Chest
advertisement

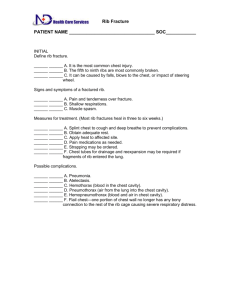
Clinical medicine – Chest 1 CHEST Anatomy N.B.: to find a certain rib: Find angle of Lewis 2nd rib. Find last rib from the back 12th rib. Find apex of scapula 7th rib. N.B.: the rib is followed by its space downwards. N.B.: Vertical lines: Midline (ML). Parasternal line (PSL). Midclavicular line (MCL). Anterior axillary line (AAL): passes through anterior axillary fold. Midaxillary line (MAL) خط خياطة القميص Posterior axillary line (PAL): passes through posterior axillary fold. Scapular line (SL): passes through apex of scapula. Paravertebral line (PVL): midway between ML and SL. Surface anatomy of right lung: Match between the following points: 4 cms above midclavicular point sternoclavicular junction angle of Lewis midline at 6th rib PSL at 6th rib MCL at 6th rib AAL at 7th rib MAL at 8th rib PAL at 9th rib SL at 10th rib PVL at 10th back to 1st point again. Surface anatomy of left lung: As right lung but in ML till 4th rib. Surface anatomy of pleura: As lungs, but add 2 ribs to the points of lower border. NB: right lung 3 lobes and 2 fissures. Left lung 2 lobes and 1 fissure. Oblique fissure: o Starts from T2 o Move parallel to medial border of scapula (while patient rising his arms up) till MAL at 5th rib. o Move forwards and medially till MCL at 6th rib. NB: o T2: below T1 below C 7 to get its process tell the patient to flex his neck; it will be the most prominent. o When the examiner asks you to examine lower lobe examine back. o Lateral view of right lung is the best to see the 3 lobes. Transverse Fissure: right lung only o From right MAL at 5th rib. o To ML at 4th rib NB: Upper and middle lobes are examined from front. Clinical medicine – Chest 2 Kronigs Isthmus: o Apex apex of lung o Base 4 pints: 1. Sterno-clavicular junction. 2. Spine of C 7. 3. Junction between lateral 1/3 and medial 2/3 of clavicle. 4. Junction between lateral 2/3 and medial 1/3 of spine of scapula. Traub’s Area: of left lung (5, 8, 9, 11) o 5th space MCL o 8th rib PSL o 9th rib MAL o 11th rib MAL Upper border by lower border of left lung Lower border by costal margin Right border by lower border of left lobe of liver Left border by anterior border of spleen NB: Trachial bifurcation: From front: angle of Lewis From back: spine of T4 NB: Upper lobe: Middle lobe: Lower lobe: Right lung Apical Anterior Posterior Medial Lateral Apical basal Anterior basal Posterior basal Lateral basal Left lung Apical Anterior Posterior Superior lingular Inferior lingular No middle lobe Apical basal Anterior basal Posterior basal Lateral basal Mediastinum: o Upper: presented by trachea, affected by lesions to upper ½ of lung. o Lower: presented by cardiac apex, affected by lesions to lower ½ of lung. Histology o Trachea main bronchus lobar bronchus bronchioles respiratory bronchioles alveoli. o Elsatin around alveoli is responsible for recoil tendency of lungs. o Pleura: Visceral layer. Parietal layer: lining chest wall, mediastinum and diaphragm. In between, there is monomolecular layer of serous fluid. The 2 layers can Clinical medicine – Chest 3 slide over each other but cannot be separated. In inspiration, diaphragm descends pulling parietal pleura pulling visceral pleura pulling lungs. Monomolecular layer is responsible for sliding and adhesion between the 2 pleural layers. For you: Capacity of thoracic cage is 5 liters while capacity of lungs is 1 liter. In spite of that, there are impressions for ribs on lung surface. This is explained as follow: At birth capacities are equal. During life, hard tissue grows faster than soft tissue. Monomolecular layer of pleura pulls thoracic cage inwards and lungs out wards making both of them stretched and making capacity of both 2.5 liters. After death, when we dissect they have their real capacities. Physiology Respiration is controlled by: 1) Chemical control: a) Inspiration ↑ O2 -- R.C. Expiration. b) Expiration ↑ CO2 ++ R.C. Inspiration. R.C. is inhibited by: ↑ O2, ↓ CO2, severe hypoxia. R.C is stimulated by: ↑ CO2, H2, hypoxia 2) Neural control: (Herring-Brever Reflex) R.C. discharges continuous impulses to diaphragm and intercostals muscles active inspiration + inflation of lungs inflation of alveoli stimulation of stretch receptors on alveoli reflex inhibition of R.C relaxation of diaphragm and