dilated pupils, flushing, and drowsiness. Diphenhydramine should be used with caution in patients with Asthma/COPD, glaucoma, and bladder obstruction, as all of these can be exacerbated by its administration. DOPAMINE Indications Administration Contraindications Precautions Side Effects and Special Notes Significant hypotension and signs of shock Hypovolemic shock only after fluid replacement Dosage per medical control then use drip rate table below Use premixed solution with gtt set and Exacdrop™ or similar device. Known hypersensitivity Dopamine may induce tachy-dysrhythmia. If the heart rate exceeds 140, the infusion should be stopped At low doses, decreased B/P may occur due to peripheral vasodilatation. Increasing the rate will correct this. Should not be mixed with sodium bicarbonate Extravasations at the IV site can cause skin sloughing due to vasoconstriction; assure IV patency before initiating an infusion. Drip Rate Table (1600 g/ml) g/kg/ min 5 10 15 20 110 10 20 30 40 132 10 25 35 45 Patient weight in lbs 154 176 198 15 15 15 25 30 35 40 45 50 50 60 70 gtt per minute (or ml/hr) 220 20 35 55 75 242 20 40 60 85 EPINEPHRINE Indications Administration Cardiac arrest with VF, Pulse less VT, Asystole, PEA Anaphylaxis Cardiac Arrest Adult: 1mg IV q 3 min Pedi: First dose: 0.1 mg/kg IV (0.1 ml/kg of 1:1,000 solution) Subsequent doses 0.2 mg/kg IV (0.2 ml/kg of 1:1,000 solution) Anaphylaxis Adult: 0.3 - 0.5 mg (0.3 ml of 1:1,000) SQ or 0.1 - 0.5mg (1:10,000) IV very slowly Pedi: 0.01 mg/kg (0.01 ml/kg 1:1,000) SQ or IV ET tube doses at 2 to 2½ times the IV dose Contraindications Precautions Side Effects and Special Notes Epi Auto-injectors (both adult and pediatric) may be utilized and should be used as directed by the service’s medical director. None in cardiac arrest Dysrhythmia, coronary insufficiency, organic brain damage Do not add to solutions containing bicarbonate Increase in myocardial oxygen demand can cause angina or MI in patients with CAD Use with caution in hyperthyroidism, peripheral vascular disease, or cerebrovascular disease Anaphylactic shock is a systemic allergic reaction with cardiovascular collapse. Angioedema involves swelling of the mucous membranes; potential exists for airway compromise. Mild or moderate allergic reactions with urticaria or wheezing may progress to anaphylaxis or severe angioedema. Monitor patient carefully and treat according to patient status. Epinephrine comes in two strengths. Use of the wrong formulation will result in a ten-fold difference in dosage. Be sure you use the right one. Anxiety, tremor, palpitations, vomiting, and headache are common side effects Services with full time paramedic staffing are not required to stock auto injectors FUROSEMIDE Indications Administration Adjunctive therapy for acute pulmonary edema and hypertensive crisis Adult: 0.5 – 1 mg/kg IV slow push over 1-2 minutes HOTRAC Regional EMS Guidelines Rev. 5.10 Page 75 Contraindications Side Effects and Special Notes Pedi: 1mg/kg IV slow push over 1-2 minutes Known hypersensitivity to the drug Patients with anuria Possible side effects include, hypotension, EKG changes, chest pain, dry mouth, hypochloremia, hypokalemia, hyponatremia, and hyperglycemia Onset occurs within 5 minutes of administration, peak effects occur within 30 minutes of administration GLUCAGON Indications Administration Contraindications Precautions Side Effects Hypoglycemia, after two unsuccessful IV attempts Procedure Adult: 1 mg IM Pedi: 0.1 mg/kg IM Known hypersensitivity to drug Only effective if there are stores of liver glycogen Return to consciousness may take between 5 and 20 minutes Use with caution in patients with a history of cardiovascular or renal disease Glucagon exerts a positive inotropic action on the heart and decreases renal vascular resistance GLUCOSE, INSTANT Indications Administration Contraindications Hypoglycemia in patients who can protect their own airway Administer entire contents of a 15 gm tube PO Semiconscious patients Unconscious patients LABETALOL Indications Administration Contraindications Precautions Side Effects and Special Notes Second drug for hypertensive crisis B/P 110 diastolic Adult: 20 mg IV push over 2 minutes. May repeat with 40 mg PRN q 10 min with approval of medical control Patients with bronchial asthma, congestive heart failure, high degree AV block, bradycardia, or cardiogenic shock. When administering Labetalol stay alert for signs and symptoms of CHF, bradycardia, shock, heart block, or bronchospasm. If any of these appear discontinue the drug immediately. Supine B/P should be monitored immediately before the injection, at 5 minutes and 10 minutes after the injection. These should be documented. Postural hypotension should be anticipated LACTATED RINGERS Indications Administration Contraindications Precautions Side Effects/Special Notes Suspected volume depletion due to thermal burns Adult: IV fluid therapy due to thermal burns: 2-4ml x burn % x weight (kg) up to 2 liters Pedi: same as above. Pulmonary edema Fluid overload; Potentially sensitive patients may include those with renal failure, pregnancy, neardrowning and CHF Fluid overload; pulmonary edema LIDOCAINE HOTRAC Regional EMS Guidelines Rev. 5.10 Page 76 Indications Administration Following successful defibrillation Recurrent or refractory VF or VT Ventricular or wide complex tachycardia with pulses Premedication for intubation of patient with head trauma Cardiac Arrest (Pulse less VF or VT) Adult: 1.5 mg/kg IV bolus repeat 0.5 mg/kg IV bolus q 3 min up to 4/mg/kg Pedi: 1.5 mg/kg IV bolus repeat 0.5 mg/kg IV bolus q 3 min up to 4 mg/kg VT or Wide Complex Tach with pulse Adult: 1 mg/kg IV Pedi: 1 mg/kg IV Premedication for intubation of head trauma Adult: 1 mg/kg IV (No drip necessary) Pedi 1 mg/kg IV (No drip necessary) ET tube doses at 2 to 2½ times the IV dose Infusion Adult: Use a premixed infusion at 4 mg/ml concentration with a micro drop set and a Exacdrop™ or similar device. Then use chart below. Lidocaine Drip Bolus dosage 1 mg/kg 1-2 mg/kg 2-3 mg/kg mg/min 2 3 4 gtt/min, or ml/hr 30 45 60 Dosage Pedi: Use a premixed infusion at 4mg/ml concentration with a gtt set and a Exacdrop™ or similar device. Then use chart below. Pedi Lidocaine Drip 3 3 Weight 15lb 22lb 44lb 55lb 66lb 77lb 88lb 99lb l b 30 3 5 7 9 11 14 16 18 20 g/min 40 4 6 9 12 15 18 21 24 27 g/min 1 50 g 5 8 15 19 23 26 30 34 1 /min gtt/min Known hypersensitivity to drug Severe SA, AV or interventricular blocks in the absence of artificial pacemaker. High grade AV block is relative contraindication Do not treat ventricular escape beats or accelerated idioventricular rhythm with Lidocaine Lidocaine is metabolized in the liver; elderly patients and those with liver disease or poor liver perfusion secondary to shock or CHF are more likely to experience side effects Side effects include drowsiness, confusion, convulsion, hypotension, bradycardia, and tachycardia. Head trauma requires careful airway management. If endotracheal intubation is appropriate, pretreatment with Lidocaine may help avoid further increase in intracranial pressure, if time permits. Resist the urge to treat every PVC. Lidocaine is a toxic drug. PVCs outside the setting of acute MI should not be treated. Hypoxia can generate PVCs, and Lidocaine will not help; treat the cause. Best available evidence currently indicates that prophylactic Lidocaine (in the setting of MI without PVCs) may actually increase mortality. For patients over 70, or with liver dysfunction, the usual adult loading dose will be utilized. This dose will then be followed by half of the usual maintenance dose of Lidocaine. Contraindications Precautions Side Effects and Special Notes MAGNESIUM SULFATE Indications Administration Contraindications Precautions Side Effects and Special Notes First drug for torsades de pointes. First drug for seizures due to eclampsia Torsades de pointes: 2gm over 2 minutes; draw up 2 gm into a 20 ml syringe then draw up normal saline to fill the syringe to the 20 ml mark. Invert the syringe several times to mix the medication then give 10 ml of the solution every 6 seconds. Eclampsia: Mix 4 gm in a 50 cc bag of D5W and infuse over 20 minutes None in cardiac arrest Active labor AV Block Decrease in respiratory or cardiac function Eclampsia is defined as pregnancy > 20 weeks with the following 1. Blood Pressure > 180 mm systolic or > 120 diastolic with altered mental status, or 2. Seizures with B/P > 140/90 Principle side effect is respiratory depression, ventilator assistance may be needed Not for pediatric use HOTRAC Regional EMS Guidelines Rev. 5.10 Page 77 MIDAZOLAM Indications Administration Contraindications Precautions Side Effects and Special Notes Sedation prior to cardioversion, pacing, or other painful procedure Sedation: Adult: 2.5 – 5 mg IVP repeat as necessary. (No more frequently then q 2 min) Pedi: Not given for sedation Known hypersensitivity to drug Shock, coma, and acute alcohol intoxication May cause changes in heart rate and BP May cause respiratory rate or APNEA Headache, over sedation, drowsiness, amnesia, nausea, vomiting, hiccough M ORPHINE SULFATE Indications Administration Contraindications Chest pain with anxiety Extremity injury where severe pain is present: to be given only in the absence of any evidence of head, chest, or abdominal injuries. If you think MS should be given for any other reason contact medical control Severe burns after contacting medical control Adult: 2 mg IV or IM initially; repeat q 3-5 PRN up to 10mg. The goal is decreased anxiety and patient comfort. Contact medical control for additional doses. Pedi: 0.1 – 0.2 mg/kg IV slowly Known hypersensitivity to drug Precautions Hypotension is a contraindication to use. Remember, some people will be hypotensive in response to pain itself. Smaller doses are less likely to cause or aggravate hypotension. Contact medical control first if head, chest, or abdominal trauma is also a relative contraindication to morphine use, since the analgesic effect removes the clinical signs that need to be observed Do not use in the presence of major blood loss. The body’s compensatory mechanisms will be suppressed by the use of morphine and the hypotensive effect will be very prominent. May cause respiratory effort or even APNEA May cause vomiting; administer slowly. It is not necessary to stock Morphine Sulfate if Nalbuphine is carried. Side Effects and Special Notes NALOXONE Indications Administration Contraindications Precautions Side Effects and Special Notes Narcotic and synthetic narcotic overdose Coma of unknown origin Adult or Pedi: 2mg IV, IM or IO If no response is observed this dose may be repeated after 5 minutes if narcotic overdose is strongly suspected. May be given via ET tube at 2 times the IV dose. Known hypersensitivity to drug In patients physically dependant on narcotics, violent withdrawal symptoms may be precipitated. Be prepared to restrain the patient. Titrate the dose (1-2 mg at a time) to reverse cardiac and respiratory depression but to keep the patient groggy. May need large doses (8-12 mg) to reverse propoxyphene (Darvon) overdose The duration of some narcotics is longer than Naloxone and the patient must be monitored closely. Repeated doses of Naloxone may be required. Patients who have received this drug must be transported to the hospital because coma may reoccur when Naloxone wears off. With an ET tube in place and assisted ventilation, narcotic overdose patients may be safely managed without Naloxone. Think twice before totally reversing coma; airway may be lost, or (worse) the patient may become violent and may refuse transport. NITROGLYCERINE (NTG) Indications Administration Contraindications Precautions Side Effects and Special Notes Chest pain of suspected cardiac origin Hypertensive crisis Pulmonary edema Chest Pain (Systolic 100) & Hypertensive Crisis (Diastolic 100) Adult: 1 NTG 0.4 mg SL q 5 minutes max of 3 doses (Must check B/P prior to each dose) Pulmonary Edema (Systolic 100) Adult: 2 NTG 0.4 mg SL q 5 minutes max of 3 doses (Must check B/P prior to each dose) Known hypersensitivity to nitrates May cause profound hypotension and reflex tachycardia Common side effects include throbbing headache, flushing, dizziness, and burning under the tongue. Less common: orthostatic hypotension, sometimes marked Because nitroglycerine causes generalized smooth muscle relaxation, it may be effective in relieving chest pain caused by esophageal spasm. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 78 May be effective even in patients using paste, disks, or oral long acting nitrate preparations NORCURON Indications Administration Contraindications Precautions Side Effects and Special Notes Indications Administration Contraindications Precautions To achieve paralysis to facilitate endotracheal intubation Adult: Defasiculating Dose: 0.01 mg/kg IVP Maintaining Paralysis: 0.1 mg/kg IVP Pedi: not indicated Patients with known hypersensitivity Endotracheal intubation equipment must be ready Increased intracranial and intraocular pressure Hypertension and hypotension Respiratory depression Bradycardia NOTE: Norcuron is packaged with a vial of sterile water but in the absence of sterile water, normal saline may be used for reconstitution. NORMAL S ALINE Hypotension (Systolic B/P 90), Altered LOC, Cardiac Arrest, V-Tach and Wide complex Tach with a pulse, Hyperthermia, Category 1 or 2 trauma, trauma with significant blood loss potential, vaginal bleeding TKO = 5-10 gtt/min Side Effects and Special Notes In hemorrhagic shock, volume expansion with blood is the treatment of choice. Normal saline will temporarily expand intravascular volume and “buy time”, but it does not increase the O2 carrying capacity, and is not sufficient in severe shock. Because of this rapid transport is still needed to treat severely Hypovolemic patients who need blood and possible surgical intervention. Volume overload is a constant danger, particularly in cardiac patients. Keep a close eye on your IV rate during transport Flow rate through a 14g cannula is twice the rate through an 18g cannula, and volume administration in trauma patients can be accomplished more rapidly. If the patient has poor veins, a smaller bore is better than no IV at all. IVs in unstable trauma patients should be placed en route, and may be left to the emergency department for short transports. Do NOT delay transport in critical patients for IV attempts. If you are unable to start in two attempts, another qualified attendant may try, or you may leave the IVs for the emergency department. OXYGEN Indications Administration Precautions Side Effects and Special Notes Chest Pain O2 Sat < 90% Dyspnea Suspected closed head injury Category 1 & 2 trauma Suspected carbon monoxide poisoning Cyanosis Hypotension from any cause Altered LOC (from baseline for the Suspected hypoxemia patient) High flow O2 (12-15 liters/min via non or partial rebreather mask) is indicated for the conditions listed above. Otherwise administer O2 with the appropriate adjuncts at your discretion. If the patient is not breathing adequately, the treatment of choice is ventilation, not just oxygen. A small percentage of patients with chronic lung disease breathe because they are hypoxic. Administration of O2 will inhibit their respiratory drive. Do not withhold O2 because of this possibility. Be prepared to assist ventilation if needed. Oxygen toxicity is not a hazard of short-term use. Always note O2 Sat before and after administering O2 If pulse oximeters are not available clinical signs of perfusion must be monitored and documented. PROMETHAZINE HOTRAC Regional EMS Guidelines Rev. 5.10 Page 79 Indications Administration Contraindications Precautions Side Effects and Special Notes Persistent vomiting with long transport time ( 15 min) Adult: Dilute 12.5 mg in 20 ml syringe (1 ml Promethazine to 19 ml NS) and give slow IV push over 2 minutes (1 ml every 6 seconds) Can repeat once PRN Pedi: Not given to pediatric patients Altered level of consciousness Traumatic injury Pregnancy or Lactation Can cause dystonic reaction in some individuals Use with caution if patient ever had adverse reactions to phenothiazine May cause localized burning and irritation upon administration May cause drowsiness, confusion, disturbed coordination, restlessness, tremors, transient hypotension, blurred vision, dry mouth, dry nose, dry throat, irregular respiration, photosensitivity Incompatible with Morphine Sulfate and Nalbuphine SUCCINYLCHOLINE Indications Administration Contraindications Precautions Side Effects and Special Notes To facilitate intubation Adult: 1 mg/kg IV push over 10 to 30 seconds Pedi: Not given to pediatric patients Inability to control airway and/or support ventilations with oxygen and positive pressure. Hypersensitivity May cause cardiac dysrhythmia May cause hypotension Onset: Less than 1 minute. Duration: 3 to 10 minutes after initial IV dose Succinylcholine has no effect on consciousness or pain. May only be given and carried by those specifically trained and certified by the medical director. SODIUM BICARBONATE Indications Administration Contraindications Precautions Side Effects and Special Notes Tricyclic Overdose Adult: 1 mEq/kg IV after contacting medical control Pedi: Not given to pediatric patients Known metabolic or respiratory alkalosis, known hypocalcaemia Addition of too much sodium bicarbonate may result in alkalosis. Alkalosis is very difficult to reverse and can cause as many problems as acidosis. May increase cerebral acidosis Incompatible with almost every other drug. Sodium bicarbonate’s lack of proven efficacy and its numerous adverse effects have lead to the reconsideration of its role in cardiac resuscitation. Effective ventilation and circulation of blood during CPR are the most effective treatments for acidemia associated with cardiac arrest. Sodium bicarbonate may be considered for the dialysis patient in cardiac arrest due to suspected hyperkalemia. TERBUTALINE Indications Administration Contraindications Precautions Severe wheezing and bronchospasm Adult: 0.25 mg SQ May repeat dose in 15-30 minutes after contacting medical control Pedi: Not given to pediatric patients Known hypersensitivity to drug Tachydysrhythmias, coronary insufficiency May cause tachydysrhythmias or hypertension Monitor V/S closely THIAMINE Indications Administration Contraindications Precautions Side Effects Coma of unknown origin especially associated with alcohol Adult: 100 mg IVP Pedi: Rarely indicated and not by these guidelines None in emergency setting Precede D50W in administration sequence. Rare anaphylactic reactions have been reported. Rare, if any (hypotension and dyspnea) HOTRAC Regional EMS Guidelines Rev. 5.10 Page 80 PROCEDURES These descriptions of procedures do not constitute the total list of procedures that an EMT, EMTI or Paramedic may be required to proficiently perform. They are intended to be guidelines for interventions that are used, and the list is not all-inclusive. Each member of the EMS team is expected to be proficient in these procedures (as appropriate per level of provider). These procedures must be demonstrated and skills-proficiency tested and documented on at least an annual basis. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 81 AUTOMATIC EXTERNAL DEFIBRILLATOR GUIDELINE Note: The following guideline is written presuming that only BLS and the AED are available during a cardiac arrest. If a Paramedic unit is available, then the Paramedic will follow the cardiac arrest guidelines. He/she may utilize the AED but should convert to their monitor/defibrillator before transport when possible. 