Laboratory Exercise 19: Reproductive Anatomy

Laboratory Exercise 19: Reproductive Anatomy
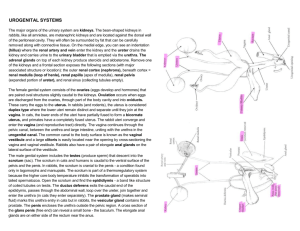
The primary role of the reproductive system is the perpetuation of the species. Male and female reproductive anatomy makes possible the union of ovum and sperm so that the new organism will have precisely ½ its genetic constitution from each parent.
The female, in addition, provides specialized structures to house and nurture the developing new individual and provide nutrients and antibodies during early postnatal life.
A secondary role of the reproductive system is to initiate and maintain the secondary sexual characteristics so as to distinguish males from females.
A.
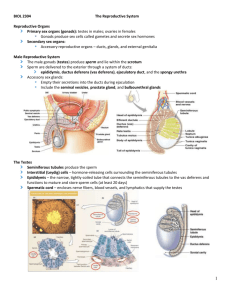
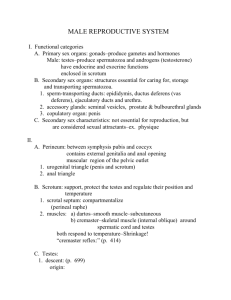
Gross Anatomy of the Male Reproductive System
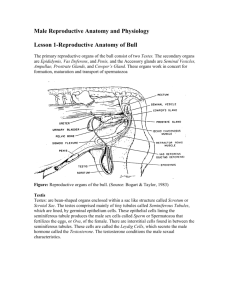
Testes
The testes are paired oval organs suspended in the saclike scrotum. The testes are connected to the abdominopelvic cavity by the spermatic cord. The spermatic cord contains blood vessels, nerves and the vas deferens (sperm duct).
The testes are divided into lobules by connective tissue septa, tunica albuginea. The tunica albuginea also surrounds each testis. Each lobule contains seminiferous tubules, where the sperms are produced.
Epididymis
The epididymis is a coiled tubule along the posterior side of each testis. It is here that nonmotile sperm reach full maturity in the fluid secreted by the epithelial cells of this organ. They are stored until peristaltic waves (ejaculation); created by smooth muscle, force them toward the vas deferens.
Vas (Ductus) Deferens (vas means vessel or duct)
The vas deferens is a continuation of the duct of the epididymis. It extends through the inguinal canal as part of the spermatic cord. After entering the abdominal cavity, each vas deferens terminates behind the urinary bladder. Here they merge with the ducts of the seminal vesicles to form the ejaculatory ducts. Peristaltic smooth muscle activity in the walls of the vas deferens and ejaculatory ducts discharge sperms under pressure.
1
Seminal Vesicles
The seminal vesicles are a pair of baglike structures on the posterior bladder wall. The glands secrete a yellow viscous, alkaline secretion from the mucous membrane lining.
The seminal fluid is high in fructose and is the largest component of the total semen volume (about 60%).
Prostate Gland
The prostate gland is a chestnut-shaped organ lying just inferior to the bladder. The prostate secretes a milky, slightly acidic fluid (prostatic fluid) which is about 20% of the semen volume. The prostate secretes the prostatic fluid into the prostatic urethra, the first part of the male urethra. The ejaculatory duct joins the prostatic urethra at this point.
Between the prostate and the penis is a short section of the male urethra, the membranous urethra.
Bulbourethral (Cowper’s) Glands
The bulbourethral glands are paired pea-sized structures at the base of the penis. They secrete a mucous secretion into the urethra.
Penis
The penis contains 3 columns of erectile tissue. The highly vascular bodies are the paired corpora cavernosa lying to either side of the midline and the corpus spongiosum lying in the ventral midline of the penis. The corpus spongiosum contains the penile urethra. The spongy nature of the erectile tissues on engorgement of blood makes erection of the penis possible.
The glans penis is covered by the prepuce (foreskin).
Semen
The semen consists of sperms and the 3 secretions from the male accessory sexual glands.
Seminal vesicles – a viscous, alkaline fluid, high in fructose – seminal fluid
Prostate – a milky acidic fluid – prostatic fluid
Bulbourethral glands – mucus
2
B. Histology of the Male Reproductive System
Testis
Each lobule of the testis contains seminiferous tubules where the sperm are produced.
The seminiferous tubules fuse to form straight tubules, which converge into a netlike arrangement of tubules, rete testis.
The rete testis connects to the epididymis by the efferent ductules. The epididymis is continuous with the vas deferens.
Seminiferous Tubules
The germinal epithelium lines the outer most layer of the seminiferous tubules. Sperm production takes place from here toward the center of the lumen. Sustentacular (Sertoli) cells within the seminiferous tubules support and nourish the developing sperm.
Interstitial cells, cells between the tubules secrete testosterone.
Spermatogenesis
Spermatogonia
mitosis
I
○
spermatocyte
I
○
meiosis
II
○
spermatocyte
I I
Spermatid
○
meiosis
Spermatozoa
(46)
(46) (46)
(23) (23)
(23) (23) (23) (23)
Penis
(23) (23) (23) (23)
Corpus spongiosum surrounds the urethra and on the dorsal surface is the corpora cavernosa. The penile urethra is lined with mucous membrane of stratified epithelium.