intercostals muscles passive expiration. Inspiratory Expiratory Active Need muscle contraction Homogenous air flow Bronchial Diseases: o Bronchitis o B.A. o Bronchiectasis Pulmonary diseases: o Consolidation o Emphysema o Cavitations Passive Depends on recoil tendency 80% of air in 1st 1/3 time 20% of air in last 2/3 time Pathology o Bronchogenic carcinoma+bronchial edema o Bronchopneumonia o Lung fibrosis o Lung collapse Clinical medicine – Chest 4 Pleural diseases: o Pleurisy o Pleural effusion o pneumothorax Bronchitis: Inflammation of bronchial mucosa: edema+ hypersecretion generalized narrowing in proximal bronchi. It is chronic if occurs for 3 months in 2 successive years. Chronic bronchitis is usually associated with emphysema together called COPD (chronic obstructive pulmonary disease) or COLD (chronic obstructive lung disease) or COAD (chronic obstructive airway disease). May be associated with B.A or bronchiectasis. N.B: - Cilia spill mucous and distribute it. Ciliary dysfunction mucus accumulation COPD, and predisposes to infection destruction of bronchial wall become thin: o Dilatation (bilateral and basal [anaerobic infection]) o Surrounded by consolidation, fibrosis and collapse. o Filled with pus ( suppurative lung syndrome) and blood ( bronchiectasis sicca hemorrhagica) Bronchial Asthma: On 1st exposure to antigen formation of IgE without Ag-Ab reaction. On 2nd exposure Ag-Ab component fixation degradation of mast cells liberation of chemical mediators distal bronchi: bronchospasm, edema in mucosa and hypersecretion generalized narrowing of peripheral airways. N.B: Generalized narrowing in B.A. is more severe than in bronchitis due to broncho-spasm and distal bronchi have been already narrower. Course: o During attack: severe dyspnea, wheezy chest o In between attacks: complete free. Chronic bronchitis B.A. N.B: Sometimes B.A. comes on top of chronic bronchitis Asthmatic Bronchitis. Bronchogenic carcinoma and bronchial edema: Produce localized narrowing of airway. Bronchogenic carcinoma in apex of lung called Superior Sulcus Syndrome may affect: o Trachea o Pharynx o Chest wall o Sympathetic chain pancoast tumor. Clinical medicine – Chest Bronchopneumonia: Terminal bronchitis +patchy pneumonitis. Consolidation: Alveoli are filled with fluid, cellular exudates and fibrin. Causes: o Pneumonia (broncho-, lobar-) o Bronchiectasis o Around lung abscess. Emphysema: Compensatory Localized due to partial obstruction As part of COPD Mechanism: Inhaled micro-organisms contain lipase to digest fat, amylase to digest CHO, protease (α1 trypsin) to digest proteins, but α1 trypsin of micro-organism is inhibited by α1 anti-trypsin. Smoking decreased synthesis of α1 antitrypsin, and accumulation of monocytes containing α1 trypsin leading to loss of recoil tendency hyperinflation (emphysema). NB: smokers suffer from emphysema and chronic bronchitis. COPD: Type A: o Emphysema > chronic bronchitis. o Pink puffer المريض أحمر وينافخ o Inflation rupture of interalveolar septa decreased surface of gas exchange Decreased O2, increased CO2 stimulation of R.C. wash CO2, increased O2 pinkish. Tachycardia puffer. Type B: o Bronchiectasis > emphysema. o Blue bloater المريض منفوخ وأزرق o Breathing is difficult due to bronchitis cyanosis blue. o Acidosis due to increased H2CO3 increased H+ acidic urine + increased Na+ reabsorption together with its iso-osmotic water bloater. Cavitations: Filled: o Cyst o Abscess: Pyogenic T.B. Amebic Empty: old abscess. Lung fibrosis: narrowing. Lung collapse: Compressive: o Pleural effusion o Pneumothorax 5 Clinical medicine – Chest Obstructive: o With obstructive main bronchus: Tumor F.B. Fibrosis o With patent main bronchus: Hypersection. Pleurisy: edema and roughness of parietal and visceral pleura. Pleural effusion: accumulation of fluid in pleural sac: - Serous fluid hydrothorax - Blood hemothorax - Lymph chylothorax - Pus pyothorax - Fibrosis of pleura fibrothorax. Pyothorax + broncho-pleural fistula coughing pus suppurative lung syndrome. NB: Suppurative lung disease: Lung abscess Bronchiectasis Pyothorax + broncho-pleural fistula. Pneumothorax: A. Closed: forced cough rupture of alveoli into cavity. If emphysematous rupture of emphysematous bullae more serious condition. B. Open: Trauma: Stab wound Iatrogenic by needle in drainage of pleural pleural effusion. Bronchopleural fistula. In this case there is direct connection with atmosphere and so air inside pleura ↔ with inspiration and expiration and not accumulated. C. Tension pneumothorax: Cause: stab wound at angle, where the 2 holes not opposing each other. In inspiration: air enters inside pleural cavity. In expiration: air is trapped as 2 holes not opposing each other +ve pressure. NB: Closed regressive course: air is absorbed. Open stationary course: air ↔ Tension progressive course: treatment by making open pneumothorax. D. Hydropneumothorax. 