1. Confirm cardiac arrest (apneic & pulse less). DO NOT put an AED on a patient who has a pulse or is breathing. Have the AED available for patient’s experiencing severe chest pain or shortness of breath that may go into cardiac arrest. 2. If witnessed cardiac arrest and AED is available, attach AED immediately and turn on. Follow AED instructions. 3. If witnessed cardiac arrest with no AED immediately available (2 – 3 minutes), or if patient is found in cardiac arrest with unknown down time, begin CPR for 2 minutes. CPR should be conducted in accordance with 2006 Emergency Cardiac Care (ECC) standards (30 compressions to 2 rescue breaths for all patients over 1 year of age). 4. After 2 minutes of CPR attach the AED and turn on. Follow AED instructions. 5. Move patient to a firm surface before beginning CPR. 6. Ensure patient is not lying in/on or touching standing water. 7. Check patient for any of the following: Remove any excessive chest hair by using a disposable razor or shears. Dry patient’s chest if wet. Place pads 1” above or below a pacemaker, internal IV port, central line, or AICD. Remove any medication patches from chest area using a gloved hand. Make sure no one is touching patient prior to pushing defibrillation button. All clothing must be removed from the patient’s chest area, including bras or medical support devices. Remove any jewelry from chest or around neck. 8. DO NOT USE AED on patient’s less than one year of age (infants). 9. If patient is less than 9 years of age use pediatric pads if available or adjust AED for pediatric patient if possible. If pediatric pads or device is not available adult pads and device may be used. 10. Ensure pads do not touch and are at least 1” apart. DO NOT cut adult pads to make them fit pediatric patient. If pads are too large for pediatric patient place one in the center of the patient’s chest and the other in the center of the patient’s back. 11. Conduct 2 minutes of CPR between shocks. If no shock advised continue CPR in accordance with 2006 ECC standards.* 12. DO NOT STOP CPR to check for pulse after shocking. Continue CPR for 2 minutes. Check ABC’s every 2 minutes or after 5 sets of CPR (30 compressions to 2 rescue breaths). 13. All uses of AED require (by State Law) review of the case, so provide Medical Director the trip summary and recording. *Newer models of AEDS are programmed in accordance with 2006 ECC standards. Older AEDS may require to be reprogrammed by the manufacturer. If using an older model AED that has not been programmed with the newer standards follow the AED prompts. DO NOT turn the AED off and on during CPR. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 82 CRICOTHYROTOMY Level Indication Contraindication Technique Notes Documentation Paramedic with special clearance by the medical director Inability to ventilate with a BVM and an inability to establish airway by any other means Acute upper airway obstruction which cannot be relieved by obstructed airway maneuvers Upper airway trauma with inability to ventilate the patient with severe respiratory insufficiency Ability to ventilate the patient by any other means. 1. Open the package, remove the device, and familiarize yourself with its contents. 2. Place the patient in a supine position. Assure stable positioning of the neck region (place a pillow or piece of clothing under the patient’s shoulders) and hyperextend the neck. 3. Secure the larynx laterally between the thumb and forefinger. 4. Locate the cricothyroid membrane by palpating the patient’s neck, starting at the top. The first prominence felt will be the thyroid cartilage, while the second is the cricoids cartilage. The space between these two, noted by the small depression, is the cricoids membrane. This is the puncture site. 5. Firmly hold the device and puncture the cricothyroid membrane at a 90 angle. 6. Check the entry of the needle into the trachea by aspirating air through the syringe. If air is present the needle is within the trachea. 7. Change the angle of insertion to 60 and advance the device forward into the trachea to the level of the stopper. 8. Remove the stopper. Be careful not to advance the device further with the needle still attached. 9. Hold the needle and syringe firmly and slide only the plastic cannula along the needle into the trachea until the flange rests on the neck. Carefully remove the needle and syringe. 10. Secure the cannula with the neck tape, apply the connecting tube to the 15mm connection, and connect the other end to the BVM. Because of the sharp tip and conical shape of the needle, an incision of the skin with the scalpel is not necessary. The opening of the trachea is achieved by dilating through the skin. This reduces the risk of bleeding as only the smallest opening necessary is made Do not delay transport to perform the Cricothyrotomy Justification for utilizing Name of physician that gave the order Time Procedure used to place the trach Verification of placement and technique used Verification of adequacy of ventilation Any change in the patients condition after the procedure DEFIBRILLATION/CARDIOVERSION Level Indication Contraindication Technique Notes Documentation Paramedic Per protocol Per protocol 1. If possible place the patient in an environment away from pooled water or a metal surface under either the patient or the rescuer 2. Apply appropriate conductive materials to hand-held electrodes or use monitor-defibrillator pads 3. Turn on the defibrillator 4. Select the appropriate energy level 5. Charge the defibrillator 6. Place the electrodes on the chest; one just to the right of the upper sternum below the right clavicle and the other just below and to the left of the left nipple, or you may use the anterior/posterior placement. 7. Make sure no personnel are in direct or indirect contact with the patient. 8. If cardioverting assure that the unit is in sync mode 9. Deliver the shock AHA recommends delivery of the first three shocks in succession without stopping to check a pulse if the monitor clearly demonstrates VF Time of shock Who delivered shock Rhythm interpretation pre and post shock with associated strips Level of energy delivered If cardioverting, verification that the current was given in sync mode DRUG ADMINISTRATION Level Indication Contraindication Technique Per specific protocol and drug Standing or verbal order for drug administration Specific to each drug 6 Patient Rights of Drug Administration: Right Patient Right Drug Right Dose Right Time Right Route Right Documentation HOTRAC Regional EMS Guidelines Rev. 5.10 Page 83 Notes Documentation Each route of administration has a slightly different technique. Injections require adequate preparation of the site and aspiration before delivery to assure that the needle is in the intended tissue. IV administration also requires preparation of the site and assured patency of the IV. (Dextrose is not as effective when administered subcutaneously and may be harmful.) Auto injectors require you to press the injector firmly against the injection site for ten seconds to assure complete delivery of medication. Remember: Right Patient, Right Medication, Right Dosage and Right Route Medication errors must be immediately reported to the receiving physician and thoroughly documented Time Who gave the medication Medication given Dosage of medication Route of administration ESOPHAGEAL INTUBATION WITH A MULTILUMEN AIRWAY Level Indication Contraindication Technique Notes Documentation Intermediate, Paramedic Immediate endotracheal intubation cannot be performed Attempts at endotracheal intubation have proven unsuccessful Direct visualization of the larynx is inhibited because of profuse bleeding or vomiting To ensure airway patency in cases of arrest or in cases where the airway requires continuous protection from aspiration. Patients less than 16 years old Patients under 5 feet tall Patients with an intact gag reflex Patients with known esophageal disease Patients who are known alcoholics (May have esophageal varices) Patients who have ingested a caustic substance 1. While maintaining ventilator support, oxygenate the patient with 100% O2 (give at least 4 good ventilations before each attempt) 2. Assemble and check the equipment 3. Position patient with head midline, neutral position. Guard c-spine with trauma patients. 4. Insert the device using the jaw-lift maneuver to the depth indicated by the markings on the tube. The black rings on the tube should be positions between the patient’s teeth. 5. Once the multilumen airway is in place, inflate its pharyngeal cuff with 100 ml of air. This should firmly seal the device in the posterior pharynx behind the hard palate. 6. Inflate the distal cuff with 10 to 15 ml of air. 7. Begin ventilation through the longer blue connector (tube number 1). 8. Auscultate both lungs and the stomach. If you hear bilateral breath sounds, begin ventilation through the shorter clear connector (tube number 2). Confirm bilateral breath sounds and absent gastric sounds after changing the ventilation tube. 9. Continue ventilation with 100% O2, and periodically reassess the airway. The multilumen airway should never be the technician’s “First Choice” airway because it is easier to place than an ET Tube. The multilumen airway should be used in those rare cases where the technician is unable to intubate after repeated attempts. It is impossible to suction tracheal secretions when the airway is in the esophageal position Placement of an endotracheal tube is difficult, but not impossible, with the multilumen airway in place. The pharyngeal cuff must be deflated leaving the esophageal cuff inflated. Do not delay transport for placement of the multilumen airway Each attempt must include the following information: Time Who made the attempt Each successful intubation must also contain the following: Amount of air used to inflate the pharyngeal cuff Amount of air used to inflate the esophageal cuff Verification of placement Which lumen was used to ventilate the patient The tube was secured Verification of placement noting techniques used Verification of placement after the patient is loaded into the ambulance, unloaded from the ambulance, and before being moved from EMS’ stretcher to the emergency department’s bed (preferably by a physician) Any change in the patients condition after the procedure INTRAOSSEOUS INFUSION Level Indication EMT-I, Paramedic Severe illness or injury requiring immediate drugs or fluids, when IV access is impossible or unlikely to be successful. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 84 Contraindication Technique Notes Documentation 1. 2. 3. 4. 5. 6. Available secure IV line Lower-extremity deformity in same bone as insertion site Place the patient in the supine position Put a small towel roll under the knee Prepare the skin over the insertion site Use the flat surface of the proximal medial tibia, medial to the tibial tuberosity on the flat side of the bone. Introduce the IO needle in the skin directed away from the growth plate or pointing toward the foot Pierce the bony cortex with a firm, twisting motion. Use a back and forth twisting motion to enter the marrow space. Do not push hard on the needle. A “pop” may be felt as the needle passes through the bone into the marrow. 7. Remove the stylet and aspirate marrow contents. Keep any bone marrow aspirate for glucose check or for other tests in the ED. Sometimes marrow cannot be aspirated. 8. Confirm correct placement by infusing 10 ml of normal saline without resistance. 9. Attach IV line to the hub and infuse fluids or drugs directly into interosseous space. 10. Secure to the overlying skin with tape. 11. Monitor the calf to ensure that there is no swelling to indicate leakage of fluid. Do not delay transport to place IO. No more than one attempt in the field. Time Who made the attempt Location of attempt Size of catheter used If attempt was unsuccessful, description of why attempt failed Procedure used to verify patency. Type of fluid attached to catheter. Any change in the patient’s condition after the procedure. MUSCULOSKELETAL MOTION RESTRICTION Level Indication Contraindication Technique Notes Documentation ECA, EMT, EMT-I, Paramedic Skeletal instability resulting from musculoskeletal strain, sprain, dislocations or fracture Life threatening conditions must be treated first 1. Assess the “six P’s” Pain, Pallor (pale skin or poor cap refill), Paresthesia (pins and needles sensation), Pulses (diminished or absent), Paralysis (inability to move), Pressure. 2. Assess the distal pulse, motor function and sensation (before and after movement or application of a MMR device.) 3. Inspect and palpate the injured area for DCAP-BTLS: Deformity, Contusions, Abrasions, Penetrations, Burns, Tenderness, Lacerations, Swelling 4. Motion restrict bones or joints in the injured area as well as the joint above and the joint below the injury. 5. Motion restrict open and closed fractures in the same manner covering open fractures to minimize contamination. 6. Stabilize the extremity with gentle, in line traction to a position of normal alignment. Motion restrict a long bone fracture in a comfort position as long as a pulse is present that can easily be splinted. Motion restrict dislocations in a position of comfort ensuring good vascular supply. Motion restrict joints as found; joint injuries are only aligned if there is no distal pulse. 7. Apply cold to reduce swelling and pain 8. Elevate the extremity if possible. The technician should conduct an initial assessment to determine if there is any life threatening conditions. They should care for those conditions first; never overlook musculoskeletal trauma; and never allow a horrible looking, but non-critical, injury to distract from the priorities of care. All skeletal instability should be motion restricted as soon as possible after the ABC interventions are complete. To achieve and maintain musculoskeletal motion restriction any of the following may be utilized as appropriate for the patient condition and situation: Patient’s body – Provides some natural motion restriction when an injury can be secured to a motion restricted body part (i.e. tying the legs together on a backboard where the non-injured leg is secured to the backboard) Board splints Pillow splints – In isolated ankle, foot or hand injuries Pre-formed splints Scoop Traction splints – Traction should be used in closed mid-shaft femur fractures only The “Six P’s” Distal pulse, motor and sensation before and after motion restriction. DCAP-BTLS of the injury and surrounding area. Time motion restriction was applied and by whom Any changes in patient condition post procedure HOTRAC Regional EMS Guidelines Rev. 5.10 Page 85 NASOTRACHEAL INTUBATION Level Indication Contraindication Technique Notes Documentation Intermediate, Paramedic Used in the breathing patient requiring intubation Asthma or pulmonary edema with respiratory failure, where intubation may need to be achieved in a sitting position Patients with severe facial trauma Patients with Apnea Children under 12 years old 1. Assist ventilations if spontaneous respirations are inadequate 2. Choose correct tube size. Limitation is nasal canal diameter 3. Suction should be available and equipment should be checked. 4. Position patient with head midline, neutral position. Guard c-spine with trauma patients. 5. Copiously lubricate the tube with a water based lubricant 6. With gentle steady pressure, advance the tube through the nose to the posterior pharynx. Use right nostril if possible. 7. Keeping the curve of the tube exactly midline, continue advancing slowly 8. There will be a slight resistance just before entering the trachea. Wait for an inspiratory effort before final advance into trachea. Patient may also cough or buck just before breath. 9. Continue advancing until air is exchanging through the tube. 10. Advance about 1 inch further then inflate the cuff. 11. Verify placement with bulb device, by auscultation, and by end tidal CO2 detection. 12. Note proper tube position and tape securely Often nacres are asymmetrical and one side is much easier to intubate. Avoid inducing bilateral nasal hemorrhage by forcing a nasotracheal tube on multiple attempts. Blind nasotracheal intubation is a very “elegant” technique. In the field, the secret of blind intubation is perfect positioning and gentle patience. Each attempt must include the following information: Time Size of tube Which nacre Who made the attempt Each successful intubation must also contain the following: Amount of air used to inflate cuff Centimeter marking at the nacre The tube was secured and with what device Verification of placement noting techniques used. Verification of placement after the patient is loaded into the ambulance, unloaded from the ambulance, and before being moved from EMS’ stretcher to the emergency department’s bed (preferably by a physician) Any change in the patients condition after the procedure NEEDLE CHEST DECOMPRESSION Level Indication Paramedic with special clearance from the medical director Presence of pneumothorax AND any one of the following Severe respiratory distress Tracheal deviation Hypotension Contraindication None Technique 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. Assess the patient to make sure their condition is due to pneumothorax Give the patient high flow O2 and ventilator assistance Determine that one of the indications for emergency decompression is present; then obtain medical direction to perform the procedure Open package and familiarize yourself with the contents Attach connecting tube to Heimlich valve and stopcock to connecting tube. Attach syringe to catheter introducer needle Identify the 2nd or 3rd intercostals space in the midaxillary line on the same side as the pneumothorax. Quickly prepare the area with an antiseptic Insert the catheter into the skin over the border of the 2nd or 3rd rib and direct it just over the top of the rib into the interspace. Insert the catheter through the parietal pleura you should feel a distinct “pop” as you pierce the pleura. Attempt to aspirate air into the syringe. With proper placement you should be able to draw air into the syringe. Remove the needle and leave the plastic catheter in place. Attach the stopcock to the catheter and open the stopcock. Place the blue Molnar disk around the catheter and secure with pull tie. Tape the Molnar disk to the chest HOTRAC Regional EMS Guidelines Rev. 5.10 Page 86 ne Notes Documentation The intercostals artery and vein run around the inferior margin of each rib. Poor needle placement can lacerate one of the vessels The internal mammary artery lies about 1-2 fingerbreadths lateral to the sternum. Always enter the chest in the mid-clavicular line Creation of a pneumothorax may occur if not already present. If your assessment is incorrect, you may give the patient a pneumothorax when you insert the needle into the chest. Laceration of the lung is possible. Poor technique or inappropriate insertion can cause laceration of the lung, causing bleeding and more air leak. Do not delay transport to perform needle chest decompression Supporting clinical signs and symptoms of a pneumothorax that led you to call for procedure. Name of physician that gave order. Time procedure performed Location of insertion site and how