overview
advertisement

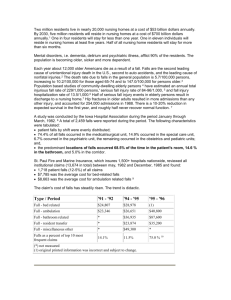
WALKING IMPROVEMENT Admission to a nursing home often coincides with older adults losing their independence with mobility and becoming more dependent on assistive devices and/or wheelchairs. As many as half of the nursing home residents who are wheelchair dependent have a history of falls and up to 25% of residents who could walk were issued a wheelchair as a result of a fall (Pawlson et al., 1986). It is also estimated that almost two-thirds of nursing home residents require assistance with transfers and walking (Resnick, 1998). Immobility can be a serious problem faced by nursing homes as it can cause limitations in activities of daily living, “pressure ulcers, pneumonia, urinary stasis, constipation and fatigue” (Norman & Gibbs, 1991). Causes of Decreased Ambulation Healthy younger adults typically perform ambulation at an energy efficient level while older adults who are generally weaker and have decreased endurance have increased energy expenditure during mobility tasks. Prosthetics, orthopedic impairments, weakened lower extremities, and assistive devices can also add to the metabolic output in addition to the effect of aging resulting in further difficulty with ambulation (McGibbon et al., 2001; Annesley et al., 1990). Although the alterations in gait of older adults indicate a progression toward a more safe, secure, and stable gait pattern, the cost of energy output can be significant. As older individuals become more physically or psychologically impaired their mobility performance and skills tend to decrease. Further, physical impairments such as loss of bone and muscle mass can often occur as a result of decreased mobility, causing even less mobility: therefore a spiral decline begins. Significant differences in biomechanical walking patterns are found between healthy older and younger adults (Winter et al., 1990; Ferrandez et al., 1990). Older adults have: Risk factors for decreased ambulation and related falls can be categorized into two groups: intrinsic and extrinsic. Intrinsic factors are those specific to the individual resident and include: A shorter step length; Decreased velocity; Increased double-support stance period (the stage of walking in which both feet are touching the floor); Decreased push-off power, a more flatfooted landing, and a reduction in their index of dynamic balance. Walking Improvement Advanced age; Medication use (antidepressants, antihypertensives, and antipsychotics); 1 Chronic diseases (chronic obstructive pulmonary disorder, arthritis, congestive heart disease, and Parkinson’s disease); Daily alcohol consumption; Impaired cognition; Decreased visual acuity; Incontinence; Self-reported decline in health status; Factors related to muscle strength, mobility, flexibility, cardiovascular conditioning, and balance; and/or Additional factors may include falls resulting in fractures or fear of falling, decreased endurance due to acute illness, infections, or psychological changes. residents not carried out correctly or not addressed at all. Basic daily needs such as feeding, medications, and toileting become the primary concern and there isn’t additional time to address activities such as walking or exercise. When facilities are understaffed, caregivers may assume it is more efficient to transport residents by wheelchair rather than supervised walking. This may be realistic as an immediate solution; however over time, if the residents were able to become independent ambulators the caregivers would spend less time transporting residents within the facility. High staff turnover rates can also be detrimental to existing programs designed for individuals in nursing homes. New staff members are often not educated on individual programs and can be unaware of their role in walking improvement. Therapy teams also share this frustration as they work individually with the residents to gain progress and then have concerns regarding the follow through and support that will be available after discharge. Staff education and training must be very comprehensive during orientation, and must be continual thereafter. Strong leadership and support must also be given to these programs by supervisors and administrators. Extrinsic factors include: Social issues such as living alone; Personal factors such as level of risktaking behaviors (Nowalk et al., 2001); and/or Environmental hazards that pose risks for falls include: cluttered hallways or living spaces, wet floors, presence of loose carpets or rugs, lack of grab bars, poor furniture arrangement, and lack of adequate lighting (Jensen et al., 2002). Motivation can have significant impact on a resident’s physical