6 Clinical medicine – Chest 7 Local Examination 1) Inspection: a) Skin: i) Dilated veins: (1) SVO, commonest, due to tumor, thrombus. (2) IVO. ii) Scar: right and left thoracotomy: in lobectomy or pleurectomy. b) Chest Wall: i) Shape: NB: For inspecting shape, look from foot side while patient lying on flat bed and watch carefully right and left antero-posterior length. (1) Symmetrical: (a) Elliptical: antero-posterior: Transverse =5:7 (normal shape). (b) Barrel shaped= permanent inspiratory position: Antero-posterior≥Transverse ≈ 1:1 Wide subcostal angle. Horizontal ribs. Wide intercostal spaces. Cause: hyperinflated chest (clinical term), e.g.: Emphyema which is pathological term. (c) Pigeon chest=Pecten Cranium: Causes: Hard tissue: Rickets, osteomalacia. Soft tissue: severe precordial bulge (RVE), hyperinflation as COPD since childhood. Rickets: delayed bone growth and inability for ossification soft tissue grows and bulges at cartilaginous parts. NB: to say: this is a ricketic chest, must be there one of two signs: Harrison sulcus + rosary beads. - - Harrison Sulcus: In healed rickets Diaphragm originates from lower ribs. In inspiration, diaphragm pulls cartilaginous parts inwards forming a sulcus at costal margin, even in healed rickets. Rosary beads: Normally costal cartilage proliferates from adjacent to bone then ossifies. Here, growth of cartilage without ossification masses in vertical lines. When patient recovers atrophy of them. Clinical medicine – Chest 8 (d) Pectus Excavatum=Funnel shaped: Causes: - Congenital 95% - Acquired 5%: in Shoemakers as pressure atrophy on chest indentation of lower 1/3 of sternum. If severe: Disturbs anatomy of: Heart H.F. Lung R.F. Press on the R.V. picture of constrictive pericarditis. (e) Flat (alar) chest: For examination: only mentioned with pulmonary T.B. (f) Kyphosis: if severe, it disturbs anatomy of heartH.F., Lung R.F. (2) Asymmetrical Chest: 1. Unilateral bulge Pleural effusion Pneumothorax Fluid, air disturb mononuclear layer of pleural cavity outward expansion of thoracic cage. NB: Compressive collapse bulge Obstructive collapse retraction NB: Both bulge and retraction cause limitation of movement. 2. Unilateral retraction Lung fibrosis Lung collapse 3. Scoliosis Retractile tissue pulls visceral + parietal pleura which pull thoracic cage Q. Is this side bulged or the other is retracted? A. If limitation from the bigger side, it's a bulge and vice versa. ii) Movement: (1) Type: In males, diaphragm is dominant abdominothoracic breathing. In females, intercostals muscles are dominant thoracoabdominal breathing. For you: In pregnancy, there is limitation of diaphragmatic movement ()الحمد هلل o Thoracoabdominal breathing in males: - Tense ascites - Peritonitis - Diaphragmatic paralysis o Abdominothoracic breathing in females: - Intercostal muscle paralysis - Marked pleural effusion Clinical medicine – Chest 9 - Pleurisy, pneumothorax - Severe COPD (2) Rate: o H.R. is involuntary while R.R. is both voluntary and involuntary. o During sleep, respiration is controlled by chemical and neuronal control. o Voluntary control of respiration indicates mood, so to examine rate, you have to draw patient's attention away from breathing, not to be under voluntary control, so pretend that you are measuring pulse while you are LOOKING to patient's chest. o R.R.: - 14-20 normal - >20 Tachypnea - <14 bradypnea Bradypnea Pontine hemorrhage Increased intracranial pressure Barbiturate toxicity Morphine Severe hypoxia Tachypnea as CO2 cannot cross BBB CO2 + H2O H2CO3 HCO3-+H+ Acidosis and stimulation of R.C. H+ ↓R.C. ↑R.C. Acidosis: - Metabolic hyperventilation (rapid+deep) In: Diabetic ketoacidosis Uremia Excessive acid intake (salycylate poisoning) - Respiratory: in respiratory