it was prepped How air was confirmed to be exiting from the catheter Any change in the patients condition after the procedure OROTRACHEAL INTUBATION Level Indication EMT-I, Paramedic To ensure airway patency in cases of arrest or in cases where the airway requires continuous protection from aspiration. To administer positive pressure when extra fluid is present in the alveoli To administer drugs during resuscitation for absorption through the lungs Contraindication None HOTRAC Regional EMS Guidelines Rev. 5.10 Page 87 Technique 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. Notes Documentation While maintaining ventilator support, oxygenate the patient with 100% O2 (give at least 4 good ventilations before each attempt) Place patient in the supine position if possible, neck slightly extended in the sniffing position. Attempt to maintain in-line spinal mobilization(SMR). Suction should be available and equipment should be checked: tube, cuff, laryngoscope, blade, and light. Have assistant apply gentle cricothyroid pressure to prevent aspiration and to assist visualization of the vocal cords. Insert laryngoscope to the right of midline. Move it to midline, pushing the tongue to the left and out of view. Lift straight up on the blade (no levering) to expose the posterior pharynx Identify the epiglottis: tip of curved blade should sit in vallecula (in front of epiglottis), straight blade should slip over the epiglottis. With further gentle traction to straighten the airway, identify trachea from arytenoids cartilages and vocal cords. Insert tube from right side of mouth, along blade, into the trachea under direct visualization. Advance tube so cuff is 1-1.5cm beyond cords. Inflate tube with 5-10ml of air and hold tube securely in place. Verify placement by visualizing rise and fall of chests or ventilating with BVM and auscultating breath sounds and gastric sounds. Adjust tube position as necessary. Withdraw and re-intubate if tube was placed in the esophagus or withdraw the tube slightly if the right main stem was intubated. Secure the tube with an appropriate device. Re-verify tube placement, and note the tube position. Do not use intubation as the initial means of controlling the airway in cardiac arrest. Oxygenation prior to intubation should be accomplished with a BVM. The use of a stylet is mandatory unless extraordinary circumstances preclude you from doing so. Intubation should take no more than 15-20 seconds to complete: do not loose track of time. If visualization is difficult, stop and ventilate before trying again. Orotracheal intubation can be accomplished in trauma victims if an assistant maintains stabilization and keeps the neck in a neutral position Esophageal intubation is not a critical error. Unrecognized esophageal intubation is. Careful, multiple and documented verification is the key. The soft tissues of the oropharynx are very susceptible to trauma. Liberally use lubrication and a gentle technique to avoid trauma. In cases of head injury premedication with Lidocaine may be appropriate, but do not delay intubation for IV efforts. Do not delay transport for intubation Each attempt must include the following information: Time Size of tube and if it had a cuff Size and type of blade used Who made the attempt Each successful intubation must also contain the following: Amount of air used to inflate cuff Verification of placement before securing tube Centimeter marking at the lips How the tube was secured Re-verification of placement Verification of placement after the patient is loaded into the ambulance, unloaded from the ambulance, and before being moved from EMS’ stretcher to the emergency department’s bed (preferably by a physician) Any change in the patient’s condition after the procedure PACING Level Indication Contraindication Paramedic Per Protocol None HOTRAC Regional EMS Guidelines Rev. 5.10 Page 88 Technique Notes Documentation 1. In patients with excessive body hair and who are conscious clip, rather than shave, any excess body hair to avoid tiny nicks in the skin that can increase pain and skin irritation. 2. Attach the appropriate pads. Place the anterior (-) electrode to the left of the sternum and center as closely as possible to the point of maximal cardiac impulse. Place the posterior (+) electrode on the back, directly behind the anterior electrode to the left of the thoracic spinal column. 3. Attach monitoring leads and adjust the gain up or down until you have an adequate QRS height, which the pacemaker may sense and mark. If this is not successful, select another lead or move the ECG electrodes until sensing occurs. 4. Power the pacemaker module by pressing the “Pacer” soft key and confirm the presence of QRS markers on the ECG. 5. If not already defaulted, set your initial pacing rate to 80 beats per minute. 6. Press the “Start/Stop” button to begin pacing: Observe for vertical pacing spikes. 7. In bradycardic arrest rapidly increase milliamperes in increments until electrical capture occurs or the maximum of 200 mA has been reached. Do not reduce milliamperes once capture occurs. 8. Electrical capture is recognized by the presence of consistent and widened QRS, ST segment and T wave immediately after the pacer spike. 9. In hemodynamically unstable bradycardia slowly increase milliamperes in increments of 5 until electrical capture occurs. Do not lower milliampere setting once electrical capture occurs. 10. Assess the patient for mechanical capture and response to pacing. Pulses should be assessed at the right femoral or right carotid artery to avoid confusion between jerking muscle contractions caused by the pacemaker and a pulse. 11. Closely monitor the patient for any changes. Mechanical and electrical captures are different things. Once electrical capture has taken place increasing the milliamperes will not cause mechanical capture to take place. Pacing is merely a way to guide the heart’s own electrical system. Lack of mechanical capture should be treated like PEA. The only reason to stop the pacer in the field is because of lack of electrical capture. Do not stop the pacer to determine the underlying rhythm. V-Fib and V-Tach would indicate loss of electrical capture and would necessitate immediate defibrillation. Pacing will not stop V-Fib, and we do not perform “overdrive” pacing for V-Tach in the field. Do not “switch out” pacers in the ER. If you have electrical capture you will leave your pacing unit with the patient until an internal pacer or other suitable device can be placed. You may medicate the conscious patient with Midazolam as per protocol. Do not delay the initiation of critically needed pacing to medicate the patient. Time pacing initiated Who initiated pacing Rhythm strips to support decision to initiate pacing Pre and post strips for each setting change i.e.: mA increases or rate increases Strips supporting electrical capture Final energy and rate setting Patient response to treatment PERIPHERAL VENIPUNCTURE Level Indication Contraindication Technique Notes EMT-I, Paramedic Vascular access in any patient who needs or may need fluid resuscitation or medications. Areas where a toxic substance is on the skin Areas distal to injury that may compromise vasculature 1. Prepare all supplies for procedure. 2. Select suitable peripheral site. 3. Apply venous tourniquet, or in cases of EJ cannulation occlude the proximal portion of the vein with a finger. 4. Cleanse the skin over and around the vein with an antiseptic wipe using the outward spiral pattern. Iodine preps are ideal but prepped area has to be allowed to dry to be effective. 5. Insert the needle and catheter, bevel up. When you enter the vein you should feel a “pop” and/or see a blood “flash” in the hub of the catheter. 6. Advance the needle and hub slightly to assure that the end of the catheter is in the vein then advance the catheter over the needle into the vein. 7. Occlude the end of the cannula by holding pressure with a free finger while completely removing the needle. If using a safety IV device assure the device is fully locked. 8. Draw labs using appropriate technique if indicated. 9. Attach appropriate infusion device to catheter. (IV line or saline lock) 10. Release tourniquet. 11. Assure flow. Observe for signs of infiltration. 12. Secure site with tape or other appropriate device. Do not delay transport to obtain IV access. No more than two attempts per technician for IV access. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 89 Documentation Each attempt must include the following information: Time Who made the attempt Location of attempt Size of catheter used If attempt was unsuccessful Each successful venipuncture must also contain the following: If labs were drawn. If not, why not. Type of device or type of fluid attached to catheter. Procedure used to verify patency. Any change in the patients condition after the procedure Level Indication Paramedic with Approval From Medical Director Hypoxic (oxygen saturation <90%, and/or cyanotic) and combative such that orotracheal or nasotracheal intubation is not possible. Age <15. Use cautiously and in reduced dosage in hypotensive or elderly patients Patient who is not vomiting and who can be maintained with BVM or 0 2 mask. Patient who can be intubated without the use of RSI. Short ETA to a fully staffed ED. Patients with penetrating eye injuries. Patients with renal failure. Patients with musculoskeletal disorders (recent stroke, MS). Upper airway obstruction or other problems that are likely to make intubation impossible (major laryngeal trauma, distorted facial or airway anatomy, etc.). Contact Medical Control STEP 1 (a) Pre-oxygenate (avoid gastric distension from excessive pressure). (b) Monitor – IV – Pulse Oximeter. (c) Check all drugs and equipment – have suction ready. (d) Give Norcuron at 0.01 mg/kg slow IVP (defasciculating dose). (e) Give Atropine 0.01 mg/kg IVP (if pulse <70 bpm). (f) Give Lidocaine 0.5 mg/kg IVP (if CHI patient with increased BP). STEP 2 (a) Give Midazolam 2.5-5.0mg slow IVP (up to 10 mg max). (b) Begin Sellick’s maneuver and continue until intubation is completed and ET bulb is inflated. (Sellick’s pressure should be equivalent to the amount of pressure needed to cause pain when you press the tip of your own nose). STEP 3 (a) Give Succinylcholine at 1.5 mg/kg IVP over 30 seconds. (b) Observe 30-45 seconds and intubate. If unable to intubate within 30-60 seconds, use BVM for 60 seconds and retry intubation. (c) Confirm tube placement with visualization of chest rise/fall, ET bulb check, CO2 detector BVM, and increasing pulse oximeter readings. STEP 4 (a) If patient begins to move and resists ventilation enroute, maintain paralysis with Norcuron at 0.1 mg/kg IVP, BUT if transport time is less than 15-20 minutes, maintain paralysis with a repeat dose of 1.0-1.5mg/kg of Succinylcholine. STEP 5 (a) If all efforts to intubate fail, use BVM and monitor pulse oximeter. (b) If unable to ventilate effectively with BVM insert PTL. Remember that Succinylcholine causes: Increased Gastric Pressure (Vomiting) Increased Cranial Pressure (Use caution with head injured patients) Which physician ordered the RSI Who implemented procedure and when All documentation for Intubation (Every attempt) Neurologic status pre and post procedure RAPID SEQUENCE INTUBATION Contraindication Technique Notes Documentation SPINAL MOTION RESTRICTION HOTRAC Regional EMS Guidelines Rev. 5.10 Page 90 Level ECA, EMT, EMT-I, Paramedic Indication Technique 1. 2. 3. 4. 5. 6. 7. Documentation Any patient presenting with a positive or questionable mechanism of injury (MOI) that indicates the potential for spinal injury, and for whom it is not possible to clinically rule-out the need, will have spinal motion restriction (SMR) performed. Patients, for whom SMR is deferred, must meet all exclusionary criteria. Any unstable patient or potentially unstable patient with positive mechanism of injury is to be rapidly extricated with SMR without compromising short scene times. SMR is considered for patient presentation positive for, or suggestive of, traumatic etiology or blunt trauma above the clavicles. These might include, but are not limited to: o Significant injury above the clavicle o Falls (of any height) o Motor vehicle collisions o Direct blunt or penetrating trauma to spine head or neck o Any abrupt accelerating, decelerating, or rotational forces SMR may be omitted when all of the following conditions apply (exclusionary criteria are assessed in order): 1. Patient’s cardiovascular and respiratory systems are stable. 2. Vital Signs are within normal limits 3. Normal peripheral perfusion signs 4. Patient is a reliable historian: 5. Conscious, alert, oriented to person, place, and time. 6. No evidence of acute stress reaction or severe anxiety. 7. No evidence or admission of intoxication or impairment by drug or alcohol use. 8. Patient is between eight (8) and seventy (70) years old. 9. Absence of major painful injuries that could distract the patient’s ability to appreciate pain. 10. If patient can’t cooperate with the assessment they are not considered reliable historians. 11. Normal neurological function in all extremities: 12. Sensory – Pain, pressure, and light touch are present and paresthesias (numbness or tingling) are absent. 13. Motor – Strength is full and symmetrical. 14. Patient denies spine or neck pain. 15. Absence of spine or neck tenderness or deformity elicited upon palpation. 16. Absence of spine or neck tenderness when patient moves head in the coronal, transverse, and sagittal planes. Routine BLS care Determine potential for spinal injury Significant injury above clavicle Positive or questionable mechanism of injury (MOI) Manual spinal stabilization is maintained until need for immobilization is ruled-out Perform initial assessment If patient is stable continue If patient is unstable or has major distracting injuries, stop and implement full SMR If patient is not considered a reliable historian stop and implement full SMR Assess neurological function. If abnormal stop and implement full SMR Assess for spine or neck pain/tenderness If at any point in the following exam pain or tenderness discovered, stop and implement full SMR Patient complains of spine pain Palpate spine for tenderness and/or deformity Direct patient to move head in all three planes of motion SMR decision If patient has NO positive findings on above examination, may omit SMR If patient has ANY positive findings on above examination, or if unable to complete examination, full SMR must be performed Full SMR consists of placing a rigid or semi-rigid C-Collar on the patient, placing the patient onto a long back board utilizing the technique that allows the least movement of the spine, securing the patient to the long back board with straps and securing the patient’s head to the backboard with a cervical motion restriction device. Who made the decision to implement or not implement SMR and a justification for that decision with all pertinent exam findings Names and roles of those assisting with SMR and time of implementation Any changes in pt condition post procedure WOUND CARE Level Indication ECA, EMT, EMT-I, Paramedic Open wounds with or without hemorrhaging HOTRAC Regional EMS Guidelines Rev. 5.10 Page 91 Contraindication Life threatening conditions must be treated first Technique 1. 2. 3. Examine the wound for bleeding, size, depth, and presence of foreign bodies, amount of tissue lost, edema and deformity. Inspect the area around the wound for damage to underlying structures, arteries, nerves, tendons, or muscle. Assess sensory and motor function of the extremity or area Examine the wound for bleeding, size, depth, and presence of foreign bodies, amount of tissue lost, edema and deformity. Inspect the area around the wound for damage to underlying structures, arteries, nerves, tendons, or muscle. 4. Notes Documentation Examine the wound for bleeding, size, depth, and presence of foreign bodies, amount of tissue lost, edema and deformity. Inspect the area around the wound for damage to underlying structures, arteries, nerves, tendons, or muscle. 5. Assess sensory and motor function of the extremity or area 6. Evaluate the perfusion status of the wound and tissue distal to the wound 7. Palpate the injury and associated structures to evaluate capillary refill, distal pulses, tenderness, temperature, edema, and crepitus (if underlying bony injury is suspected) 8. Properly prepare the wound for dressing. Clean the injured surface of gross contaminants by irrigating the wound with (in order of preference) sterile normal saline, or sterile water, or tap water. Do not attempt extensive debridement. 9. Control hemorrhage through direct pressure (you may use an ace bandage over the dressing for this purpose), then elevation, then pressure points, musculoskeletal motion restriction, and very rarely by the use of a tourniquet and only with concurrence of medical control. 10. Apply the appropriate dressing and secure in place with bandages or gauze and tape or tuck the loose ends of the bandage. 11. Assess the tetanus vaccination status of the patient. The goal of wound care is to control hemorrhage, cleanse major contaminants if possible, protect from further contaminants, reduce pain, reduce edema, and protect the technicians from further exposure to blood products. To achieve these objectives the technician may use the above interventions at their discretion. Do not remove an impaled object unless it causes an airway compromise. Move the impaled object as little as possible. Sometimes it is necessary to manipulate the impaled object if it is necessary to shorten the object for extrication or for patient transportation. In cases of avulsion the area should be cleaned of gross contaminants with a sterile saline irrigation, and the avulsed tissue should be folded back to its normal position. Appropriate bandaging should continue from that point. In cases of amputation wrap the amputated part in gauze moistened with saline solution, seal the part in a plastic bag and place the sealed bag on crushed ice. If crushed ice is not available place the bag between two, or more, cold packs. Do not delay transport to find the amputated part. It may be necessary to solicit the assistance of law enforcement or other health care providers in the search for the amputated part. Never delay transportation of a multiple trauma patient because of a prolonged wound evaluation. Assessment of size, depth, location, and extent of contamination of wound as well as any possible damage to underlying structures. Assessment of sensory, motor and perfusion status of the extremity or affected area before and after application of a dressing. Assessment of cap refill, distal pulses, tenderness, temperature, edema and crepitus of the injury and surrounding structures. Method used to prepare the wound for dressing. Techniques used to control hemorrhage and rationale for proceeding to each different level. Type of dressing used (Sterile, non-sterile, occlusive, trauma pad, abd pad, or etc) Tetanus status of the patient. When wound care was performed and by whom Any changes in patient condition post procedure HOTRAC Regional EMS Guidelines Rev. 5.10 Page 92 Airway Management General Principles Stepwise procedures for obtaining control of the airway in medical situations have been well accepted and standardized by AHA protocol as well as practical clinical experience. Use of nasopharyngeal airways in lightly comatose patients who still require some support for a lax tongue is encouraged. Nasotracheal intubation, particularly in breathing patients who require intervention, is also encouraged. When is active control of the airway needed? In many instances, the maximally invasive form of airway management is chosen because of incorrect judgments about "impending" respiratory arrest. Especially with head injuries, this is hard to predict, and an irregular-breathing pattern may represent chaotic breathing rather than impending arrest. On the other hand, despite the obvious risks of active airway management, the risks of inadequate oxygenation are even greater. Both under treatment and overtreatment may be costly to the patient, but it is better to err on the side of aggressive airway management to achieve adequate oxygenation. The unsolved problem of emergency airway management is what to do with the patient who requires active airway management and in whom there exists great potential for (or actual presence of) a cervical spine injury. Clearly no one wishes to save a life at the expense of producing a quadriplegic. Nevertheless, if the patient is in full trauma arrest, to what avail is it to save the spinal cord function, if the patient is vegetated or dies because of prolonged attempts to perform difficult operative procedures with inadequate experience? Currently, the best method to control the airway is to intubate orally with an assistant maintaining stabilization (digital intubation, also with stabilization, is an alternative.) In a non-arrested patient, nasotracheal intubation is an excellent alternative if there is no mid-face trauma. Technical competence requires good training, adequate practice, and compulsive attention to detail to ensure safe and effective performance of any procedure. Cricothyrotomy remains the only effective alternative for a small number of patients who have injuries that preclude routine airway procedures. The following guidelines are recommended as a guide for approaching difficult medical and trauma airway problems. They assume that the responder is skilled in the various procedures, and will need to be modified according to training level. Advanced procedures should only be attempted if simpler ones fail and if the technician is qualified. Individual cases may require modification of these guidelines. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 93 Airway Management Algorithm ECA/EMT INTERMEDIATE PARAMEDIC If necessary open airway using most efficient appropriate manual maneuver. If ventilations are weak or absent assist ventilation If complete obstruction or partial with poor air exchange follow FBAO protocol Assess oxygenation; use supplemental O2 as indicated Suctioning as needed Choose least invasive method to maintain airway patency during transport If necessary open airway using most efficient appropriate manual maneuver. If ventilations are weak or absent assist ventilation If complete obstruction or partial with poor air exchange follow FBAO protocol Assess oxygenation; use supplemental O2 as indicated Suctioning as needed Choose least invasive method to maintain airway patency during transport In cases of arrest or if airway requires continued protection from aspiration intubate If after 2 attempts intubation is unsuccessful another qualified technician may attempt If after 4 total intubation attempts follow Cricothyrotomy protocol If necessary open airway using most efficient appropriate manual maneuver. If ventilations are weak or absent assist ventilation If complete obstruction or partial with poor air exchange follow FBAO protocol Assess oxygenation; use supplemental O2 as indicated Suctioning as needed Choose least invasive method to maintain airway patency during transport In cases of arrest or if airway requires continued protection from aspiration intubate If after 2 attempts intubation is unsuccessful another qualified technician may attempt If after 4 total intubation attempts follow Cricothyrotomy protocol If unable to intubate or ventilate and qualified, may follow trach protocol after contacting medical control HOTRAC Regional EMS Guidelines Rev. 5.10 Page 94 Foreign Body Airway Obstruction (FBAO) Early recognition of airway obstruction is the key to a successful outcome. Mild Airway Obstruction: Good air exchange, patient is responsive and can cough forcefully. May wheeze between coughs. As long as good air exchange continues, encourage the patient to continue spontaneous coughing and breathing efforts. DO NOT interfere with the patient’s own attempts to expel the foreign body. Severe Airway Obstruction: Poor to no air exchange, with weak, ineffective or no cough at all. High pitched noise while inhaling or no noise at all. Increased respiratory effort or difficulty. Possible cyanosis around lips, and unable to speak. Clutching the neck with hands (universal sign of choking). Unable to move air. ECA/EMT INTERMEDIATE PARAMEDIC If patient is conscious and > 1 year of age perform Abdominal Thrusts (standing) until object is expelled or patient becomes unresponsive. If patient is responsive and is < than 1 year of age (infant). Place the infant across your lap with head down and alternate between 5 back blows and 5 chest thrusts until the object is dislodged or the infant becomes unresponsive. If the patient is found unresponsive or becomes unresponsive, place the patient in the prone position on the floor or on a hard surface. Perform ABC’s. If the patient is not breathing open airway and look for the object. If object can be seen, remove it using your fingers. DO NOT perform a blind finger sweep. If patient begins breathing place them in the recovery position and administer high-flow O2, assess vital signs and monitor until ALS personnel arrive. or transport If you do not see the object attempt 2 rescue breaths and if airway remains obstructed begin CPR until ALS personnel arrive, or transport. Follow CPR/AED protocol, consider ALS Intercept If patient is conscious and > 1 year of age perform Abdominal Thrusts (standing) until object is expelled or patient becomes unresponsive. If patient is responsive and is < 1 year of age (Infant), place the infant across your lap with head down and alternate between 5 back blows and 5 chest thrusts until the object is dislodged or the infant becomes unresponsive. If the patient is found unresponsive or becomes unresponsive, place the patient in the prone position on the floor or on a hard surface. Perform ABC’s. If patient is not breathing open airway and visualize with laryngoscope. If object can be seen, remove it using your fingers. DO NOT perform a blind finger sweep. If patient begins breathing place them in the recovery position, administer high flow 02, assess vital signs, saline lock, monitor until Paramedic arrives, or transport. If you do not see the object attempt 2 rescue breaths and if airway remains obstructed begin CPR until Paramedic arrives, or transport. Follow CPR/AED protocol, consider Paramedic Intercept If patient is conscious and > 1 year of age perform Abdominal Thrusts (standing) until object is expelled or patient becomes unresponsive. If patient is responsive and is < 1 year of age (infant), place the infant across your lap with head down and alternate between 5 back blows and 5 chest thrusts until the object is dislodged or the infant becomes unresponsive. If the patient is found unresponsive or becomes unresponsive, place the patient in the prone position on the floor or on a hard surface. Perform ABC’s. If patient is not breathing open airway and visualize with laryngoscope. If object can be seen, remove it using magill forceps. DO NOT perform a blind sweep. If patient begins breathing place them in the recovery position, administer high flow 02, assess vital signs, saline lock, EKG and transport. If you do not see the object attempt 2 rescue breaths and if airway remains obstructed begin CPR and transport. Follow cardiac arrest protocol Consider Cricothyrotomy to establish patent airway. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 95 COMMUNICATIONS GUIDELINES Communications with Base Hospital are accomplished by telephone or radio. It is best to contact the receiving facility as soon after initiation of transport as possible. Basic Radio Procedures All communications should be accomplished using plain English. Organize information before initiating contact. All Transmissions are to be kept short and information must be as precise as possible. The sequence should always be as follows: Identify unit calling then name of individual First Statement (Category 1 & 2 Trauma Patients) – deliver information as quickly as possible Urgency Code and whether patient is trauma victim Give patient’s GCS Age, sex, and level of consciousness of patient expressed with AVPU scale Chief complaint in 10 words or less ETA Vital Signs Second Statement (Category 3 & 4 Trauma Patients) - in addition to information above. Brief history relating to the chief complaint Significant physical findings related to the chief complaint EKG transmission if monitoring and appropriate for the situation Brief summary of interventions, treatments in the field to this point Response from Medical Control Acknowledge Further questions Orders Lastly, can give additional information, medications, etc. Communication System failures If you are unable to contact the hospital per radio, you may relay information through dispatch. Dispatch will then contact the hospital ED by landline to give information in the same format as described above. If neither of these modes is operational you can try to contact the other hospital base station. They can relay message by landline. Base Station Responsibility For Communications The Emergency Physician on duty or his designated alternate (Nurse) should be immediately available at all times for providing medical direction to the field in all communications. Communications with the field shall be completed in a timely organized manner. All orders from the Base Station must comply with the EMS protocols for the field personnel HOTRAC Regional EMS Guidelines Rev. 5.10 Page 96 ABDOMINAL PAIN / NAUSEA & VOMITING HISTORY Past medical history. Past surgical history. Meds. Onset & duration of pain (or other symptoms). Pain severity (1-10). Radiation of pain. Character of pain (cramping, dull, sharp, etc.). Fever. Time of last meal. Improvement or worsening with food or activity. Last bowel movement/emesis. Menstrual history. SIGNS & SYMPTOMS Pain. Tenderness. N/V. Diarrhea. Dysuria. Constipation. Evidence of blood in stool (melena). Vaginal bleeding/discharge. Pregnancy. Altered LOC/syncope. Weakness. General or orthostatic hypotension. DIFFERENTIALS Liver (hepatitis, CHF). Peptic ulcer disease/gastritis. Gallbladder disease. MI. Pancreatitis. Kidney stones. Abdominal aneurysm. Appendicitis. Bladder/prostate disorder. Pelvic (PID, ectopic pregnancy, ovarian cyst). Spleen enlargement. Diverticulitis. Bowel obstruction. Gastroenteritis (infectious). PEARLS: Document the mental status and V/S’s prior to any administration of Phenergan. Check blood glucose on all diabetic pts. ABD pain in women of childbearing years should be treated as an ectopic pregnancy until proven otherwise. Discourage the use of antacids in pts. with renal disease. Epigastric abdominal pain should be considered as a possible MI. Appendicitis presents with vague, peri-umbilical pain that migrates to the RLQ with time. Abdominal aneurysms should be considered in pts. >50 who have ABD pain. Never delay transport of pts. with abdominal pain even if they appear stable. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 97 EMT/ECA INTERMEDIATE PARAMEDIC Check ABC’s Assess oxygenation; use supplemental O2 as indicated Allow position of comfort. If actively vomiting provide emesis bag or lay on side to keep airway open. Suction PRN Transport Consider ALS intercept Check ABC’s Assess oxygenation; use supplemental O2 as indicated Allow position of comfort. If actively vomiting provide emesis bag or lay on side to keep airway open Suction PRN Saline Lock. Consider IV @ TKO with NS if pt. has been vomiting excessively. Bolus 20cc/kg if hypotensive Transport Consider ALS intercept Check ABC’s Assess oxygenation; use supplemental O2 as indicated Allow position of comfort. If actively vomiting provide emesis bag or lay on side to keep airway open. Suction PRN Saline Lock. Consider IV @ TKO with NS if pt. has been vomiting excessively. Bolus 20cc/kg if hypotensive Consider administering antiemetic to control vomiting or dry heaves. .Attach EKG and treat dysrhythmias per protocol. Transport HOTRAC Regional EMS Guidelines Rev. 5.10 Page 98 ALLERGIC REACTION / ANAPHYLAXIS ASSESSMENT Usually history of exposure to allergen, often oral ingestion. May be from insect sting or drug ingestion. Penicillin is a very common allergen. Patient usually has severe itching, hives, generalized Urticaria. May have stridor, facial edema, swelling of tongue ECA/EMT MANAGEMENT WITH O2 & AIRWAY ADJUNCTS INTERMEDIATE PARAMEDIC Check ABC’s Assess oxygenation; use supplemental O2 as indicated Trendelenburg’s Position if BP < 100 systolic Administer Epi Pen as appropriate Transport HOTRAC Regional EMS Guidelines Rev. 5.10 Check ABC’s Assess oxygenation; use supplemental O2 as indicated Saline Lock If BP < 100 systolic, IV Normal saline and 250 cc bolus. Reevaluate and may repeat 250 cc bolus for BP < 100 systolic Administer Epi Pen as appropriate Transport Check ABC’s Assess oxygenation; use supplemental O2 as indicated Adult Dystonic Reaction: Diphenhydramine 25 mg slow IV or deep IM Pediatric Dystonic Reason: Diphenhydramine 1 mg/kg slow IV or deep IM (25mg max) Saline Lock If BP < 100 systolic, IV Normal saline and 250 cc bolus. Reevaluate and may repeat 250 cc bolus for BP < 100 systolic Cardiac Monitor If persistent BP < 100 or LOC or respiratory distress, Epinephrine, 0.3-0.5 SQ. (May repeat q 5 minutes if long transport) Adult Anaphylaxis: Diphenhydramine 50 mg slow IV or deep IM (Pediatric is given 1-2 mg/kg up to 50 mg) Contact Medical Control Transport Page 99 ALTERED LEVEL OF CONSCIOUSNESS General Considerations ASSESSMENT A. Alert V. Verbal stimuli response (Yes or no, appropriate or not) P. Painful Stimuli response (Yes or no, appropriate or not) U. Unresponsive SPECIFIC ASSESSMENT Pupil size and reactivity. Equal or not? Vital Signs including orthostatic vital signs Skin color, temperature, moist or dry. Note odor of breath Focal neurologic deficits, if any, and any evidence of trauma Additional information (Medic alert tags) MANAGEMENT WITH O2 & AIRWAY ADJUNCTS ECA/EMT INTERMEDIATE PARAMEDIC Check ABC’s Assess oxygenation; use supplemental O2 as indicated Full Spinal Motion Restriction PRN High flow O2 Treat any injuries Perform Dextrostix If Dextrostix < 50 give Instant Glucose if patient can protect airway Transport HOTRAC Regional EMS Guidelines Rev. 5.10 Check ABC’s Assess oxygenation; use supplemental O2 as indicated Full Spinal Motion Restriction PRN High flow O2 Treat any injuries Perform Dextrostix Saline Lock If Dextrostix < 50, Start IV of normal saline & give D50, 25 gm IV. If no IV access, Instant Glucose if patient can protect airway Transport Check ABC’s Assess oxygenation; use supplemental O2 as indicated Full Spinal Motion Restriction PRN High flow O2 Treat any injuries Perform Dextrostix Saline Lock If Dextrostix < 50, Start IV of normal saline & give D50, 25 gm IV. Thiamin 100 mg IV PRN should be administered first if suspected alcohol abuse. If no IV access, Instant Glucose if patient can protect airway; If not, Glucagon I mg IM Cardiac Monitor Narcan 2.0 mg IV PRN Transport Page 100 ALTERED LEVEL OF CONSCIOUSNESS Seizure Activity ECA/EMT MANAGEMENT WITH O2 & AIRWAY ADJUNCTS INTERMEDIATE PARAMEDIC Check ABC’s Assess oxygenation; use supplemental O2 as indicated Protect patient until seizure ends and maintain quiet environment Follow general Altered LOC procedures Transport in lateral recumbent position If patient refuses transport do all possible to not allow to remain alone or drive Check ABC’s Assess oxygenation; use supplemental O2 as indicated Protect patient until seizure ends and maintain quiet environment Follow general Altered LOC procedures Saline lock & start IV Normal saline if patient actively seizing Transport in lateral recumbent position If patient refuses transport do all possible to not allow to remain alone or drive Check ABC’s Assess oxygenation; use supplemental O2 as indicated Protect patient until seizure ends and maintain quiet environment Follow general Altered LOC procedures Saline lock & start IV normal saline if patient actively seizing Monitor & treat any Dysrhythmia per protocols If persistent Seizures and not an apparent febrile seizure, Diazepam 5 mg IV and notify Medical Control If OB patient (eclampsia) near term and BP > 140/90, give Magnesium Sulfate (mix 4 gm in a 50cc bag of D5W & infuse over 20 minutes Transport in lateral recumbent position If patient refuses transport do all possible to not allow to remain alone or drive Persistent Seizures refers to seizures lasting more than 5 minutes or those occurring repeatedly (More than twice). This is not the same as the definition of status epilepticus. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 101 ALTERED LEVEL OF CONSCIOUSNESS Syncope/Fainting EMT/ECA MANAGEMENT WITH 02 & AIRWAY ADJUNCTS INTERMEDIATE PARAMEDIC Check ABC’s Assess oxygenation; use supplemental O2 as indicated Full Spinal Motion Restriction if suspected head or neck trauma Follow general Altered LOC Procedures Treat any injuries Transport HOTRAC Regional EMS Guidelines Rev. 5.10 Check ABC’s Assess oxygenation; use supplemental O2 as indicated Full Spinal Motion Restriction if suspected head or neck trauma Follow general Altered LOC Procedures Treat any injuries Saline lock Systolic BP < 100 then IV normal saline & fluid challenge with 250 cc & repeat evaluation. Repeat Bolus if Systolic BP < 100 Transport Check ABC’s Assess oxygenation; use supplemental O2 as indicated Full Spinal Motion Restriction if suspected head or neck trauma Follow general Altered LOC Procedures Treat any injuries Saline lock If Systolic BP < 100 then IV normal saline & fluid challenge with 250 cc & repeat evaluation. Repeat Bolus if Systolic BP < 100 Cardiac Monitor & treat dysrhythmia per protocols Transport Page 102 ALTERED LEVEL OF CONSCIOUSNESS With Neuro Signs ASSESSMENT Localized weakness, paralysis, paresis and unilateral facial weakness as well as slurred speech, can all be signs of a stroke syndrome. Can occur sometimes without an altered LOC ECA/EMT MANAGEMENT WITH 02 & AIRWAY ADJUNCTS INTERMEDIATE PARAMEDIC Check ABC’s Assess oxygenation; use supplemental O2 as indicated Full Spinal Motion Restriction if suspected head or neck trauma Treat any injuries Follow general Altered LOC procedures Transport HOTRAC Regional EMS Guidelines Rev. 5.10 Check ABC’s Assess oxygenation; use supplemental O2 as indicated Full Spinal Motion Restriction if suspected head or neck trauma Treat any injuries Follow general Altered LOC procedures IV Saline lock Transport Check ABC’s Assess oxygenation; use supplemental O2 as indicated Full Spinal Motion Restriction if suspected head or neck trauma Treat any injuries Follow general Altered LOC procedures IV Saline lock Monitor & Treat any Dysrhythmia per protocols Transport Page 103 SUSPECTED ACUTE MYOCARDIAL INFARCTION (TO BE USED FOR CHEST PAIN OF SUSPECTED CARDIAC ORIGIN) ASSESSMENT Chest pain lasting more than 5-10 minutes Chest pain radiating to neck or jaw and/or arm Diaphoresis, Dyspnea, nausea Character of pain crushing, heavy, squeezing Abdominal pain can also be of cardiac origin ECA/EMT INTERMEDIATE PARAMEDIC Assess ABC's & Relieve Anxiety O2 per high flow mask Screen for Thrombolytic Therapy & notify Medical Control as early as possible If patient not allergic or history of active ulcer disease, 4 chewable baby aspirin (or equivalent) even in absence of active chest pain *1 NTG SL 0.4 mg if BP 100 systolic. Repeat NTG x 2 PRN if BP remains 100 systolic Transport Patient should be treated at hospital as soon as possible Assess ABC's & Relieve Anxiety O2 per high flow mask Screen for Thrombolytic Therapy & notify Medical Control as early as possible If patient not allergic or history of active ulcer disease, 4 chewable baby aspirin (or equivalent) even in absence of active chest pain 1 NTG SL 0.4 mg if BP 100 systolic. Repeat NTG x 2 PRN if BP remains 100 systolic Saline Lock No more than 2 IV attempts Transport. Patient should be treated at hospital as soon as possible Assess ABC's & Relieve Anxiety O2 per high flow mask Screen for Thrombolytic Therapy & notify Medical Control as early as possible If patient not allergic or history of active ulcer disease, 4 chewable baby aspirin (or equivalent) even in absence of active chest pain 1 NTG SL 0.4 mg if BP 100 systolic. Repeat NTG x 2 PRN if BP remains 100 systolic Saline Lock . No more than 2 IV attempts Monitor & treat any Dysrhythmia per protocols If chest pain persists & Systolic BP 100 then MS 2-4 mg IV Transport. Patient should be treated at hospital as soon as possible *May NOT be performed by ECA HOTRAC Regional EMS Guidelines Rev. 5.10 Page 104 BRADYCARDIA ASSESSMENT Refer to Acute MI/Chest Pain Guideline SPECIFIC ASSESSMENT Prolonged capillary refill, diaphoresis, cyanosis Chest pain, dyspnea, LOC, systolic BP < 90, shock, CHF? IF THE PATIENT IS HEMODYNAMICALLY STABLE FOLLOW CHEST PAIN GUIDELINES FOR THE STABLE PATIENT IF THE PATIENT IS HEMODYNAMICALLY UNSTABLE AND HEART RATE < 60 EMT/ECA INTERMEDIATE PARAMEDIC Check ABC’s Assess oxygenation; use supplemental O2 as indicated O2 high flow Mask Assist ventilation PRN Transport HOTRAC Regional EMS Guidelines Rev. 5.10 Check ABC’s Assess oxygenation; use supplemental O2 as indicated O2 high flow Mask Assist ventilation PRN Intubate PRN IV normal saline TKO rate Transport Check ABC’s Assess oxygenation; use supplemental O2 as indicated O2 high flow Mask Assist ventilation PRN Intubate PRN IV normal saline TKO rate Monitor with pacing pads if available Atropine 0.5 mg IV q3 min. up to 0.04 mg/Kg Pace at lowest voltage at which capture takes place. Consider Midazolam 2.5-5 mg IV in the awake patient Contact Medical Control may request Dopamine 5-10g/Kg/min if hypotensive Transport Page 105 HYPERTENSIVE CRISIS ASSESSMENT Refer to Chest Pain Guideline SPECIFIC ASSESSMENT Check BP in both arms Signs or symptoms of over hydration? Consider head trauma To qualify as Hypertensive Crisis, BP is usually elevated to over 120 mm Hg. Diastolic. In addition there must be end organs symptoms and/or signs present. These can be manifested by: Severe Headache with Altered LOC but usually not lateralizing signs Angina type chest pain Congestive heart failure or pulmonary edema. These patients may have BP lowered to about 110 mm Hg to 100 mm Hg diastolic but not below! For patients with a stroke with lateralizing signs, we must not lower the BP below 110 diastolic and most of the time stroke patients do not need to have their BP lowered acutely ECA/EMT INTERMEDIATE PARAMEDIC Check ABC’s Assess oxygenation; use supplemental O2 as indicated High flow O2 & assist ventilation PRN Transport Check ABC’s Assess oxygenation; use supplemental O2 as indicated High flow O2 & assist ventilation PRN Saline lock Transport Check ABC’s Assess oxygenation; use supplemental O2 as indicated High flow O2 & assist ventilation PRN Saline lock Cardiac Monitor As long as diastolic BP > 110, 1 NTG 0.4 mg SL q 5 min up to 3 doses. Contact Medical Control If BP remains > 110 diastolic & long transport time, request Labetalol 20 mg IV over 2 min Transport HOTRAC Regional EMS Guidelines Rev. 5.10 Page 106 HYPOTENSION/SHOCK (Hypovolemic) ASSESSMENT Assess ABC's and note presence or absence of venous distention, rales, pulse volume, capillary refill. Measure BP and repeat BP measurements during treatment/transport phase. Try to decide if the problem is a volume problem (flat neck veins, dehydrated, bleeding, poor capillary refill, dry mucous membranes) or a pump problem (distended neck veins, rales, pulmonary edema, irregular rhythms) ECA/EMT INTERMEDIATE PARAMEDIC Check ABC’s Assess oxygenation; use supplemental O2 as indicated O2 per high flow mask Assist ventilation PRN Place in Trendelenburg’s position (head down/feet up) Transport Check ABC’s Assess oxygenation; use supplemental O2 as indicated O2 per high flow mask Assist ventilation PRN Place in Trendelenburg’s position (head down/feet up) IV normal saline If Systolic BP <90 mm Hg then bolus of 250cc & repeat BP Continue monitoring breath sounds Contact Medical Control Repeat fluid bolus PRN Transport Check ABC’s Assess oxygenation; use supplemental O2 as indicated O2 per high flow mask Assist ventilation PRN Place in Trendelenburg’s position (head down/feet up) IV normal saline If Systolic BP < 90 mm Hg then bolus of 250cc & repeat BP Continue monitoring breath sounds Contact Medical Control Repeat fluid bolus PRN If long transport time, request Dopamine Transport HOTRAC Regional EMS Guidelines Rev. 5.10 Page 107 The following cardiac guidelines are for ECA/EMT and Intermediate. The Paramedic Guidelines begin on page . Apneic & Pulseless ASSESSMENT Refer to Acute MI/Chest Pain Guideline SPECIFIC ASSESSMENT Consider the possibility of a Trauma Code situation. Does the patient meet DNR criterion? Hypovolemia is first consideration in trauma, and drug therapy is of little value in that case. Check leads in two positions to confirm Asystole ECA/EMT INTERMEDIATE Assess ABC’s AED CPR Transport Assess ABC’s CPR Intubate if possible IV normal saline TKO Transport HOTRAC Regional EMS Guidelines Rev. 5.10 Page 108 TACHYCARDIA – Unstable with Pulses ASSESSMENT If Ventricular rate > 150/min. prepare for immediate Cardioversion. May give brief trial of medication based on the type of Dysrhythmia Immediate Cardioversion seldom needed for rates < 150/min. ECA/EMT INTERMEDIATE Check ABC’s Assess oxygenation; use supplemental O2 as indicated O2 high flow mask Assist ventilation PRN Transport Check ABC’s Assess oxygenation; use supplemental O2 as indicated O2 high flow mask Assist ventilation PRN Intubate PRN IV normal saline TKO rate Transport HOTRAC Regional EMS Guidelines Rev. 5.10 Page 109 TACHYCARDIA - Stable STABLE BUT SYMPTOMATIC ECA/EMT INTERMEDIATE Check ABC’s Assess oxygenation; use supplemental O2 as indicated Transport Check ABC’s Assess oxygenation; use supplemental O2 as indicated Saline lock Transport HOTRAC Regional EMS Guidelines Rev. 5.10 Page 110 VENTRICULAR FIBRILLATION/PULSELESS V. TACH (VF/VT) ASSESSMENT Refer to Chest Pain Guideline SPECIFIC ASSESSMENT Consider possibility of Trauma Code situation Check EKG leads & Patient Level of Consciousness ECA/EMT INTERMEDIATE Assess ABC’s Apply leads & follow AED Protocol CPR if pulse less Transport Assess ABC’s Apply leads & follow AED Protocol CPR Intubate if possible IV normal saline TKO Transport HOTRAC Regional EMS Guidelines Rev. 5.10 Page 111 CARDIAC EMERGENCIES (PARAMEDIC LEVEL CARE) TACHYCARDIA (narrow & wide complex – with a pulse / non-arrest) HISTORY Estimated duration of the tachycardia (if known). ASHD A-fib, tachydysrhythmias (& previous treatment for). WPW. Smoker. Implanted defibrillator (AICD). Meds. Previous MI’s. Cardiovascular surgery. Digitalis toxicity. SIGNS & SYMPTOMS Chest pain. Shortness of breath N/V. Skin: diaphoresis, cyanosis, pallor, flushed, cool, clammy, etc. Pulse regularity. Weakness, syncope. Orthostatic hypotension. DIFFERENTIALS Rate due to compensation for dehydration and/or resp. distress. Drug-induced tachycardia. Anxiety-induced tachycardia. Fever, sepsis. PEARLS The cardiac monitor & 02 kit must go in to the pt. on ALL calls with possible cardiac disorders (i.e. altered LOC, chest pain, palpitations, shortness of breath, etc.) Priority of treatment: Pain-Rate-Rhythm-BP. Treat the patient – not the monitor. Amiodarone contraindicated for patients taking Coumadin (see drug description) Do NOT electrically cardiovert anyone on digitalis (Lanoxin, Digoxin) without consulting medical control first. An unstable pt. is one who is defined by a systolic BP <80, signs & symptoms of shock, and/or a seriously depressed LOC. Adenosine must be pushed as rapidly as possible followed with an immediate flush of saline. Use large vein (if available). Be prepared for a brief run (10 sec or greater) of asystole after giving Adenosine. The effect of Adenosine may be short-lived in patients with WPW (Wolff-Parkinson-White syndrome) and reoccurrence is common. Symptomatic tachycardia does NOT equal unstable tachycardia. Assess the LOC, BP, & perfusion status closely to determine stability. If performing synchronized cardioversion – make sure sync control is turned on for EACH attempt. Paced rhythms may resemble wide-complex tachycardia and spikes may be inconspicuous. Always ask about allergies. CONDITION Narrow Complex (regular) SVT (HR > 150 bpm) Asymptomatic & Stable (systolic BP > 80, weakness, no altered LOC). ACTIONS High flow 02. Monitor ECG closely. IV (saline lock). Adenosine 6 mg rapid IVP. 12 mg may be given 1-2 minutes after 1st dose if SVT persists x 2. Not to exceed 18 mg. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 112 TACHYCARDIA (continued) (narrow & wide complex – with a pulse / non-arrest) Unstable (systolic BP < 80, poor LOC, dyspnea, chest pain, poor perfusion, etc.) Narrow complex tachycardia -irregular with HR > 150 (A-fib/flutter w/RVR) Asymptomatic & Stable (Systolic BP > 80, no weakness or altered LOC). Symptomatic or Unstable (Systolic BP < 80, Altered LOC, weakness, chest pain, S&S of poor perfusion). High flow 02. Monitor ECG closely. IV (saline lock). Consider sedation (Midazolam, Diazepam, etc.) Synchronized cardiovert @ 100 J, 200J, 300 J, 360 J. Wide-complex (Ventricular) Tachycardia Stable (systolic BP > 80, weakness, no altered LOC). High flow 02. IV (saline lock). Transport & monitor EKG closely Consider administering medication to control rate (Diltiazem or B-blocker) Consult with Medical Control High flow 02. IV (saline lock) Administer Diltiazem 5-10 mg IVP over 2 minutes. Contact Medical Control DO NOT cardiovert unless confirmed new onset < 24 hours. If confirmed new onset synchronize cardiovert @ 50J, 100J, 200J, 300J, 360J Unstable (systolic BP < 80, poor LOC, dyspnea, chest pain, poor perfusion, etc.) Torsades de pointes HOTRAC Regional EMS Guidelines Rev. 5.10 High flow 02. Monitor ECG closely. IV (saline lock). Administer Lidocaine 1.0- 1.5 mg/kg IVP or Amiodarone 150mg IV over 10 min. Second dose of Lidocaine can be administered at ½ dose not to exceed 3mg/kg. Amiodarone may be repeated PRN at 150 mg over 10 min. High flow 02. Monitor ECG closely. IV (saline lock). Consider sedation Synchronized cardiovert @ 100 J, 200J, 300 J, 360 J. High flow 02. Monitor ECG closely. IV (saline lock). Administer Magnesium 1 – 2 grams over 5 – 15 minutes. Page 113 CARDIAC ARREST V-FIB / PULSELESS V-TACH HISTORY Downtime. Bystander CPR. Implanted defibrillator (AICD). Meds. Cardiovascular and/or other significant medical history. Substance abuse. SIGNS & SYMPTOMS Apnea, pulselessness. DIFFERENTIALS Hypoxemia. Hypoglycemia Hypovolemia. Hypokalemia. Hyperkalemia. Hypothermia Tension pneumothorax. Cardiac Tamponade. Trauma Thrombosis (pulmonary/coronary embolism). PEARLS If CPR is being applied upon arrival – have continued until ECG ‘quick-look’ is available. Half-dose Lidocaine on all pts. >70, BP <90, or with liver dysfunction (bolus & infusion). Apply 02 at highest flow to BVM as early on as possible. Flush IV line after each drug. Avoid any interruption of CPR, except for pre intubation ventilation, defibrillation and rhythm check. CPR should be performed for 2 minutes after each defibrillation without checking pulse or rhythm. At any time the rhythm changes – go to the appropriate guideline. At any time a pulse reoccurs – go to post-resuscitation guideline. CONDITION Unconsciousness. Apnea. No pulse. V-Fib (or pulse less V-Tach) ACTIONS Confirm Give 2 initial breaths with BVM (or other ventilation device). If unknown down time or greater than 2-3 minutes, begin CPR ( 30 compressions & 2 ventilations for 2 minutes). Quick-look to identify rhythm if monitor is available. First Defib @ 360 J (monophasic) 200 J (biphasic). Continue CPR Place ET or other airway device & confirm for correct placement. IV (saline or saline lock). Epi 1mg IVP (repeat Q3-5 min) If no IV is available Epi x 2 via ET Second Defib @ 360 joules (mono) 300 (biphasic) Continue CPR x 2 minutes Administer Lidocaine 1mg/kg IVP (repeat Q5 HOTRAC Regional EMS Guidelines Rev. 5.10 min to a max of 3mg/kg) or 300 mg Amiodarone IVP. All further Defib @ 360 joule Continue CPR x2 minutes between drugs and defibrillations. Page 114 ASYSTOLE HISTORY Downtime. Bystander CPR. Implanted defibrillator SIGNS & SYMPTOMS Apnea, pulselessness. (AICD). Meds. Cardiovascular and/or other significant medical history. Substance abuse. DIFFERENTIALS Hypoxemia. Hypovolemia. Hypokalemia. Hyperkalemia. Hypothermia. Toxins Tension pneumothorax. Tamponade. Thrombosis (coronary or pulmonary embolism). Thrombosis (MI). Trauma Acidosis PEARLS The cardiac monitor & 02 kit must go in to the pt. on ALL calls with possible cardiac disorders (i.e. altered LOC, chest pain, palpitations, shortness of breath, etc.). If CPR is being applied upon arrival – have continued until ECG ‘quick-look’ is available. If downtime >20 min – consider DNR (refer to DNR guideline). This must be well documented. Apply 02 at highest flow to BVM as early on as possible. Flush IV line after each drug. At any time the rhythm changes – go to the appropriate guideline. At any time a pulse reoccurs – go to post-resuscitation guideline. CONDITION Unconsciousness. Apnea. No pulse. Asystole ACTIONS Confirm. Give 2 initial breaths with BVM (or other ventilation device). Quick-look to identify rhythm (CPR until monitor/defibrillator attached). Check in 2 leads. CPR (w/BVM/OPA). ET (Monitor pulse Ox & Capnography) IV access. Epinephrine 1mg IVP Q3-5 min (2 mg/20 ml ET if IV not available). Atropine 1mg IVP Q5 min (to max of 3.0mg). Monitor rhythm for changes. CONTACT MEDICAL CONTROL HOTRAC Regional EMS Guidelines Rev. 5.10 Page 115 PULSELESS ELECTRICAL ACTIVITY HISTORY Downtime. Bystander CPR. Implanted defibrillator SIGNS & SYMPTOMS Apnea, pulselessness. (AICD). Meds. Cardiovascular and/or other significant medical history. Substance abuse. DIFFERENTIALS Hypoxemia. Hypovolemia. Hypokalemia. Hyperkalemia. Hypothermia. Hypoglycemia. Toxicology. Tension pneumothorax. Tamponade. Thrombosis (pulmonary embolism). Thrombosis (MI). PEARLS The cardiac monitor & 02 kit must go in to the pt. on ALL calls with possible cardiac disorders (i.e. altered LOC, chest pain, palpitations, shortness of breath, etc.). If CPR is being applied upon arrival – have continued until ECG ‘quick-look’ is available. If downtime >20 min – consider DNR (refer to DNR guideline). This must be well documented. Apply 02 at highest flow to BVM as early on as possible. Flush IV line after each drug with no less than 20cc NS. At any time the rhythm changes – go to the appropriate guideline. At any time a pulse reoccurs – go to post-resuscitation guideline. CONDITION Unconsciousness. Apnea. No pulse. PEA. ACTIONS Confirm. Give 2 initial breaths with BVM (or other ventilation device). Quick-look to identify rhythm (CPR until monitor/defibrillator attached). CPR (w/BVM/OPA). ET (Monitor Pulse Ox & Capnography) IV access. Fluid challenge with 250cc-500cc NS Epinephrine 1 mg IVP Q 3-5 min (2 mg/20 ml ETP if IV not available). Atropine 1 mg IVP Q 5 min (to max of 3 mg) IF HR <60. Monitor rhythm for changes. CONTACT MEDICAL CONTROL HOTRAC Regional EMS Guidelines Rev. 5.10 Page 116 POST-RESUSCITATION (guideline for resuscitated cardiac arrest) PEARLS Half-dose Lidocaine on all pts. >70, BP <90, or with liver dysfunction (bolus & infusion). Use caution in the immediate post-resuscitation period (1st 15-min post-arrest) by avoiding medications (or electrical therapy) for SVT, bradycardia, or hypotension without first allowing these things to correct themselves – however, they may need to be corrected if prolonged – contact Medical Control when unsure. Do NOT hyperventilate resuscitated pts. (ventilate adults at 12-15 min & with normal tidal volume). DO apply high flow 02. Restraints should be considered to prevent self-extubation by the pt. CONDITION Pulse returned. Ventricular ectopy (10 or more PVC’s/min after 15 min post-arrest). If unstable or runs of V-Tach Intubated pt. (struggling with tube). ACTIONS High flow 02. Assess for return of spontaneous respirations & provide if needed (do NOT hyperventilate). Assess blood pressure. Lidocaine 0.5mg/kg IV may repeat up to 3mg/kg Hypotension. For active gag reflex, Do NOT extubate. Attempt to get pt. to tolerate tube. If needed, and BP is stable, administer Promethazine 12.5mg slow IVP to minimize gag reflex (6.25mg in elderly/small pts.) Or, if sedation is indicated, you may deliver 1.0mg Versed IVP. 250ml saline fluid challenge (if breath sounds are clear). Consider Trendelenburg’s position. CONTACT MEDICAL CONTROL Hypotension refractory to fluids (after 15 min post-arrest). HOTRAC Regional EMS Guidelines Rev. 5.10 Dopamine infusion @ 5mcg/kg/min (14-18 gtt/min). Page 117 RESPIRATORY DISTRESS MEDICAL General Considerations ASSESSMENT History of Asthma, COPD, Heart Failure, Pulmonary Edema, Pneumonia Medications, including Theophylline preparations, inhalers, digitalis Events leading to distress...allergic exposure, chest pain, elevated BP SPECIFIC ASSESSMENT Level of Consciousness Airway obstruction Cyanosis Respiratory rate and depth of ventilation Neck vein distention or not Consider trauma MANAGEMENT WITH O2 AND AIRWAY ADJUNCTS ECA/EMT INTERMEDIATE PARAMEDIC Check ABC’s Assess oxygenation; use supplemental O2 as indicated O2 per high flow mask Assist ventilation PRN Transport, sitting if necessary for comfort Check ABC’s Assess oxygenation; use supplemental O2 as indicated O2 per high flow mask Assist ventilation PRN Intubate PRN Contact Medical Control Transport, sitting if necessary for comfort Check ABC’s Assess oxygenation; use supplemental O2 as indicated O2 per high flow mask Assist ventilation PRN Intubate PRN Contact Medical Control Monitor & treat any Dysrhythmia per protocols Transport, sitting if necessary for comfort HOTRAC Regional EMS Guidelines Rev. 5.10 Page 118 RESPIRATORY DISTRESS MEDICAL Asthma & COPD SEVERE WHEEZING & DYSPNEA OR DECREASED RESPIRATORY EFFORT ECA/EMT INTERMEDIATE PARAMEDIC Check ABC’s Assess oxygenation; use supplemental O2 as indicated High flow O2 & assist ventilation PRN Monitor level of consciousness and respiratory rate *Albuterol if wheezing is severe or not moving air well. Transport, sitting if necessary for comfort *May NOT be performed by ECA Check ABC’s Assess oxygenation; use supplemental O2 as