functioning. Resnick (1998) suggests that residents who are motivated to improve had increased participation and improved functional outcomes. The presence of depression was found to have a significant correlation to a decline in functional abilities, however it may be because it has an impact on motivation. Benefits of Effective Walking Improvement Programs Benefits from programs or interventions producing walking improvement include “increased socialization, greater independence in functional areas, improved posture, balance, coordination, cardiac conditioning, and relief from stress” (Norman & Gibbs, 1991). “Progressive resistive strength training interventions can improve lower extremity strength, balance, and performance in nursing home residents” Barriers to Successful Walking Programs Nursing departments are often under staffed resulting in individualized programs for Walking Improvement 2 (Resnick, 1998). Jivorec (1991) reports multiple benefits identified in a literature review of various exercise regimens as: “increased physical work capacity, increased muscle strength, improved aerobic capacity, increased joint flexibility, improved body image, and increased life satisfaction.” Also, “increases in range of motion and flexibility and decreases in recovery heart rate, aches, and pains.” Psychologically, residents “demonstrated significant improvement in morale and attitude toward their own aging” (Jivorec, 1991). Balance training with beanbags, balls, and balloons; Flexibility exercises; and Walking. Research of Walking Improvement Programs Program #2: A Six-Month Walking Program Koroknay (1995) conducted a six-month walking program in order to promote functional mobility in the frail nursing home population. Twenty residents who would not or could not ambulate without the assistance of staff were identified based on initial assessments completed by the nursing unit manager and the gerontological clinical nurse specialist (GCNS). The goal was “to establish a nursing procedure that focuses on the resident’s need to walk, and to improve or maintain the ambulatory status of the frail elderly… this goal was accomplished by making walking a regular part of the day’s activities rather than an additional ‘task,’ and by holding a nursing assistant accountable for walking residents.” Their program included the following key points: The FFLTC demonstrated greater functional outcomes than standard seated ROM exercise programs and it can be individualized to the resident’s abilities. The program also has additional benefits, as it can be safely implemented by nursing home staff, caregivers, or volunteers with minimal education and low cost. The majority of nursing homes offer exercise and walking programs for their residents, but recent research shows that how the program is organized makes a big difference in resident outcomes. Here are some ideas about how to make your program successful from a series of studies that have improved outcomes for residents: Program #1: The Functional Fitness for Long-Term Care (FFLTC) Program The FFLTC (Lazowski et al., 1990) was designed not only to maintain upper and lower extremity range of motion (ROM), but also to improve strength, balance, flexibility, mobility, and function. It requires simple equipment and minimal training. Families, volunteers, or nursing home staff can administer the program. Nursing home residents were randomly assigned to 2 groups: ROM exercises only, or FFLTC. Each program was conducted for 45 minutes, three times per week, for four months. Key components of the FFLTC program included: Nursing assistants assured that residents ambulated; The focus was on maintaining mobility in frail nursing home residents who required assistance with walking; Schedules and goals were coordinated with the nursing unit’s activities (meals) and the residents’ daily activities (using the restroom); and The residents who were participants in the program experienced an increase in Progressive strengthening with resistive exercise bands and ankle/wrist weights; Walking Improvement 3 “The exercise should be designed both to gradually extend the resident’s exercise tolerance and to be performed on a schedule that maximizes the efficient use of staff time.” their functional ambulation and a decrease in falls. Staff was educated regarding the objective of the program, benefits of walking and exercise, and the dangers of immobility. The environment was adapted to reflect banners and distance markers for encouragement and motivation. New residents were assessed upon admission, existing residents were continually reassessed, and goals revised if needed. Results of the program reflected a significant improvement in