MALE REPRODUCTIVE SYSTEM
advertisement

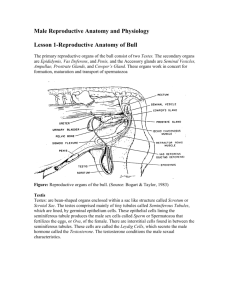
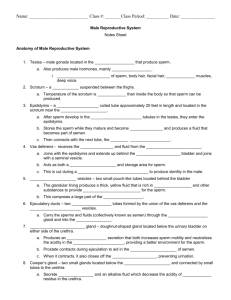
MALE REPRODUCTIVE SYSTEM I. Functional categories A. Primary sex organs: gonads–produce gametes and hormones Male: testes–produce spermatozoa and androgens (testosterone) have endocrine and exocrine functions enclosed in scrotum B. Secondary sex organs: structures essential for caring for, storage and transporting spermatozoa. 1. sperm-transporting ducts: epididymis, ductus deferens (vas deferens), ejaculatory ducts and urethra. 2. accessory glands: seminal vesicles, prostate & bulbourethral glands 3. copulatory organ: penis C. Secondary sex characteristics: not essential for reproduction, but are considered sexual attractants–ex. physique II. A. Perineum: between symphysis pubis and coccyx contains external genitalia and anal opening muscular region of the pelvic outlet 1. urogenital triangle (penis and scrotum) 2. anal triangle B. Scrotum: support, protect the testes and regulate their position and temperature 1. scrotal septum: compartmentalize (perineal raphe) 2. muscles: a) dartos–smooth muscle–subcutaneous b) cremaster–skeletal muscle (internal oblique) around spermatic cord and testes both respond to temperature–Shrinkage! “cremaster reflex:” (p. 414) C. Testes: 1. descent: (p. 699) origin: 2. inguinal canal: 3. “Cryptorchidism:” 4. Tunics: a) tunica vaginalis–outer thin serous sac from peritoneum parietal layer b) tunica albuginea–inner fibrous layer–visceral layer encapsulates each testis and forms the septa which divide the testis into lobules. 5. Lobules: a. seminiferous tubules: “functional unit of the testes” sustentacular cells =“nurse cells”=Sertoli cells blood-testis barrier (tight junctions) spermiogenesis mature sperm cell: spermatozoa head–acrosome (tip with enzymes) 23 chromosomes body-tail– Functions?! b. interstitial cells=cells of Leydig produce male hormones: testosterone is major one Androgens: anabolic steroids: stimulate muscle growth, growth of accessory sex organs, larynx, hemoglobin and bone growth 6. Ducts: rete testis–further maturation efferent ductules–to epididymis D. Spermatic Ducts: 1. Epididymis: location–superior, posterior part of testes coiled tubes–~17 feet head–body–tail 2. Ductus Deferens (aka: “vas deferens”)–from epididymis to the ejaculatory duct (18 inches) ampulla: pseudostratified ciliated columnar epithelium smooth muscle: sympathetic stimulation–peristaltic contractions 3. Ejaculatory duct: formed by ampulla of the vas deferens and the duct of the seminal vesicle. About 1 inch long, inside prostate gland. Fluid from seminal vesicle and prostate gland and sperm from vas deferens empty into the prostatic urethra. Spermatic Cord: from testes to Inguinal canal contains: ductus deferens, testicular artery and veins (pampiniform plexus), lymphatics, testicular nerve surrounded by the cremaster muscle. 4. Urethra: urinary and reproductive functions a. prostatic urethra–urine from bladder –sperm & fluid from prostate and ejaculatory ducts b. membranous urethra–through urogenital diaphragm contains: external urethral sphincter c. spongy or penile urethra: receive secretion from bulbourethral glands lined by transitional epithelium and mucous glands smooth muscle (tunica muscularis) E. Accessory Glands: 1. Seminal vesicles: location–posterior, inferior surface of urinary bladder secretes fluid with nutrients (energy) for sperm alkaline– ~60% of semen histologically–coiled mucosa–“glandular epithelium” sympathetic stimulation: 2. Prostate: location: immediately