indicated High flow O2 & assist ventilation PRN Monitor level of consciousness and respiratory rate Saline lock Albuterol if wheezing is severe or not moving air well. Transport, sitting if necessary for comfort Note: If very long transport time and unable to contact Medical Control, repeat Albuterol PRN if pulse < 140 HOTRAC Regional EMS Guidelines Rev. 5.10 Check ABC’s Assess oxygenation; use supplemental O2 as indicated High flow O2 & assist ventilation PRN Monitor level of consciousness and respiratory rate Saline lock Cardiac monitor & contact Medical Control if Dysrhythmia Albuterol if wheezing is severe or not moving air well. May repeat x1 (up to 3 times) Contact Medical Control for additional medication administration Transport, sitting if necessary for comfort Page 119 RESPIRATORY DISTRESS MEDICAL Pulmonary Edema ASSESSMENT Note rales, neck vein distention, Dyspnea, frothy or blood-tinged sputum ECA/EMT Follow General Respiratory Distress Protocol Monitor BP q 5 minutes If patient not allergic or history of active ulcer disease, 4 chewable baby aspirin or equivalent even in absence of active chest pain Transport, sitting if necessary for comfort HOTRAC Regional EMS Guidelines Rev. 5.10 SEVERE DYSPNEA WITH MOIST RALES INTERMEDIATE Follow General Respiratory Distress Protocol Monitor BP q 5 minutes If patient not allergic or history of active ulcer disease, 4 chewable baby aspirin or equivalent even in absence of active chest pain Saline lock Transport, sitting if necessary for comfort PARAMEDIC Follow General Respiratory Distress Protocol Monitor BP q 5 minutes If patient not allergic or history of active ulcer disease, 4 chewable baby aspirin or equivalent even in absence of active chest pain Saline lock Cardiac monitor & manage any Dysrhythmia If BP 100 Systolic, 2 NTG 0.4 mg & repeat BP If still Dyspneic & BP ≥ 110 Systolic, repeat 2 NTG 0.4 mg x 2 PRN Contact Medical Control If transport time > 15 min. and still dyspneic, Furosemide 1 mg/Kg. May start Dopamine drip; dosage per medical control Transport, sitting if necessary for comfort Page 120 RESPIRATORY DISTRESS MEDICAL Suspected Epiglottitis ASSESSMENT Toxic appearing child/adult with sore throat and respiratory distress SPECIFIC ASSESSMENT Usually in children from 2 to 5 years old but can occur at any age Febrile, very toxic appearing children with respiratory distress and drooling Head usually held forward in "tripod” position Can also occur in adults at any age Croup in children also presents similarly, usually in child age 6 mo. to 3 yr. ECA/EMT INTERMEDIATE PARAMEDIC Follow General Respiratory Distress Protocol Use extreme caution and try to keep child quiet. May ask mother to hold child and hold O2 near child's nose & mouth Use Bag-Valve-Mask with tight seal if airway starts to close Contact Medical Control Transport Follow General Respiratory Distress Protocol Use extreme caution and try to keep child quiet. May ask mother to hold child and hold O2 near child's nose & mouth Use Bag-Valve-Mask with tight seal if airway starts to close. Do not attempt intubation Contact Medical Control No IV in children Transport Follow General Respiratory Distress Protocol Use extreme caution and try to keep child quiet. May ask mother to hold child and hold O2 near child's nose & mouth Use Bag-Valve-Mask with tight seal if airway starts to close. Do not attempt intubation Contact Medical Control No IV in children Transport HOTRAC Regional EMS Guidelines Rev. 5.10 Page 121 VENTILATOR PROTOCOL (for Auto Vent 2000/3000 Portable Ventilators) Policy: The Auto vent Portable Ventilator is to be used for facility-to-facility transports of patient requiring constant ventilator support. They may be used for scene-to-hospital transports, especially when there is a prolonged scene time, a cardiac arrest, or prolonged scene-to-hospital time. I. SET-UP a. Connect: 1. 6 ft 02 tubing (green) to source gas inlet and O2 source 2. Dual white 3 ft hose assembly to patient outlet 3. Assemble basic or PEEP parts b. Turn on 02 source (50 PSI) c. Set RATE (per Respiratory Therapist) or 10-12 if scene response d. Set TIDAL VOLUME (per Respiratory Therapist) or 10cc/kg if scene response e. Set dial to child or adult (auto vent 3000 only) f. Adjust volume and rate as needed (from pulse ox and capnography readings) and document all adjustments and their effect. g. Assure that the green visual indicator located on top of the patient valve assembly appears during each ventilation. II. PATIENT APPLICATION a. Check all alarms and settings, and run ventilator for several cycles to confirm that everything is functional. b. If the high pressure alarm sounds, check unit for kinked tube or obstruction. III. USE OF THE VENTILATOR a. Prior to making a ventilator transport, be sure that the unit has an ample supply of oxygen. Be prepared to change 02 tanks en route if needed. b. If the machine malfunctions and it cannot be easily remedied, remove it and provide ventilations via a bag-valvemask. IV. STORAGE a. After use, discard and replace all disposable parts. b. Surface clean entire unit and connections (refer to manufacturer’s manual for detailed cleaning instructions). HOTRAC Regional EMS Guidelines Rev. 5.10 Page 122 TASER REMOVAL GUIDELINE STEPS: 1. Before touching any patient who has been subdued using a Taser, insure that the police officer has disconnected the wires from the handheld unit. 2. Identify the location of the probes on the patient’s body. 3. Determine from the law enforcement officer, the patient’s condition from the time of Taser discharge, until EMS arrival. 4. Assess vital signs including ECG monitoring and pulse oximeters. 5. If patient’s age greater than 35, perform 12-lead ECG. 6. Obtain patient’s history including; tetanus, cardiac history and mind altering stimulants such as Phencyclidine (PCP) or Cocaine. 7. All of the above findings should be documented on the patient care report and transport the patient if appropriate. 8. Extracted probes are evidence and should be given to law enforcement officers. Removal of Probe(s) by EMS Provider: 1. Place one hand on the area where the probe is embedded and stabilize the skin surrounding the puncture site. 2. Place second hand firmly around the probe. 3. In one fluid motion, pull the probe straight out from the puncture site. 4. Repeat procedure for second probe. 5. Cleanse puncture sites and bandage as appropriate. 6. Suggest patient be evaluated within 48 hours by MD. 7. If no tetanus within 5 years, advise patient to obtain tetanus within 48 hours. Contraindications: When a probe is embedded in a potentially vulnerable region (i.e. face, neck, groin or female breast) do not remove. If potential for complications exist, contact on-line medical control or transport to appropriate hospital. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 123 SNAKEBITE ASSESSMENT Identify Snake if possible. Note localized swelling, erythema and circulation/ pulses Bite wound: Location, number of fang marks Signs of envenomation: Edema, vomiting, hypotension, paresthesias ECA/EMT INTERMEDIATE PARAMEDIC Remove patient from area of snake Check ABC’s Assess oxygenation; use supplemental O2 as indicated Remove any rings or jewelry because of swelling Immobilize bitten part lower than heart Do not place ice on affected part or attempt incision or suction Transport Remove patient from area of snake Check ABC’s Assess oxygenation; use supplemental O2 as indicated Remove any rings or jewelry because of swelling Immobilize bitten part lower than heart Do not place ice on affected part or attempt incision or suction Saline lock Transport Remove patient from area of snake Check ABC’s Assess oxygenation; use supplemental O2 as indicated Remove any rings or jewelry because of swelling Immobilize bitten part lower than heart Do not place ice on affected part or attempt incision or suction Saline lock Cardiac monitor if symptoms or cardiac history Transport HOTRAC Regional EMS Guidelines Rev. 5.10 Page 124 POISONING & OVERDOSE ASSESSMENT Note type of poisoning. If possible bring sample of poison, or container, to hospital If substance is identified in the field, call hospital as early as possible with information Try to determine amount, time of exposure, concentration of poison Note skin condition, pupils, salivation, odor of breath Medical history, medications, any injury associated with the poisoning? Take precautions examining any patients with possible contact poisoning. Decontamination of patient should include protective garments for rescuer and removal of the patient from contact with the poison, followed by cleansing of the body or affected body parts with water. ECA/EMT INTERMEDIATE PARAMEDIC Check ABC’s Assess oxygenation; use supplemental O2 as indicated Contact Medical Control Transport Check ABC’s Assess oxygenation; use supplemental O2 as indicated Contact Medical Control Saline lock Transport Check ABC’s Assess oxygenation; use supplemental O2 as indicated Contact Medical Control Saline lock Cardiac monitor If suspected opiate ingestion, Naloxone 2 mg IV Contact Medical Control May request Diphenhydramine 25 IV if dystonic reaction Contact Medical Control If organophosphate poisoning and has salivation, lacrimation, vomiting, then request Atropine, 1 mg IV & repeat PRN in 5 minutes. If known Tricyclic overdose contact Medical Control for 1 amp Sodium Bicarbonate slow IV Transport HOTRAC Regional EMS Guidelines Rev. 5.10 Page 125 INTOXICATION AND BEHAVIORAL EMERGENCIES ASSESSMENT SCENE SAFETY SHOULD ALWAYS BE OBSERVED. Intoxication assessment in field consists mostly of clinical evaluation. Odor of alcohol If possible with patient's behavior evaluate per Poisoning & Overdose Guideline If not able to apply monitor or start saline lock etc., due to inability of patient to cooperate then document the circumstances and proceed to transport ECA/EMT INTERMEDIATE PARAMEDIC Check ABC’s Assess oxygenation; use supplemental O2 as indicated C-Spine Precautions if indicated Psych support Restrain PRN according to restraints policy May do finger stick and perform Dextrostix If Dextrostix 50 give Instant Glucose if patient can protect airway Transport Check ABC’s Assess oxygenation; use supplemental O2 as indicated C-Spine Precautions if indicated Psych support Restrain PRN according to restraints policy Perform Dextrostix Saline lock If Dextrostix 50, start IV of Normal saline & give D50, 25 gm IV. If no IV access, Instant Glucose if patient can protect airway Transport Check ABC’s Assess oxygenation; use supplemental O2 as indicated C-Spine Precautions if indicated Psych support Restrain PRN according to restraints policy Perform Dextrostix Saline lock If Dextrostix 50, start IV of Normal saline & give D50, 25 gm IV. If no IV access, Instant Glucose if patient can protect airway If not Glucagon 1 mg IM Transport HOTRAC Regional EMS Guidelines Rev. 5.10 Page 126 HYPERTHERMIA Heat Exhaustion ASSESSMENT Does patient have fever? Is he sweating or not, was he exercising prior to onset Environmental factors: temperature, humidity Predisposing factors, age, medications, alcohol, exercise Altered level of consciousness? Hypovolemic? SPECIFIC ASSESSMENT Patient may not have a fever. Warm, sometimes diaphoretic with headache, nausea, weakness. Usually somewhat Hypovolemic. *No very high fever and *no alteration in state of consciousness ECA/EMT INTERMEDIATE PARAMEDIC Check ABC’s Assess oxygenation; use supplemental O2 as indicated Remove from warm environment & loosen clothing Sponge with cool water if available Small amounts of clear liquids PO is OK if not nauseated Transport Check ABC’s Assess oxygenation; use supplemental O2 as indicated Remove from warm environment & loosen clothing Sponge with cool water if available Small amounts of clear liquids PO is OK if not nauseated IV Normal saline 250 cc Bolus then reassess and may rebolus Transport Check ABC’s Assess oxygenation; use supplemental O2 as indicated Remove from warm environment & loosen clothing Sponge with cool water if available Small amounts of clear liquids PO is OK if not nauseated IV Normal saline 250 cc Bolus then reassess and may rebolus Cardiac monitor Transport HOTRAC Regional EMS Guidelines Rev. 5.10 Page 127 HYPERTHERMIA Heat Stroke SPECIFIC ASSESSMENT Patients with Heat Stroke will have high fever and appear quite ill. They are hot & dry and almost always have some altered level of consciousness. ECA/EMT INTERMEDIATE PARAMEDIC Check ABC’s Assess oxygenation; use supplemental O2 as indicated Remove patient from hot environment and loosen clothing Aggressively cool patient with ice packs, wet towels, if available Small amounts of clear liquids PO is OK if not nauseated Transport Check ABC’s Assess oxygenation; use supplemental O2 as indicated Remove patient from hot environment and loosen clothing Aggressively cool patient with ice packs, wet towels, if available Small amounts of clear liquids PO is OK if not nauseated IV Normal saline 250 cc bolus then re-assess and may rebolus Transport Check ABC’s Assess oxygenation; use supplemental O2 as indicated Remove patient from hot environment and loosen clothing Aggressively cool patient with ice packs, wet towels, if available Small amounts of clear liquids PO is OK if not nauseated IV Normal saline 250 cc bolus then re-assess and may rebolus Cardiac monitor If seizure activity, then Diazepam 5 mg IV Transport HOTRAC Regional EMS Guidelines Rev. 5.10 Page 128 HYPOTHERMIA SPECIFIC ASSESSMENT Air & water temperature and length of exposure are risk factors. Was patient wet or dry? Level of consciousness Vital Signs. If present, but very depressed, do not start CPR History including medications, alcohol, trauma ECA/EMT INTERMEDIATE PARAMEDIC Move patient to warm area & remove wet clothing. Wrap in blankets. Check ABC’s Assess oxygenation; use supplemental O2 as indicated High flow O2 if possible If core temperature > 90°F OK to use blankets. Warm blankets OK. If core temp 90°F, use blankets, but no external heat to be applied. Do not use airway adjuncts unless CPR. CPR PRN after 1 min. of evaluation to determine pulselessness. Pt will require CPR until re-warmed. Transport Move patient to warm area & remove wet clothing. Wrap in blankets. Check ABC’s Assess oxygenation; use supplemental O2 as indicated High flow O2 if possible If core temperature > 90°F OK to use blankets. Warm blankets OK. If core temp 90°F, use blankets, but no external heat to be applied. Do not use airway adjuncts unless CPR. CPR PRN after 1 min. of evaluation to determine pulselessness. Pt will require CPR until re-warmed. IV Normal saline, 250 cc bolus then re-assess and may rebolus. Warm the solution if possible. Transport Move patient to warm area & remove wet clothing. Wrap in blankets. Check ABC’s Assess oxygenation; use supplemental O2 as indicated High flow O2 if possible If core temperature > 90°F OK to use blankets. Warm blankets OK. If core temp 90°F, use blankets, but no external heat to be applied. Do not use airway adjuncts unless CPR. CPR PRN after 1 min. of evaluation to determine pulselessness. Pt will require CPR until re-warmed. IV Normal saline, 250 cc bolus then re-assess and may rebolus. Warm the solution if possible. Cardiac monitor. Note that if V. Fib then defibrillation not effective until re-warmed. Any cardiac drugs will have delayed effects. Transport HOTRAC Regional EMS Guidelines Rev. 5.10 Page 129 OBSTETRICS Normal Delivery & General Considerations ****note triage tags with all assessment information. ASSESSMENT Due date & previous pregnancies Medical History, allergies, bleeding disorders Previous complications such as C-sections, difficult deliveries It patient is a multiple trauma victim, then becomes a Level III unless other factors make her a higher trauma level SPECIFIC ASSESSMENT Interval between pains. Are membranes ruptured? Bleeding? Urge to Push? Face or extremities edematous or headache present or elevated BP? (Possible pre-eclampsia) Perineum inspection: Any bleeding or fluid? Crowning? If infant delivered, evaluate with APGAR score at 1 minute and 5 minutes with score of 0-2 for each category. APGAR: Color, Heart Rate, Respirations, Reflexes, Muscle Tone If multiple births, must provide which baby came first ECA/EMT INTERMEDIATE PARAMEDIC If not crowning or actively pushing transport on left side Check ABC’s Assess oxygenation; use supplemental O2 as indicated High flow O2 If crowning: sterile technique & control speed of delivery. Suction nose & mouth. Gently dry baby. Resuscitate baby PRN. Prepare for delivery of placenta. Clamp cord 8" and 10" from baby & cut cord between clamps Transport Keep mother & baby together. Place triage tag on both mother and baby & note mother’s number on baby’s tag and baby’s number on mother’s tag If not crowning or actively pushing transport on left side Check ABC’s Assess oxygenation; use supplemental O2 as indicated High flow O2 If crowning: sterile technique & control speed of delivery. Suction nose & mouth. Gently dry baby. Resuscitate baby PRN. Prepare for delivery of placenta. Clamp cord 8" and 10" from baby & cut cord between clamps Saline lock Transport Keep mother & baby together. Place triage tag on both mother and baby & note mother’s number on baby’s tag and baby’s number on mother’s tag If not crowning or actively pushing transport on left side Check ABC’s Assess oxygenation; use supplemental O2 as indicated High flow O2 If crowning: sterile technique & control speed of delivery. Suction nose & mouth. Gently dry baby. Resuscitate baby PRN. Prepare for delivery of placenta. Clamp cord 8" and 10" from baby & cut cord between clamps Saline lock Monitor, if cardiac history Transport Keep mother & baby together. Place triage tag on both mother and baby & note mother’s number on baby’s tag and baby’s number on mother’s tag HOTRAC Regional EMS Guidelines Rev. 5.10 Page 130 OBSTETRICS Prolapsed Cord ASSESSMENT Loop of cord will be protruding from vagina prior to delivery of baby, usually with fetal distress ECA/EMT INTERMEDIATE PARAMEDIC Check ABC’s Assess oxygenation; use supplemental O2 as indicated High flow O2 Put mother in Knee-Chest Position Glove & place 3 fingers into vagina and support head off cord Sterile, moist saline dressing on cord during transport Transport Check ABC’s Assess oxygenation; use supplemental O2 as indicated High flow O2 Put mother in Knee-Chest Position Glove & place 3 fingers into vagina and support head off cord Sterile, moist saline dressing on cord during transport Saline lock, but do not delay transport Transport Check ABC’s Assess oxygenation; use supplemental O2 as indicated High flow O2 Put mother in Knee-Chest Position Glove & place 3 fingers into vagina and support head off cord Sterile, moist saline dressing on cord during transport Saline lock, but do not delay transport Transport HOTRAC Regional EMS Guidelines Rev. 5.10 Page 131 OBSTETRICS Nuchal Cord ASSESSMENT Baby will deliver with loop of cord around his neck, may be cyanotic. Usually some tension on cord ECA/EMT INTERMEDIATE PARAMEDIC Check ABC’s Assess oxygenation; use supplemental O2 as indicated High flow O2 Attempt to slip cord over infant's head with gloved hand If attempt unsuccessful, clamp cord x2 and cut between clamps Keep infant's head dry & warm & suction nose & mouth if procedure lasts over 60 seconds Follow Normal Delivery Protocol Transport mother & baby together Check ABC’s Assess oxygenation; use supplemental O2 as indicated High flow O2 Attempt to slip cord over infant's