ambulatory status, and the percentage of residents who fell decreased from 25% to 5%. Koroknay also found that the residents with cognitive impairments benefited as much as the residents who were cognitively intact. Residents were given individualized goals for mobility and for standing tolerance. The average walk time of ambulatory residents involved in the FIT program increased from 30 minutes a week to 55 minutes. The average sit to stands performed in a day improved from 3.4 to 10. The control group did not change significantly for either activity. Designing the FIT program to be implemented by nurses aides while performing other care routines has the advantage of time management as it only required an average of six minutes more per session than the PV only. Program #3: Functional Incidental Training (FIT) The FIT program walking is integrated with prompted voiding (PV), which is a behavioral intervention shown to decrease the severity of incontinence. Seventy-six residents participated in the program for eight weeks. The subjects were randomly divided into two groups, one integrated the FIT program with PV and the other was PV only. Every two hours between 8:00 a.m. and 4:00 p.m. five days a week the residents were approached for toileting needs. The subjects receiving the FIT protocol were encouraged to participate in transfers, ambulation, and standing activities along with toileting assistance. The control group was given socialization and toileting assistance. The FIT program was developed around three principles: Program #4: Walking Program The residents walked five days a week for four weeks. The intervention lasted approximately 30 minutes per day and the residents were verbally encouraged to walk as far as they could without taking a break. At the beginning of the study the subjects walked an average of 50 feet before they were fatigued. After the study the residents walked an average of 73 feet. Only two of the 15 subjects could rise independently out of a chair before the intervention opposed to six after daily exercise. Three residents could walk unassisted before the program compared to five at the end of the fourth week. The frequency of urinary incontinence was significantly decreased during the day shift from an average of 2.33 incontinent episodes to an average of one. The prevalence of urinary incontinence can be impacted by the interventions of caregivers, and is related to muscle atrophy and loss of function such as walking that often occurs in a nursing home setting (Jivorec, 1991). “The exercise should be integrated into the PV incontinence care routine”; “Emphasis should be placed on the repetition of exercises that are specific to the functional skills involved with toileting and other activities of daily living”; and Walking Improvement 4 social group had individual social visits for 30 minutes. The results showed significant progress. The subjects in the walking program increased their maximal walk endurance time by 77%, and distance by 92% (MacRae et al., 1996). Program #5: Walking Programs for Residents with Alzheimer’s Disease (AD) One of the barriers identified by Tappen et al. (2000) of an effective ambulation program for individuals with AD is compliance with the intervention. In their study, 65 residents with AD were randomly assigned to treatment groups of assisted walking, walking combined with conversation, and conversation-only. Interventions were provided for 30-minute intervals three times a week for 16 weeks. Residents in the assisted walking group declined with functional mobility by 20.9%, the conversation-only group declined by an average of 18.8%, and the combined walking and conversation group declined only 2.5%. Residents in the conversationonly group had a compliance rate of 90%, the combined group averaged 75% compliance, and the ambulation only achieved a compliance rate of 57%. The conversation element of the intervention appears to have improved compliance of the residents. Based on the results of this study, Tappen et al. (2000) suggest that assisted walking with conversation can contribute to maintenance of functional mobility, specifically ambulation, for individuals with Alzheimer’s disease in nursing homes. Summary of Key Elements to a Successful Walking Improvement Program Many interventions for walking improvement have been initiated since the Omnibus Budget Reconciliation Act (OBRA) of 1987, which emphasized the necessity for long-term care facilities to maintain and promote higher levels of functioning. Programs require support by the entire interdisciplinary team and are typically implemented by physicians, restorative personnel, therapists, gerontological clinical nurse