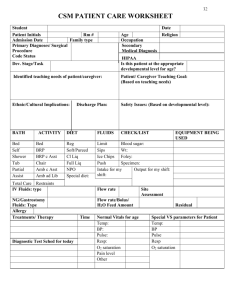
Patient Care Worksheet for Nursing Students
advertisement

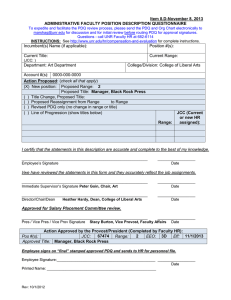
CSM PATIENT CARE WORKSHEET Student: ________________________________ Date: ___________________________ Patient’s Initials: ________ RM#: ______ Age: _____ Sex: _____ Religion: ____________________ Code Status: ____________ HIPAA: _____________ Admission Date: ___________ Family Role: __________________ Occupation: ____________________ Primary Medical Diagnoses/Surgical Procedures: _____________________________________________ Dev. Secondary Medical Diagnoses: _____________________ Stage/Task: ____________________________ Identified Teaching Needs: Is this patient at appropriate developmental level for age? Patient Teaching Goal: Ethnic/Cultural Implications: Discharge Goal: Safety Issues: BATH Bed Self Shwr Tub Sitz Partial ACTIVITY Bed BRP BRP c Asst Chair Amb c Asst Amb Ad Lib http://consultgerirn.org/topics/ethnogeriatrics_and_cult ural_competence_for_nursing_practice/ DIET FLUIDS Reg Limit Soft Sips Cl Liq Ice Chips Full Liq Push NPO Intake = Special Diet: _____ Output = CHECK Blood Sugar Wt: ______ Foley Specimen: ____ EQUIPMENT BEING USED IV Fluids: Type: ______________ IV Balance: _________ ________ Rate of Flow: ________ ________ (Beginning) (Ending) (ml/hr) (gtts/min) IV Site Assessment: ____________________________ Tubing Change (date to be done): _______________ Allergies: Treatments/Therapy (lab, radiology, special procedures, etc.) Time Date S: Test Results Diagnostic Tests Scheduled For Today: B: A: R: Significant Diagnostic Data Significance Project Course Related: Prioritize System ASSESSMENT CRITERIA INTEG: color, temp, moisture, turgor, integrity, scars, incisions, lesions (measure) NEURO: A&O x 4, PERRLA, T= symmetry, facial expressions, EOMs, fine/gross motor fxn, MAE, grips, sensation, speech, strength *RESP: rate, rhythm, depth, R= effort, breath sounds, O2 sat, incentive spirometry, m. membranes *CV: pulses, capillary refill, B/P= edema, CSM *GU: amount, urine characteristics, bladder distention, ext. genitalia GI: intake, appetite, BM, bowel sounds, distention *MS: ROM, spine, MAE, strength ASSESSMENTS/OBSERVATIONS Day 1 Day 2 T= R= Apical P= Radial P= B/P= EENT: vision, glasses, ENT discharge, hearing, hearing aid, dentures, nares, lymphadenopathy EMOT/PSYCH: affect, mood, cooperation, family support systems PAIN: location, intensity, characteristics, pharmacological and nonpharmacological interventions SLEEP/REST: http://consultgerirn.org/topics/s leep/want_to_know_more/ *Include any accessory equipment used on patient (monitor, 02, foley) Primary Patient Goal: TIME PLAN TIME MANAGEMENT PLAN ANALYSIS OF DAY Apical P= Radial P= PATIENT CARE PLAN DATA [Indicate subjective (s) & objective (o)] #1 #2 NURSING DIAGNOSIS Goals (short and long term) O. CRITERIA (with deadline) N. INTERVENTIONS (Rationale with references) EVALUATIONS Time Medication Dosage/ Frequency/Route Reason/Parameters Side Effects/Nursing Implications