head with gloved hand If attempt unsuccessful, clamp cord x2 and cut between clamps Keep infant's head dry & warm & suction nose & mouth if procedure lasts over 60 seconds Follow Normal Delivery Protocol Saline lock but do not delay transport Transport mother & baby together Check ABC’s Assess oxygenation; use supplemental O2 as indicated High flow O2 Attempt to slip cord over infant's head with gloved hand If attempt unsuccessful, clamp cord x2 and cut between clamps Keep infant's head dry & warm & suction nose & mouth if procedure lasts over 60 seconds Follow Normal Delivery Protocol Saline lock but do not delay transport Transport mother & baby together HOTRAC Regional EMS Guidelines Rev. 5.10 Page 132 OBSTETRICS Breech Presentation ASSESSMENT Buttocks will be presenting part. Usually body rotates so that face is down. No extreme force should be used to affect baby position. If Limb presentation, field delivery is not possible & should not be attempted. Rapid transport in that case. ECA/EMT INTERMEDIATE PARAMEDIC Check ABC’s Assess oxygenation; use supplemental O2 as indicated High flow O2 If buttocks presenting, prepare for delivery. If short transport time, better to transport rapidly Keep infants abdomen toward floor Use gloved fingers to feel around neck for cord and try to slip off from around the neck Slip gloved fingers along infant's nose to establish air passage Keep infant's body warm & proceed as in Normal Delivery Protocol Transport mother & baby together Check ABC’s Assess oxygenation; use supplemental O2 as indicated High flow O2 If buttocks presenting, prepare for delivery. If short transport time, better to transport rapidly Keep infants abdomen toward floor Use gloved fingers to feel around neck for cord and try to slip off from around the neck Slip gloved fingers along infant's nose to establish air passage Keep infant's body warm & proceed as in Normal Delivery Protocol Saline lock if personnel available so no delay in transport Transport mother & baby together Check ABC’s Assess oxygenation; use supplemental O2 as indicated High flow O2 If buttocks presenting, prepare for delivery. If short transport time, better to transport rapidly Keep infants abdomen toward floor Use gloved fingers to feel around neck for cord and try to slip off from around the neck Slip gloved fingers along infant's nose to establish air passage Keep infant's body warm & proceed as in Normal Delivery Protocol Saline lock if personnel available so no delay in transport Transport mother & baby together HOTRAC Regional EMS Guidelines Rev. 5.10 Page 133 PEDIATRIC NEWBORN RESUSCITATION ASSESSMENT Note if Meconium staining. Note APGAR score at 1 minute and 5 minutes. Evaluate respiration effort In route, be sure and keep baby warm and dry. Note any congenital abnormalities If color blue or dusky, provide O2 & continue to re-evaluate in route ECA/EMT INTERMEDIATE PARAMEDIC Position infant & gently suction mouth & then nose Suction trachea if Meconium stained fluid Provide tactile stimulation If spontaneous respirations, Note heart rate. If below 100 ventilate with BVM 100% O2 for 10 seconds If rate does not increase then continue ventilation and start compressions if rate < 80 If rate < 60 start CPR Transport Position infant & gently suction mouth & then nose Suction trachea if Meconium stained fluid Provide tactile stimulation If spontaneous respirations, Note heart rate. If below 100 ventilate with BVM 100% O2 for 10 seconds If rate does not increase then continue ventilation and start compressions if rate < 80 If rate < 60 start CPR Intubate if possible Attempt IV Normal saline TKO in route, no more than 2 attempts Transport Position infant & gently suction mouth & then nose Suction trachea if Meconium stained fluid Provide tactile stimulation If spontaneous respirations, Note heart rate. If below 100 ventilate with BVM 100% O2 for 10 seconds If rate does not increase then continue ventilation and start compressions if rate < 80 If rate < 60 start CPR Intubate if possible Attempt IV Normal saline TKO in route, no more than 2 attempts Epinephrine 0.1cc/kg 0f 1:10,000 or ET 0.1cc/kg of 1:1000 Transport HOTRAC Regional EMS Guidelines Rev. 5.10 Page 134 OBSTETRICS/GYNECOLOGY Vaginal Bleeding SPECIFIC ASSESSMENT Consider Trauma History of last menstrual period, number of months gestation if pregnant Try to estimate amount of blood loss If tissue present, save tissue Fever? Vital signs ECA/EMT INTERMEDIATE PARAMEDIC Check ABC’s Assess oxygenation; use supplemental O2 as indicated High flow O2 If patient is post partum, fundus massage Assess fetal status if pregnant Transport on left side if > 6 months pregnant Check ABC’s Assess oxygenation; use supplemental O2 as indicated High flow O2 If patient is post partum, fundus massage Assess fetal status if pregnant Saline lock If BP < 100 Systolic bolus with 250 cc Normal saline. Repeat BP. May repeat bolus if BP < 100 Systolic. Contact Medical Control Transport on left side if > 6 months pregnant Check ABC’s Assess oxygenation; use supplemental O2 as indicated High flow O2 If patient is post partum, fundus massage Assess fetal status if pregnant Saline lock If BP < 100 Systolic bolus with 250 cc Normal saline. Repeat BP. May repeat bolus if BP < 100 Systolic. Contact Medical Control Transport on left side if > 6 months pregnant Note: If patient not known to be pregnant, or post menopause, then may need to go to hypotension protocol or to abdominal pain protocol. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 135 TRAUMA General Procedures (Follow for Category 1 & 2 Classification) ASSESSMENT Note mechanism of injury and damage to vehicle if MVA If penetrating trauma, note type of weapon, number of wounds, and location of wounds Revised Trauma Score to be completed on all major trauma incidents All Category 1 trauma patients are to be treated as "load & go" All Category 1 & 2 trauma patients are to be transported directly to Hillcrest Baptist Medical Center. SPECIFIC ASSESSMENT Level of consciousness and Glasgow Coma Score if applicable ABC's secured and C-spine protected Secondary Survey to be completed rapidly. Do not delay transport. Note pulses, sensation and movement of all extremities ECA/EMT INTERMEDIATE PARAMEDIC Check ABC’s Assess oxygenation; use supplemental O2 as indicated Immobilize C-Spine PRN Control airway; high low O2 Follow Spinal Motion Restriction Guidelines & Transport CPR PRN Control hemorrhage Apply splints & dressings as needed. Do not delay transport in unstable or hypotensive patients Check ABC’s Assess oxygenation; use supplemental O2 as indicated Immobilize C-Spine PRN Control airway; high flow O 2 Follow Spinal Motion Restriction Guidelines & Transport CPR PRN Control hemorrhage IV Normal saline large bore cath & 2nd IV if BP < 90 sys. Bolus with 250 ml. Do not delay transport to start the IV Contact Medical Control If BP still < 90 systolic. Rebolus with 250 ml Apply splints & dressings as needed. Check ABC’s Assess oxygenation; use supplemental O2 as indicated Immobilize C-Spine PRN Control airway; high flow O 2 Follow Spinal Motion Restriction Guidelines & Transport CPR PRN Control hemorrhage IV Normal saline large bore cath & 2nd IV if BP < 90 sys. Bolus with 250 ml. Do not delay transport to start the IV Contact Medical Control If BP still < 90 systolic. Rebolus with 250 ml Monitor if cardiac history or patient has chest pain Apply splints & dressings as needed. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 136 CLASSIFICATION OF TRAUMA PATIENTS for PRE-HOSPITAL Patients in TSA-M are classified according to severity of injury in order to determine the medical resources which may be required. EMS personnel will triage and transport trauma patients in TSA-M according to the following guidelines: Category 1. Trauma Patients with the most severe injuries are classified as Category 1 patients. Patients with the following problems are included in this category and will require the medical resources available at a TSA-M Level II Trauma Facility. When EMS personnel are unable to establish on-line medical control, these patients should be transported directly to Hillcrest Baptist Medical Center (or another appropriate Level I or Level II Trauma facility) unless the patient’s condition requires resuscitation and stabilization at the nearest appropriate acute care facility. Gun Shot Wound to head, neck or torso Respiratory Compromise/obstruction GCS less than 8 O2 sat less than 85% Adult Patients with a SBP less than 90 Child less than one year with SBP less than 70 or heart rate less than 100 or more than 190 Child 1-9 years with SBP less than 70 + 2 x age in years or heart rate less than 80 or more than 150 Category 2. Trauma Patients with the serious injuries are classified as Category 2 patients. Patients with the following problems are included in this category and will require the medical resources available at a TSA-M Level II Trauma Facility. When EMS personnel are unable to establish on-line medical control, these patients should be transported directly to Hillcrest Baptist Medical Center (or another appropriate Level I or Level II Trauma facility) unless the patient’s condition requires resuscitation and stabilization at the nearest appropriate acute care facility. Penetrating injuries to head, neck, and torso (non-GSW) Suspected Amputation proximal to the wrist or ankle Suspected Two or more proximal long bone fractures (Femur, Humerus) O2 sat less than 90% Suspected Pelvic fractures Burns more than or equal to 20% BSA or more than 10% if under 6 years old Temperature less than or equal to 95◦F GCS less than 13 Adult SBP 90-100 Heart rate more than 140 Patients with traumatic paralysis Category 3. Category 3 trauma patients are those with injuries not classified as Category 1 or Category 2. When EMS personnel are unable to establish on-line medical control, these patients should be transported directly to the nearest appropriate TSA-M trauma facility for physician evaluation. Level IV HOTRAC Regional EMS Guidelines Rev. 5.10 Page 137 Trauma Facilities after stabilization should make the decision whether to transfer to the Level II Trauma Facility if the patient has any mechanism listed or any finding listed below. Mechanism of Injury Motor Vehicle Collision - With ejection - High speed more than 40 mph - Unrestrained more than 20 mph - Death in same car - Extrication more than 20 minutes - Rollover MCC/ATV/Bike/Large animal - Separation of rider - Crash speed more than 20 mph Falls (greater than 10 feet or 2 x child’s height if under 6 years old) Assault/child abuse Auto/Pedestrian Burns (partial or full thickness) Hanging/Immersion Crush injury (not hands or feet) Findings Head - Suspected skull fracture - Documented LOC less than 5 minutes Neurologic - GCS less than 14 - Focal deficit - Traumatic paresis Musculoskeletal - Suspected Open fracture (humerus, femur, tibia) - Suspected Femur fracture - Suspected Spine fracture - Suspected Pelvic fracture - Pulseless extremity Abdomen - Severe abdominal pain - Seat belt “abrasions” Burns - Inhalation injury - More than or equal to 5% or less than 20% BSA Chest - O2 sat less than 92% HOTRAC Regional EMS Guidelines Rev. 5.10 Page 138 - Suspected Multiple (more than 2) rib fractures Sub Q air Suspected Pneumothorax/Hemothorax Significant neck and/or chest “abrasions” Category 4. Category 4 trauma patients are those with injuries not classified as Category 1, 2, or 3. When EMS personnel are unable to establish on-line medical control, these patients should be transported directly to the nearest TSA-M acute care facility for physician evaluation. GCS less than 15 Falls (less than 10 feet or less than 2 x child’s height if under 6 years old) Snakebites Injured diabetic patients taking insulin Injured pregnant patients not classified as 1, 2, or 3 Toxic substance at scene in contact with the patient HOTRAC Regional EMS Guidelines Rev. 5.10 Page 139 TRAUMA Head Injury & Spinal Trauma SPECIFIC ASSESSMENT Mechanism of Injury Vital signs...consider spinal trauma in patient with hypotension but warm & flushed Any motor deficit? Level of sensory deficit if any present Note priapism if present ECA/EMT INTERMEDIATE PARAMEDIC Follow General Trauma Protocol Transport with frequent reevaluation. Be prepared for vomiting. Follow General Trauma Protocol Intubate if decreased respiratory effort or PRN to protect airway. Transport with frequent reevaluation. Be prepared for vomiting. Follow General Trauma Protocol Contact Medical Control May premedicate with Lidocaine 100mg IV prior to intubation. Intubate if decreased respiratory effort or PRN to protect airway. Transport with frequent reevaluation. Be prepared for vomiting. HOTRAC Regional EMS Guidelines Rev. 5.10 Page 140 TRAUMA Respiratory Distress with Chest Injury ASSESSMENT Mechanism of injury Note crepitus on affected side, decreased breath sounds, flair chest movement Note any tracheal deviation, venous distention ECA/EMT INTERMEDIATE PARAMEDIC Follow General Trauma Protocol If paradoxical movement Splint area and ventilate with BVM If sucking chest wound: cover with 3-sided dressing & palpate for crepitus Recheck lung sounds frequently Follow General Trauma Protocol If paradoxical movement Splint area and ventilate with BVM If sucking chest wound: cover with 3-sided dressing & palpate for crepitus Recheck lung sounds frequently Follow General Trauma Protocol If paradoxical movement Splint area and ventilate with BVM If sucking chest wound: cover with 3-sided dressing & palpate for crepitus Recheck lung sounds frequently Needle Thoracostomy if ordered by Medical Control HOTRAC Regional EMS Guidelines Rev. 5.10 Page 141 TRAUMA Abdominal Trauma SPECIFIC ASSESSMENT Note any evidence of evisceration Note rigidity, bruising, abrasions, swelling, and pulsations Note number, location, size, and depth of wounds Note pelvic stability Important if bloody emesis or hematuria. ECA/EMT INTERMEDIATE PARAMEDIC Follow General Trauma Protocol If implementing Spinal Motion Restriction, Patient may keep knees bent if comfortable If open wound or evisceration: Cover area with moist, sterile dressing Follow General Trauma Protocol If implementing Spinal Motion Restriction, Patient may keep knees bent if comfortable If open wound or evisceration: Cover area with moist, sterile dressing Follow General Trauma Protocol If implementing Spinal Motion Restriction, Patient may keep knees bent if comfortable If open wound or evisceration: Cover area with moist, sterile dressing HOTRAC Regional EMS Guidelines Rev. 5.10 Page 142 TRAUMA Amputated Parts ECA/EMT INTERMEDIATE PARAMEDIC Follow General Trauma Protocol Cover stump with moist sterile gauze & elevate Control hemorrhage If severed part can be quickly located: wrap in moist sterile gauze, place in water tight container and place container in ice (Do not freeze) If severed part cannot be quickly located, delegate search for part Follow General Trauma Protocol Cover stump with moist sterile gauze & elevate Control hemorrhage If severed part can be quickly located: wrap in moist sterile gauze, place in water tight container and place container in ice (Do not freeze) If severed part cannot be quickly located, delegate search for part Follow General Trauma Protocol Cover stump with moist sterile gauze & elevate Control hemorrhage If severed part can be quickly located: wrap in moist sterile gauze, place in water tight container and place container in ice (Do not freeze) If severed part cannot be quickly located, delegate search for part HOTRAC Regional EMS Guidelines Rev. 5.10 Page 143 TRAUMA Isolated Fractures, Dislocations, & Sprains SPECIFIC ASSESSMENT Note localized swelling, discoloration, deformity, lacerations, and exposed bones Check for loss of motion or function Note guarding, pain, instability, pulses, sensation, movement ECA/EMT INTERMEDIATE PARAMEDIC ABC's & follow Spinal Motion Restriction Guidelines Check motor, sensory, circulation Splint areas of tenderness or deformity in accordance with Musculoskeletal Motion Restriction procedure Recheck pulses, if absent try gentle traction. Do not attempt if open fracture with bone exposed. If unsuccessful, apply splint & note time Elevate extremity and apply cold packs to distal extremities Transport ABC's & follow Spinal Motion Restriction Guidelines Check motor, sensory, circulation Splint areas of tenderness or deformity in accordance with Musculoskeletal Motion Restriction procedure Recheck pulses, if absent try gentle traction. Do not attempt if open fracture with bone exposed. If unsuccessful, apply splint & note time Elevate extremity and apply cold packs to distal extremities Transport ABC's & follow Spinal Motion Restriction Guidelines Morphine up to 5 mg IV if severe pain and no respiratory depression or hypotension Check motor, sensory, circulation Splint areas of tenderness or deformity in accordance with Musculoskeletal Motion Restriction procedure Recheck pulses, if absent try gentle traction. Do not attempt if open fracture with bone exposed. If unsuccessful, apply splint & note time Elevate extremity and apply cold packs to distal extremities Contact Medical Control May request repeated Morphine if patient still in pain Transport HOTRAC Regional EMS Guidelines Rev. 5.10 Page 144 TRAUMA Burns SPECIFIC ASSESSMENT Type of burn (thermal, electrical, chemical) Explosion or toxic fumes involved? (trauma and respiratory complications) Entrance and/or exit wounds for electrical burns Estimate depth and per cent body area of burns Watch for possibility of rescuer contamination (chemical burns) ECA/EMT INTERMEDIATE PARAMEDIC Remove patient from source Decontamination PRN Follow General Trauma Protocol If burns >10% body area, cover with dry, sterile dressing Remove patient from source Decontamination PRN Follow General Trauma Protocol If respiratory burn with soot or charring of mouth/nose, consider intubation If burns >10% body area, cover with dry, sterile dressing Remove patient from source Decontamination PRN Follow General Trauma Protocol If respiratory burn with soot or charring of mouth/nose, consider intubation If burns >10% body area, cover with dry, sterile dressing Contact Medical Control Morphine up to 5 mg IV if severe pain and no respiratory depression or hypotension. May repeat with concurrence of medical control until pain is controlled HOTRAC Regional EMS Guidelines Rev. 5.10 Page 145 TRAUMA Near Drowning ASSESSMENT Important factors are water temperature, length of time submerged, water contamination. Bring sample of water if contaminated Note depth of water (Possible trauma from diving injury) Lung sounds and neurologic status important Is SCUBA diving a factor? HYPOTHERMIA IS FREQUENT ACCOMPANIMENT OF NEAR DROWNING. ALWAYS TRANSPORT: PULMONARY EDEMA CAN BE DELAYED FOR SEVERAL HOURS ECA/EMT INTERMEDIATE PARAMEDIC Protect C-Spine while removing patient from water on backboard Follow General Trauma Protocol Suction PRN. Vomiting is common Protect C-Spine while removing patient from water on backboard Follow General Trauma Protocol Suction PRN. Vomiting is common Protect C-Spine while removing patient from water on backboard Follow General Trauma Protocol Suction PRN. Vomiting is common HOTRAC Regional EMS Guidelines Rev. 5.10 Page 146 EMS Guidelines APPENDIX HOTRAC Regional EMS Guidelines Rev. 5.10 Page 147 S A M P L E ------- EMS Patient Refusal Checklist Name Age/DOB Date Nature of Call Run # ASSESSMENT OF PATIENT (Complete each item, check appropriate response) 1. Oriented to: Person, Place, Time? Yes No Age? Yes No Birthday? Yes No President? Yes No Count backwards? Yes No Recall of three items? Yes No 2. Altered level of consciousness? No Yes 3. Suspected head injury? No Yes 4. Alcohol / drug ingestion? (Exam or History) No Yes 5. Age 18 or over? Yes No MEDICAL CONTROL (Contact if patient is unable to make legal informed consent.) Contacted by: Phone Radio Time Unable to contact: (Explain) Possible Possible Spoke With Orders: Indicated treatment and/or transport may be refused by patient Use reasonable force and/or restraints to provide indicated treatment Use reasonable force and/or restraints to transport Other: PATIENT ADVISED (Complete each item, check appropriate response) Yes No Medical treatment / evaluation needed Yes No Ambulance transport needed Yes No Further harm could result without medical treatment / evaluation Yes No Transport by means other than ambulance could be hazardous in light of patient’s present illness or injury Yes No Patient provided with refusal advice sheet Yes No Patient accepted refusal advice sheet Yes No Patient informed, if appropriate, that there is a potential threat to life/limb HOTRAC Regional EMS Guidelines Rev. 5.10 Yes Yes No No Yes No Yes Yes No No Agency: Officer: Yes No Refused all EMS Services Refused transport, accepted field treatment Refused field treatment, accepted transport Released in care or custody of self Released in custody of law enforcement agency Released in care or custody of relative or friend Name: Relationship: Page 148 S A M P L E ---- Refusal of Care Information Sheet Please read and keep this form! The Emergency Medical Service has given this form to you because you have refused treatment and/or transport. Your health and safety are our primary concern. Even though you have decided not to accept our advice, please remember the following: 1. 