specialists, or nursing unit managers. Responsibilities of the team should include: Making initial assessments of functional mobility status Determining the potential of walking improvement Developing goals consistent with residents’ needs and capabilities Assessing current medications that may affect balance or ambulation potential and adjust or delete as needed Providing continual education and communication with the resident and family or caregivers regarding status and plan of care Implementing and maintaining the program on a daily basis Program #6: A Walking Improvement Program MacRae et al. (1996) conducted a 12-week walking program to determine the effects on walk endurance capacity, physical activity level, mobility, and quality of life in ambulatory nursing home residents who had been identified as having low physical activity levels and low walk endurance capacities. The subjects were divided into two groups, a walking program or a social program. The residents in the walking program ambulated five times a week up to 30 minutes a day for 12 weeks. The control Walking Improvement Staff members must be aware of the goals, purpose, and design of the program in order to be effective and accountable. The elements of successful treatment according 5 to Tinetti (1986) are: “correct exercise prescription, good supervision, continuity and persistence, and stepwise progression.” falls, and tracked when the falls normally occurred. They determined the majority of falls occurred between 11:00 a.m. - 3:00 p.m. The staffing schedule was adjusted and a new position titled “Special Care C.N.A.” was created with the redistributed hours. This new position “concentrates on residents who require special attention at the busiest times of the day with tasks such as showering, walking to events, or assistance with one-on-one activities” (Crotty, 1999). In the following quarter the fall rate decreased by 15%. Additional approaches included individualized prevention programs following changes in psychotropic drug plan, and reviewing resident care plans during morning interdisciplinary meetings the day after a fall. An interdisciplinary focus was important to ensure staff awareness to residents at risk. Documentation of data such as time of fall, date, and injuries sustained, is essential in identifying results of the program and areas of improvement. Norman and Gibbs (1991) also support a model of an interdisciplinary team approach. In this model physical therapists make referrals to nursing for residents currently on therapy caseload who could benefit from additional ambulation practice on the unit with supervision by the nursing staff. Therapists provide education and training to the nursing staff regarding the resident’s potential and functional skills, and provide gait and balance assessments to measure baseline status and progress throughout the course of stay in the facility. Nursing staff that recognize a change in condition of the resident’s mobility status request an evaluation by a physical therapist. The gerontological clinical nurse specialist offers initial and reassessments for appropriateness of admission into the program, and medication adjustments are made through collaboration with the physician. Volunteers assist by providing incentives such as certificates or awards, and providing refreshments for the program. Further responsibilities include environmental or maintenance personnel to help with marking the distances in the hallways or environmental modifications, the activities department to keep a record of progress in a main area with the resident’s consent, social services to inform families and caregivers of the resident’s progress, and dietary to recommend supplemental nutrition to increase energy. Walking interventions should include components such as: strength and balance training, endurance training, cardiovascular conditioning, and motivational persuasion. According to Norman and Gibbs (1991), intervention strategies should involve reassurance, praise, encouragement, verbal goal reminders, and incentives for participation. Residents should be encouraged to set their own goals. The more control they have over their own progress the more motivation and ownership they will exhibit throughout the program. Residents may develop their treatment plan to include when they walk, how far, time of day, which route to take and offer suggestions for the program (Norman and Gibbs, 1991). Determining underlying causes of decreased mobility can also be an important aspect. Norman and Gibbs suggest beginning by identifying residents who ambulate and do According to Crotty (1999), one long-term care facility was able to turn their falls prevention program