failure tachypnea (rapid + shallow): > 40 decompensated R.F. <40 compensated R.F. (3) Inspiratory retraction: - Caused by: o Diaphragm o –ve intrathoracic pressure Both pull lower inercostals. If exaggerated it's called Litting's Sign. - Exaggerated in R.F. as COPD. - Lost in: o Diaphragmatic paralysis o Pleural effusion+pneumothorax o obesity (4) Expansion: o Type test: - Using meter tape around patient's chest at level of nipple or below breast in female (4th rib in both sexes). - Let him take deep inspiration and measure inspiration and expiration difference: 3-5 cm normal, <3 cm limited movement. Clinical medicine – Chest c) Pulsations: - Examine pulsation of heart (see inspection in cardiology). Invisible apex: emphysema/pleural effusion/pleural thickening. Extracardiac causes of apex displacement:(lesion affecting lower 1/2 of lung) Ipsilateral pulling coolapse, fibrosis. Contralateral pushing tumor, pneumothorax, pleural effusion. - Signs of RVE: Apex is shifted outwards Systolic retraction Diffuse apex LPS pulsation Epigastric pulsation - Significance of RVE diagnoses Cor-pulmonale (=RVE with or without failure due to lung disease) - The most important pulse to examine is Epigastric because if patient is emphysematous it will be the only seen pulse. N.B.: Normal HR is 60 Normal RR is 15 So Normal C/P ratio is 4:1 If heart problem tachycardia >4:1 If lung problem tachypnea <4:1 Exercise, Stress, thyrotoxicosis affect both unchanged ratio. 2) Palpation:(TPE)طبي a) Trachea: Normally cenral Causes of shifted ttrachea: lesion affecting upper 1/2 of lung: o Ipsilateral pulling coolapse, fibrosis. o Contralateral pushing tumor, pneumothorax, pleural effusion. How to examine? Left hand on the patient head to fix it making him looking forwards. Index of right hand with the nail laterally in suprasternal notch, then move to feel distance between trachea and sternomastoid muscle inboth sides: o Equal central. o Wider shifted to the other side. b) Tenderness: Palpate by pressure, looking to patient face noticing facial expressions. التسأله Causes of tenderness: from in to out: o Pleurisy: especially lower axillary+beneath breast. o Bone: Traumatic: fracture rib Inflammation: osteomylitis=Teid's Syndrome. Neoplastic: leukemia, 1ry, 2ry bone tumor. o Muscle: myositis. o Veins of breast: thrombophlebitis (Monder's disease) 10 Clinical medicine – Chest o Skin: Herpes Zoster. N.B.: In herpes zoster, in the first 24 hours no signs, only severe pain, so patient go to internist doctor not to dermatologist. N.B.: In ischemic heart diseases (Angina, myocardial infarction) there is pain without tenderness. c) TVF=tactile Vocal Fremitus: o Rules: - Comparative - By the same hand - Tips of fingers directed laterally - Sites: Supramamary, mammary, inframammary Upper, middle, lower axillary. Supra-, inrascapular on both sides, interscapular. - Each time tall patient to say أربعة أربعة o ↑↑ TVF: - Consolidation: o Pneumonia o Bronchiectasis o Around lung abscess - Lung cavity: large, superficial, empty, connected to a bronchus. - Obstructive collapse with patent main bronchus. o ↓↓ TVF: obstruction: F.B. Tumor Fibrosis Barrier: Pleural effusion Pleural thickening Pneumothorax Emphysema Obesity d) Palpable Rhonchi: o Rules: as TVF but ask patient to take deep breath. o Causes: o Bronchitis o B.A. o Fibrosis o F.B. o Tumor o Secretions (air way obstruction). e) Pulsation: see inspection + cardiology. 11 Clinical medicine – Chest 12 f) Expansion: i) Apical يامنيّل ii) Basal: (1) Anterior (infrasternal). (2) Posterior (interscapular). Method: o Take skin fold medially. o Ask patient to breath. o Notice widening. 3) Percussion: o Rules: Comparative From up downwards Horizontal pleximeter in intercostal spaces, nut horizontal or vertical in paravertebral. Light percussion except the back heavy. o Sites: Lungs: Apex: o Vertical pleximeter from behind patient. o Normally resonant. o Causes of dullness: - apical fibrosis - apical collapse - apical tumor (Pancoast tumor) - apical abscess (T.B.) - apical consolidation (Freidlander's) - apical pleural effusion (massive or encysted by adhesion) - pleural thickening Clavicle: direct percussion as clavicle acts as pleximeter, infraclavicular. Main mass of lung: o Heart: Tidal percussion Right border Bare area. Traube's areaبالطلب o 4) Auscultation