Sperm – consists of a head, midpiece and flagellum.
3
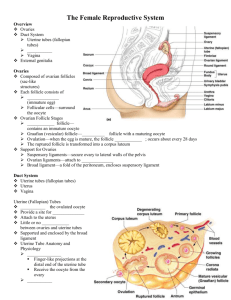
C. Gross Anatomy of the Female Reproductive System
Vulva - Female external genitalia
Mons pubis – is a hair-covered cushion due subcutaneous fat over the pubis symphysis.
Labia majora – two longitudinal folds of adipose tissue covered by hairy skin, extends inferiorly from the mons pubis. They are homologous to the scrotum.
Labia minora – a pair of hairless skin folds medial to the labia majora.
Clitoris – a cylindrical mass of erectile tissue, located at the anterior junction of the labia minora. It is homologous to the penis.
Vestibule – the space bordered by the labia minora.
Urethra – opens into the vestibule below and just posterior to the clitoris.
Vestibular (Bartholin’s) glands – mucous glands, provides mucus for lubrication during coitus.
Ovaries
The ovaries are paired organs located in the upper pelvic cavity, one on either side of the uterus. The ovaries are almond-shaped.
The ovaries are held in place by peritoneal folds.
The ovarian ligaments attach the ovaries to the uterus.
The ovaries are also supported by the mesovarium, a double fold of peritoneum that attaches to the broad ligament of the uterus.
Oviducts (Uterine or Fallopian tubes)
The oviducts are extensions of the uterus. The anterior end surrounds each ovary. To increase the probability of an ovum entering the uterus, the anterior ends of the oviducts are modified into fringes, the fimbriae. The inner surface of the each fimbriae is lined with simple ciliated columnar epithelium.
Uterus (Womb)
The uterus is a pear-shaped muscular organ located between the bladder and the rectum.
The uterus is subdivided into a fundus, the dome-shaped region above the oviducts; the body in the center and the cervix (neck), which opens into the vagina.
The uterus has 3 layered walls:
visceral peritoneum or perimetrium, the outer most layer;
myometrium an intermediate smooth muscle layer;
endometrium is a mucous membrane which lines the uterine cavity.
The uterus is attached to the wall of the pelvic cavity by the broad and uterosacral ligaments.
4
Vagina
The vagina is a canal inferior to the uterus and ends at vaginal opening into the vestibule.
The vaginal wall has inner folded mucous membrane and a smooth muscle layer outside of the mucous membrane. At the proximal end, the vagina extends past the level of the cervix to form the fornices.
D. Histology of the Female Reproductive System
Ovary
Follicles are spherical sacs of cuboidal epithelial cells surrounding the oocyte (ovum or egg cell).
Primary (I
○
) follicle – is a single layer of cells surrounding a I
○
oocyte in the center of the follicle.
Secondary (II
○
) or Growing follicle – The follicle has two or more cell layers surrounding the oocyte.
Mature (Graafian) follicle – A follicle with a central fluid-filled cavity, the antrum. The oocyte is off-center and attached to the side of the follicle by several layers of follicle cells, the corona radiata.
Only one mature follicle is formed from the 18-20 secondary follicles that develop in each menstrual cycle.
Corpus luteum – A glandular structure derived from the ovulated mature follicle.
Estrogens are mainly secreted by the cells of the follicles and progesterone by the cells of the corpus luteum.
E. Histological Changes in the Uterus During the Menstrual Cycle
These changes are under the control of the estrogens and progesterone.
1 st
week Menstrual phase (3-5 days)
The menstrual cycle begins with the onset of the menstrual flow with sloughing of the endometrium.
2 nd week Proliferative phase (6-14 days)
Under the rising estrogen level the endometrium is resurfaced with epithelial cells and the endometrium grows in thickness.
Ovulation occurs about the 14 th
day.
5
3 rd
week Secretory phase (14-21 days)
Under the influence of progesterone from the corpus luteum endometrial growth continues, endometrial glands secrete a nutritive substance to nourish the embryo.
At this time (3 rd
week), the endometrium is ready for embryo implantation.
4 th week (22-28 days)
The concentration of the estrogen and progesterone drops late in the 4 th
week if no implantation occurs. The uterine arterioles constrict, the endometrium is sloughed off and a new menstrual cycle begins.
Oogenesis
Oogonium (46)
mitosis
I
○
oocyte (46) (46)
I
○
meiosis
II
○
oocyte (23) (23) I
○
polar body
II
○
meiosis mature ovum (23) (23) (23) (23) II
○
polar bodies
F. Mammary Glands
The mammary glands are for the production of nutritive fluid, milk, for the newborn.
The mammary glands are located anterior to the pectoral muscles and extend from the lateral margin of the sternum to the anterior border of the axilla. Each breast has 15-20 lobes radially arranged around the nipple. In the lobes are alveolar glands surrounded and supported by adipose and dense connective tissue. The secretion (milk) is conveyed by lactiferous ducts whose openings are on the anterior surface of the nipple. The areola is a circular band of heavily pigmented skin surrounding the nipple. The areola contains sebaceous glands to lubricate the nipple.
6