into a best practice with individualizing the program according to their facility’s needs. The quality improvement team reviewed residents’ records and identified all residents at risk for Walking Improvement 6 not use a wheelchair, those who are unable to ambulate, and those who can ambulate but use a wheelchair. Pawlson et al. (1986) interviewed 50 residents who used wheelchairs but could ambulate and found the three reasons cited most often were fear of falling, they could get around faster, and they get too tired when they walk, respectively. Further investigation from that point may assist in reducing dependent mobility patterns. Ferrandez AM, Pailhous J, and Durup M. Slowness in Elderly Gait. Experimental Aging Research. 1990; 16: 79-89. Jensen J, Lundin-Olsson L, Nyberg L, and Gustafson Y. Fall and Injury Prevention in Older People Living in Residential Care Facilities: A Cluster Randomized Trial. Annals of Internal Medicine. 2002; 136: 733-741. Jivorec MM. The Impact of Daily Exercise on the Mobility, Balance, and Urine Control of Cognitively Impaired Nursing Home Residents. International Journal of Nursing Studies. 1991; 28(2): 145-151. Comprehensive programs involving rehabilitation and discharge from the facility to a lesser level of care should include balance and gait training, walking on uneven surfaces, on carpeted floors, negotiating stairs, maneuvering through obstacles, walking outside on sidewalks using curbs, and practicing car transfers. The best opportunity to predict success in the subsequent environment is to perform an onsite evaluation with the resident present. If family members or other caregivers will be involved in the follow-up care, it would be helpful to have them attend for educational purposes. Further therapy provision by caregivers or home health therapists may be needed once the resident is discharged from the facility to assist the resident with achieving their highest possible level of independent ambulation. Koroknay VJ, Werner P, Cohen-Mansfield J, and Braun JV. Maintaining Ambulation in the Frail Nursing Home Resident: A Nursing Administered Walking Program. Journal of Gerontological Nursing. 1995; 21(11): 18-24. Lazowski DA, Ecclestone NA, Myers AM, Paterson DH, Tudor-Locke C, Fitzgerald C, Jones G, Shima N, and Cunningham DA. A Randomized Outcome Evaluation of Group Exercise Programs in Long-Term Care Institutions. Journal of Gerontology: Medical Sciences. 1999; 54A(12): M621M628. MacRae PG, Asplund LA, Schnelle JF, Ouslander JG, Abrahamse A, and Morris C. A Walking Program for Nursing Home Residents: Effects on Walk Endurance, Physical Activity, Mobility, and Quality of Life. Journal of the American Geriatrics Society. 1996; 44: 175-180. References Annesley AL, Almada-Norfleet M, Arnall DA, and Cornwall MW. Energy Expenditure of Ambulation Using the Sure-Gait® Crutch and the Standard Axillary Crutch. Physical Therapy. 1990; 70: 18-23. McGibbon CA, Puniello MS, and Krebs DE. Mechanical Energy Transfer During Gait in Relation to Strength Impairment and Pathology in Elderly Women. Clinical Biomechanics. 2001; 16(4): 324-33. Crotty MT. Setting Best Practices in Motion. Provider. 1999; 25(7): suppl 7,10. Walking Improvement 7 Norman G and Gibbs J. Why Walk When You Can Ride? Clinical Ambulation Incentives for the Immobile Elderly. Journal of Gerontological Nursing. 1991; 17(8): 2933. Changes in the Fit and Healthy Elderly. Physical Therapy. 1990; 70: 340-347. Nowalk MP, Prendergast JM, Bayles CM, D’Amico FJ, and Colvin GC. A Randomized Trial of Exercise Programs Among Older Individuals Living in Two Long-Term Care Facilities: The FallsFREE Program. Journal of the American Geriatrics Society. 2001; 49(7): 859-65. Pawlson G, Goodwin M, and Keith K. Wheelchair Use by Ambulatory Nursing Home Residents. Journal of the American Geriatrics Society. 1986; 34(12): 860-864. Resnick B. Functional Performance of Older Adults in a Long-Term Care Setting. Clinical Nursing Research. 1998; 7(3): 230249. Schnelle JF, MacRae PG, Ouslander JG, Simmons SF, and Nitta M. Functional Incidental Training, Mobility Performance, and Incontinence Care with Nursing Home Residents. Journal of the American Geriatrics Society. 1995; 43: 1356-1362. Tappen RM, Roach KE, Applegate EB, and Stowell P. Effect of a Combined Walking and Conversation Intervention on Functional Mobility of Nursing Home Residents with Alzheimer Disease. Alzheimer Disease and Associated Disorders. 2000; 14(4): 196-201. Tinetti ME. Performance-Oriented Assessment of Mobility Problems in Elderly Patients. Journal of the American Geriatrics Society. 1986; 34(2): 119-126. Winter DA, Patla AE, Frank JS, and Walt SE. Biomechanical Walking Pattern Walking Improvement 8