2. 3. 4. 5. 6. The evaluation and/or treatment provided to you by EMS are not a substitute for medical evaluation and treatment by a doctor. We advise you to get medical evaluation and treatment. Your condition may not seem as bad to you as it actually is. Without treatment, your condition or problem could become worse. If you are planning to get medical treatment, a decision to refuse treatment or transport by the EMS may result in a delay that could make your condition or problem worse. Medical evaluation and/or treatment may be obtained by calling your doctor, if you have one, or by going to any hospital emergency department in this area, all of which are staffed 24 hours a day by emergency physicians. You may be seen at these departments without an appointment. If you change your mind or your condition becomes worse and you decide to accept treatment and transport by EMS, please do not hesitate to call us back. We will do our best to help you. Don't wait! When medical treatment is needed, it's usually better to get it right away. If the box at the left has been checked, it means that your problem or condition has been discussed with an emergency physician by radio or telephone and the advice given to you by EMS has been issued or approved by the emergency physician. I have received a copy of this information sheet. I assume all risks and consequences of my decision and hereby release Provider and their agents or employees from any liability arising from this decision. Patient Signature _______________________________________Date_______________________ La NEGATIVA DE HOJA de INFORMACION de CUIDADO Lea por favor y mantenga esta forma! La Emergencia el Servicio Médico le ha dado esta forma a usted porque usted ha rehusado el tratamiento y/o el transporte. Su salud y la seguridad son nuestro primario concierno. Aunque usted ha decidido no aceptar nuestro consejo, recuerda por favor lo Siguiente: 1. 2. 3. 4. 5. 6. La evaluación y/o el tratamiento proporcionados a usted por EMS no son un substituto para la evaluación y el tratamiento médicos por un doctor. Nosotros lo avisamos a obtener la evaluación y el tratamiento médicos. Su condición no puede parecer como mala a usted como es verdaderamente. Sin el tratamiento, su condición o el problema podrían llegar a ser peores. Si usted planea para obtener el tratamiento médico, una decisión de rehusar el tratamiento o el transporte por el EMS pueden tener como resultado una demora que podría hacer su condición o el problema peores. La evaluación y/o el tratamiento médicos pueden ser obtenidos llamando a su doctor, si usted tiene uno, o yendo a cualquier departamento de la emergencia del hospital en esta área, todos los cuales son proveídos 24 horas un día por médicos de emergencia. Usted puede ser visto en estos departamentos sin una cita. Si usted cambia de opinión o su condición llega a ser peor y usted decide aceptar el tratamiento y el transporte por EMS, por favor no vacilan en llamarnos apoyamos. Haremos nuestro ayudarlo mejor. ¡No espere! Cuándo tratamiento médico se necesita, generalmente mejor lo deberá obtener inmediatamente. Si la caja en la izquierda se ha verificado, significa que su problema o la condición han sido discutidos con un médico de la emergencia por radio o teléfono y por el consejo dado a usted por EMS ha sido publicado o ha sido aprobado por el médico de la emergencia. He recibido una copia de esta hoja de información. Asumo que todo se arriesga y las consecuencias de mi decisión y por la presente libera Provider y sus agentes o los empleados de cualquier responsabilidad que surge de esta decisión. La Firma paciente____________________________________La fecha: _______________________ HOTRAC Regional EMS Guidelines Rev. 5.10 Page 149 S A M P L E ---- Pre-Hospital Thrombolytic Screen Date___________________ Patient Name________________________________________ Age__________ Weight__________ Time since onset of chest pain in Hours____________________ Medications Now:_____________________________________ ___________________________________________________ ___________________________________________________ ___________________________________________________ Allergy to Medication?_________________________________ History: Recent CVA/Stroke Pregnant? Recent surgery (3 months) Recent Injury or wound? History of clotting disorder? High Blood Pressure? History of Cancer? Peptic ulcer or GI bleeding? Suspected Aortic Dissection Allergy to TPA or Streptokinase? Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes No No No No No No No No No No Additional History or Pertinent Information or Comments: ___________________________________________________ ___________________________________________________ EMT:_______________________________________________ HOTRAC Regional EMS Guidelines Rev. 5.10 Page 150 Pediatric & Neonatal Assessment ASSESSMENT 1. LOC may be difficult to evaluate. Need to know baseline from the parent 2. Airway evaluation: note obstructions, stridor, drooling, head in sniff position 3. Breathing evaluation: note retractions, nasal flaring, use of accessory muscles Begin Newborn resuscitation with airway management and ET intubation if APGAR < 8 APGAR SCORE, NEWBORN Sign 0 1 2 Heart Rate Absent <100 >100 Respirations Absent Slow/Irregular Good, Crying Muscle Tone Limp Some Flexion Active Motion Reflex Irritability No Response Grimace Color Blue or Pale Acrocyanosis Cough or Sneeze Completely Pink PEDIATRIC VITAL SIGNS Age Heart Rate Respiratory Rate Newborn 85-205 (Mean 140) 30-60 (Mean 30+) 3 mo.-2 yr. 100-190 (Mean 130) 26-34 (Mean 27) 2 yr.-10 yr. 80-140 (Mean 80) 20-30 (Mean 24) >10 yr. 60-100 (Mean 75) 15-24 (Mean 20) HOTRAC Regional EMS Guidelines Rev. 5.10 Page 151 Example of a Standard Delegation Order (SDO) (Attachment 8 of HOT Area Chempack SOG) Standard Delegation Order for Administration of CHEMPACK Pharmaceuticals PURPOSE: To provide for immediate response in treating patients with nerve agent exposures. AUTHORITY: Texas Administrative Code, Title 25 Health Services DEFINITIONS: CHEMPACK: The voluntary participation project for the forward placement of sustainable repositories of nerve agent antidotes in numerous locations throughout the United States for quick response to a nerve agent event such as a terrorist attack. CHEMPACK is a component of the federal Strategic National Stockpile Program (SNS) operated by the Centers for Disease Control and Prevention (CDC). Nerve Agents: Extremely toxic organophosphate type chemicals, including GA (tabun), GB (sarin), GD (soman), GF (cyclosarin), and VX, which attack the nervous system and interfere with chemicals that control nerves, muscles, and glands. They are odorless and invisible and can be inhaled, absorbed through the skin, or swallowed. POLICY: 1) In the event of a nerve agent release, a CHEMPACK container (s) will be deployed from strategically located positions within the Heart of Texas Area. 2) Once deployed, CHEMPACK pharmaceuticals are administered under standing delegation orders that apply to the agency administering the pharmaceuticals during the incident. Documentation of pharmaceuticals administered should also follow standard protocols set forth by the agency administering the pharmaceuticals. 3) All Providers will ensure personal safety by assuring adequate decontamination of victims and using appropriate personal protective equipment (PPE). Medical procedures within the Exclusion Zone (Hot Zone/contaminated area) will only be performed by personnel who have specific training to allow them to function in that area. FOR: Administration of CHEMPACK Pharmaceuticals EFFECTIVE DATE: Through AUTHORIZING PHYSICIAN: SIGNATURE: ,M.D. DATE:________________ (Authorizing Physician) SIGNATURE:_________________________________________DATE:________________ Name of Entity: ______________________________________________________________ Address of Entity: _____________________________________________________________ Phone Number of Entity: _______________________________________________________ HOTRAC Regional EMS Guidelines Rev. 5.10 Page 152 Antidote Administration Recommendations for CHEMPACK Medications (Attachment 9 of HOT Area Chempack SOG) Subject: Nerve Agent / Organophosphate Antidote Administration Recommendations Purpose: Provide medical guidance to physicians providing delegated authority for any local jurisdiction receiving the CHEMPACK. The treatments outlined within this document are considered the standards for administration of these medications and are based on best practice recommendations from the United States Army Medical Research Institute for Chemical Defense. Authority: This document does not constitute or represent any authorization for distribution or administration of any medication or medical procedure. It is the responsibility of the local medical authority to determine and authorize the appropriate application, dosing, and management for patients exposed to nerve agents / organophosphates. Definitions: The nerve agents – Tabun (GA), Sarin (GB), Soman (GD), GF, and VX – are considered primary agents of threat because of their high toxicity and effectiveness through multiple routes of entry. Routes of exposure include the gastrointestinal tract, eyes, respiratory tract, and skin. Nerve agents are chemically similar to organophosphate pesticides, but are intended to be much more potent. Organophosphates – insecticides/pesticides – pose equal threat through both common use (accessibility) and ease of accidental exposure through the multiple routes of exposure, as described above. The main principles of therapy for nerve agent poisoning are early treatment, assisted ventilation, bronchial suction, muscarinic cholinergic blockade (atropine), enzyme reactivation (pralidoxime chloride), anticonvulsants (diazepam), and bronchodilation (albuterol/atrovent – not included in the CHEMPACK). Medications are delivered in various forms including Auto-injectors (automatic, spring activated syringes containing a predetermined medication) for expedient intramuscular (IM) administration and multi-dose vials for less expedient administration intramuscularly (IM) or intravenously (IV). The terms, “Nerve Agent Antidote Kit”, “NAAK” and “Mark I" are used interchangeably and contain adult dosing of atropine and pralidoxime (2-PAM). The terms “pralidoxime chloride” and “2-PAM” are used interchangeably. Indications: The most effective care that patients can receive is that care given within the first few minutes following their exposure to nerve agent or organophosphate pesticide. The CHEMPACK can be used by medical personnel as additional antidote in the case of exposure to nerve agent or organophosphate pesticide. Reference: U.S. Army Medical Research Institute of Chemical Defense (2000) Medical Management of Chemical Casualties Handbook. Third Ed. Chemical Casualty Care Division: Aberdeen Proving Grounds. Procedure: HOTRAC Regional Trauma System Plan Revised May 2010 153 Page Upon recognition that nerve agent or organophosphate pesticide exposure has occurred and symptoms of exposure are present, personnel should administer antidotes using the following weight based recommended guidelines. HOTRAC Regional Trauma System Plan Revised May 2010 154 Page A. Patients >90 lbs. B. Mild Exposure for Patients >90 lbs. – Pinpoint Pupils (Dim Vision) No antidote administration Advise patient to monitor for progression of other obvious signs and symptoms C. Moderate Exposure for Patients >90 lbs. – Pinpoint Pupils (Dim of Vision), Nasal Discharge, Mild SOB, Nausea or Vomiting, or Tremors 2mg Atropine IM or IV and 600mg Pralidoxime Chloride IM or IV Atropine 2mg IM (Syringe or AtroPen auto-injector) or IV (Syringe), immediately followed by Pralidoxime Chloride 600mg IM (Syringe or ComboPen auto injector) or IV (Syringe) Pinpoint pupils (dim vision) may be persistent after life-threatening conditions have been resolved. D. Severe Exposure for Patients >90 lbs. – Severe SOB, Apneic, Unconscious, or Convulsions 6mg Atropine IM or IV, 1800mg Pralidoxime Chloride IM or IV, and 10mg Diazepam IM or IV EITHER: Atropine 6mg IM or IV (Syringe), immediately followed by Pralidoxime Chloride 1800mg IM or IV (Syringe) OR 3 NAAKs: Atropine 2mg IM by AtroPen auto-injector, immediately followed by Pralidoxime Chloride 600mg IM by ComboPen auto injector, immediately followed by; Atropine 2mg IM by AtroPen auto-injector, immediately followed by Pralidoxime Chloride 600mg IM by ComboPen auto injector, immediately followed by; Atropine 2mg IM by AtroPen auto-injector, immediately followed by Pralidoxime Chloride 600mg IM by ComboPen auto injector AND: Diazepam 2-10mg IM (Syringe or 10mg auto injector) or IV (Syringe) Repeat Atropine 2mg IM (Syringe or AtroPen auto-injector) or IV (Syringe) PRN until SOB relieved and drying of secretions. Repeat Prolidoxime Chloride is not necessary until approximately 1 hour after initial dosing. The same dosing regimen is appropriate. Re-dosing should not occur until atropinization has occurred. Repeat Diazepam 2-10mg IM (Syringe or 10mg auto-injector) or IV (Syringe) PRN until convulsions cease. Seizures in the absence of other muscarinic and/or nicotinic effects of nerve agents / organophosphates require further investigation for cause. Monitor patient for return of signs and symptoms. Always assure the safety of the medical team and the patient by consideration of routes of exposures and potential for missed agent / substance in decontamination. Pinpoint pupils (dim vision) may be persistent after life-threatening conditions have been resolved. Patients ≥40 and ≤90 lbs. E. Mild Exposure for Patients ≥40 and ≤90 lbs. – Pinpoint Pupils (Dim Vision) No antidote administration. Advise patient to monitor for progression of obvious signs & symptoms F. Moderate Exposure for Patients ≥40 and ≤90 lbs. – Pinpoint Pupils (Dim of Vision), Nasal Discharge, Mild SOB, Nausea or Vomiting, or Tremors Dose with 1mg Atropine IM or IV Atropine 1mg IM (Syringe or 1mg AtroPen auto-injector) or 1mg IV (Syringe) Pinpoint pupils (dim vision) may be persistent after life-threatening conditions have been resolved. HOTRAC Regional Trauma System Plan Revised May 2010 155 Page Patients ≥40 and ≤90 lbs. (Continued) G. Severe Exposure for Patients ≥40 and ≤90 lbs. – Severe SOB, Apneic, Unconscious, or Convulsions Dose with 3mg Atropine IM or IV and 2-10mg Diazepam IM or IV EITHER: Atropine 3mg IM or IV (Syringe) OR 3 Atropen 1mg IM Injections: Atropine 1mg IM by AtroPen auto-injector, immediately followed by Atropine 1mg IM by AtroPen auto-injector, immediately followed by Atropine 1mg IM by AtroPen auto-injector AND: Diazepam 2-10mg IM (Syringe or 10mg auto injector) or IV (Syringe) Pralidoxime Chloride is not recommended in pediatric patients. Repeat Atropine 2mg IM (Syringe or AtroPen auto-injector) or IV (Syringe) PRN until SOB relieved and drying of secretions. Repeat Diazepam 2-10mg IM (Syringe or 10mg auto-injector) or IV (Syringe) PRN until convulsions cease. Seizures in the absence of other muscarinic and/or nicotinic effects of nerve agents / organophosphates require further investigation for cause. Monitor patient for return of signs and symptoms. Always assure the safety of the medical team and the patient by consideration of routes of exposures and potential for missed agent / substance in decontamination. Pinpoint pupils (dim vision) may be persistent after life-threatening conditions have been resolved. H. Patients <40 lbs. I. Mild Exposure for Patients <40 lbs. – Pinpoint Pupils (Dim Vision) No antidote administration Advise patient to monitor for progression of other obvious signs and symptoms J. Moderate Exposure for Patients <40 lbs. – Pinpoint Pupils (Dim of Vision), Nasal Discharge, Mild SOB, Nausea or Vomiting, or Tremors Dose with 0.5mg Atropine IM or IV Atropine 2mg IM (1 AtroPen auto-injector) Pinpoint pupils (dim vision) may be persistent after other symptoms have been resolved. K. Severe Exposure for Patients <40 lbs. – Severe SOB, Apneic, Unconscious, or Convulsions Dose with 1.5mg Atropine IM or IV and 2-10mg Diazepam IM or IV EITHER: Atropine 1.5mg IM or IV (Syringe) OR 3 Atropen 0.5mg IM injections: Atropine 0.5mg IM by AtroPen auto-injector, immediately followed by Atropine 0.5mg IM by AtroPen auto-injector, immediately followed by Atropine 0.5mg IM by AtroPen auto-injector AND: Diazepam 0.5-10mg IM (Syringe or 10mg auto injector) or IV (Syringe) Pralidoxime Chloride is not recommended in pediatric patients. Auto-injectors are not recommended for patients under 15 lbs. HOTRAC Regional Trauma System Plan Revised May 2010 156 Page L. Patients <40 lbs. (Continued) Repeat Atropine 0.5mg IM (Syringe or AtroPen auto-injector) or IV (Syringe) PRN until SOB relieved and drying of secretions. Repeat Diazepam 0.5-10mg IM (Syringe or 10mg auto-injector) or IV (Syringe) PRN until convulsions cease. Seizures in the absence of other muscarinic and/or nicotinic effects of nerve agents / organophosphates require further investigation for cause. Monitor patient for return of signs and symptoms. Always assure the safety of the medical team and the patient by consideration of routes of exposures and potential for missed agent / substance in decontamination. Pinpoint pupils (dim vision) may be persistent after life-threatening conditions have been resolved. In children with cholinergic poisoning, a loading dose of pralidoxime (20-40 mg/kg IV over 30-60 min) followed by an infusion of 10-20 mg/kg/h is often recommended (Goldfrank's Toxicologic Emergencies 8th ed 2006, p. 1515). HOTRAC Regional Trauma System Plan Revised May 2010 157 Page