below urinary bladder surrounds prostatic urethra: BPH glandular tissue and smooth muscle fluid assist sperm motility /also alkaline ~40% of semen Clinical: BPH & prostate cancer 3. Bulbourethral glands (Cowper’s glands) location: near beginning of penile urethra mucous secretion neutralizes urine residue in urethra and lubricates the tip of the penis F. Copulatory organ: penis 1. root a. blub: attached to urogenital diaphragm–bulbospongiosus muscle b. crus: attached to pubic arch–ishiocavernosus muscle 2. body: a. (1) corpus spongiosum (erectile tissue) ventral surrounds the penile (spongy) urethra b. (2) corpora cavernosa (erectile tissue) dorsal There is fibrous C.T. between the corpora cavernosa–septum penis. c. suspensory ligament:–to symphysis pubis 3. glans penis–expanded corpus spongiousm urethral orifice corona glandis frenulum foreskin=prepuce Circumcision: FEMALE REPRODUCTION I. Functions: (p. 707) A. B. C. D. E. F. produce ova secrete sex hormones receive spermatozoa during coitus provide sites for fertilization, implantation and gestation parturition nourishment (breast) II. Functional categories: A. Primary sex organs: “gonads” Ovaries: produce gametes (ova) and sex hormones B. Secondary sex organs: essential for 1. fertilization 2. implantation 3. development 4. parturition include: external genitalia, vagina, uterine tubes, uterus, mammary glands C. Secondary sex characteristics: not essential for reproduction III. Compare to Male Reproduction: A. Similarities 1. Homologous–develop from same embryonic structures p. 725 a. testes=ovaries p. 698 b. glans penis=clitoris c. scrotum=labia majora d. spongy urethra= labia minora e. membranous urethra=vaginal vestibule f. bulbourethral glands=vestibular glands 2. Gonads produce gametes and sex hormones 3. Latent development of reproductive organs (puberty) B. Differences 1. gamete production a. male: b. female: ova –formed during fetal life not mature–stopped at prophase I/meiosis I puberty–1/month menopause Clinical: IV. Ovaries A. Attachments: 1. broad ligament–supports uterine tubes and uterus (parietal peritoneum) 2. mesovarian– 3. ovarian ligament–anchored to uterus 4. round ligament–continuation of ovarian lig. through inguinal canal to labia minora 5. suspensory ligament–attached to pelvic wall B. Anatomy 1. hilum 2. layers (4) a. superficial epithelial layer b. tunica albuginea (collagenous C.T.) c. cortex d. medulla Stroma– 3. blood supply– C. Ovarian Cycle: Newborn female has ~2 million oocytes stopped at prophase I of meiosis I. At puberty– ~400,000 ~ 400 ovulations Fig. 21.9 p. 714 Corpus luteum Corpus albicans V. Secondary sex organs A. Uterine tubes (aka fallopian tubes, oviducts, salpinx) 1. Gross structures: fimbriae infundibulum ampulla Clinical: ectopic pregnancy P.I.D. 2. Histology mucosa: muscularis serous layer B. Uterus 1. Functions: 2. Structure 1. fundus 2. body 3. cervix: a. external os (uterine ostium) b. internal os (isthmus of uterus) c. cervical canal 4. Uterine wall a. perimetrium vesicouterine pouch rectouterine pouch b. myometrium c. endometrium stratum basale stratum functionale: C. Vagina: tubular, fibromuscular orgn 1. Functions: 2. Location: 3. Structures: vaginal orifice hymen fornix 4. Histology a. mucosa: b. muscularis c. fibrous layer D. External genitalia (Vulva) 1. mons pubis 2. labia majora pudendal cleft perineum (contain sebaceous and sweat glands) Clinical: episotomy 3. labia minora prepuce 4. clitoris–glands clitoris, (2) corpora cavernosa 5. vaginal vestibule 6. vestibular glands (Bartholin’s glands) E. Breast