Discussion of Misery
advertisement

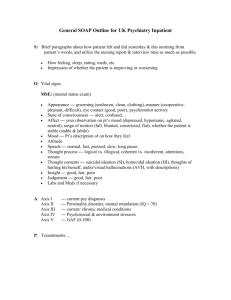
Discussion of “Misery” When a clinician attempts to obtain a history from a patient, there is a basic assumption that the patient is doing the best that he or she can do to provide accurate information. In this case, the referral was triggered by noncompliance with the surgeon’s therapeutic recommendation. The first suggestion that things might not be as they appeared was the patient’s striking nonchalance about her disability (the leg amputation)-referred to as la belle indifference. Suspicions were further raised when additional history became available from her previous surgeon. Finally, compelling evidence was obtained that indicated that she had deliberately produced many of her puzzling physical symptoms and metabolic abnormalities, suggesting a diagnosis of either Factious Disorder or Malingering. The distinction between these two conditions depends on the underlying motivation. In Malingering, there are clear external incentives-for example, the man who, in order to avoid military service, puts sugar in his urine to simulate diabetes. In contrast, in Factitious Disorder the motivation is presumed to be a psychological need to assume the sick role. In this case, there does not appear to be any clear external incentives and one can only presume that, for unknown reasons, Ms. Sandler has a pathological need to perpetuate being a medical patient. Because her symptoms are primarily physical, the Axis I diagnosis would be Factitious Disorder with Predominantly Physical Signs and Symptoms (DSM-IV, p. 474), a disorder that was first called Munchausen syndrome, after an eighteenth-century baron who wrote many fantastic tales. We assume that people with Factitious Disorder also have severe personality disturbance. However, in the absence of any specific information about this patient’s long-term personality functioning, we would note Diagnosis Deferred on Axis II. On Axis III we list the left leg amputation and her recent spinal fusion. Undoubtedly, Ms. Sandler has multiple psychosocial problems, but because of lack of any specific information, at this point we note Deferred on Axis IV. Her Axis V GAF rating of 33 reflects her major impairment in her thinking and judgment. Multiaxial Evaluation Axis I Factitious Disorder With Physical Signs and Symptoms Axis II Diagnosis Deferred Axis III Left leg amputation, recent spinal fushion Axis IV Deferred Axis V GAF=33 (current) Follow-up A team meeting was convened, and Ms. Sandler was told that it was suspected that she had factitious symptoms, implying that she was actively involved in inducing at least some of her symptoms. She was informed that this is a serious and potentially lifethreatening mental illness, and that inpatient psychiatric hospitalization was recommended for further evaluation and management. She did not comment on the diagnosis, appeared unconcerned, and agreed to transfer to a psychiatric ward. Ms. Sandler was in an acute psychiatric unit for 4 months. During that time she developed no new medical problems and made no complaints of pain of physical discomfort. Instead, she developed a series of psychiatric symptoms. She initially presented with rapid alternations of mood, appearing first hypomaniac, racing around the unit in her wheelchair and claiming to be u all night, then depressed, curling up on her bed with the lights out, refusing to eat or interact with others. Her presentation was thought by some staff members to result from factitious Bipolar Disorder, whereas others attributed her symptoms to genuine affective instability or true dissociative phenomena. Ms. Sandler’s behavior on the unit was provocative and impulsive. She was labile and suspicious. She split staff, threw tantrums, said she was suicidal, and barricaded herself in a room. She improved on an anticonvulsive medication and an antipsychotic but nevertheless spend the second half of her hospitalization refusing to participate in activities with restricted privileges because of her threats of self-destructive behavior if she was allowed to leave the unit. In psychotherapy, she gradually revealed a history of daily physical abuse at the hands of her parents throughout childhood and early adolescence. Her therapist believed that this history was genuine and diagnosed a Dissociative Disorder on the basis of the symptoms she described. Other staff members remained unconvinced of the veracity of her story of childhood abuse, but were impressed with the array of features characteristic of Borderline Personality Disorder. Ms. Sandler agreed to a voluntary transfer to long-term hospitalization. One day before the planned transfer, she changed her mind, saying she wanted to “get on with my life,” and submitted a sign-out letter. She went to court, where she was granted discharge by the judge. She signed out against medical advice, and was lost to follow-up.