File
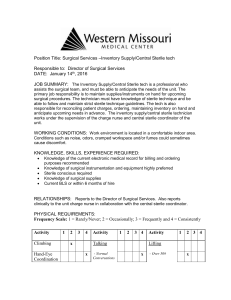
advertisement

THE INTRAOPERATIVE PERIOD - - Begins when the patient is transferred onto the OR table and ends with admission to PACU Scope: o Provide patient safety and well being o Protects clients dignity and interests while the pt is anesthetized o Coordinates the OR personnel o Maintain an aseptic environment o Ensure proper function of equipment o Provide the surgeon with specific instruments and supplies for the surgical field o Identify and minimize risks and complications o Complete appropriate documentation Activities: o Provide emotional support o Assist in positioning the patient o Acts as a scrub/circulating/ staff nurse STUDENTS’ POLICIES and Policies Concerning Nursing Responsibilities Perioperatively 1. Students are expected to wear their complete duty uniforms when reporting to the Operating Room Department and will change into their operating theater suit inside the Student’s Dressing Room. 2. Nameplate is considered part of the uniform. 3. Operating Room bonnet or cap must cover the hair and ears completely. 4. Students requested for errand outside the operating room must change their operating room gown to a complete duty uniform. 5. The Operating Room is not a place of social discourse therefore thoughtless comments and laughing are discouraged. 6. Bringing of digital and electronic devices inside the Operating Theater is highly discouraged. 7. Each student is required to perform a return demonstration after the clinical instructor has demonstrated stated procedures inside the mock Operating Room of the College of Nursing. 8. After each assisted case, the student is given three days to accomplish all the requirements and submit it to his/her respective clinical instructor. 9. Circulating student nurses are not allowed to leave the operating theater for the duration of the entire surgical procedure unless given permission to do so or with enough reason to perform such. 10. The immediate post-operative intervention and monitoring of the patient must be taken care of by the respective student circulating nurse. THE SURGICAL ENVIRONMENT: PRINCIPLES OF SURGICAL ASEPSIS 1. All articles used in the operation have been sterilized previously. 2. Persons who are sterile will only touch the sterile articles. 3. If in doubt about the sterility of anything consider it non sterile. 4. Non – sterile persons should avoid reaching over a sterile field; sterile persons must avoid leaning over an unsterile area. 5. Tables are sterile only at table level. 6. Gowns are considered sterile only from waist to shoulder level and in front including the sleeves. 7. The edge of anything that encloses sterile contents is considered unsterile. a. Sterile persons should only be within the sterile area. b. Sterile persons stand back at a distance from the operating table when draping the patient. c. Should pass each other back to back. d. A sterile person turns his back to a non-sterile person or area when passing. e. A sterile person faces a sterile area when passing it. f. A sterile person should not wander around the operating room. 8. Sterile persons keep in contact with sterile areas to a minimum. 9. When bacteria cannot be eliminated from a field they must be kept to a minimum. 10. Surgeon makes an effort to sponge only once for mopping, then discards it into a pail or kidney basin. 11. Moisture may cause contamination. When moisture soaks through sterile area to a non-sterile one or vice versa, it provides a means of transporting bacteria to the sterile area. 12. The skin cannot be sterilized. 13. Some areas cannot be scrubbed. 14. Infected areas are grossly contaminated. Intraoperative Ng | 1 THE SURGICAL TEAM: 1. Patient 2. Surgeon 3. Surgical Assistants 4. Anesthesiologist/Anesthetist 5. Nurses; Circulating Nurse, Scrub Nurse DUTIES OF A SCRUB NURSE A. Before the surgeon arrives 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. Prepares the instruments and packs to be used and places them on the Mayo table and back up table. Does a complete scrub according to accepted practice. Does Gowning and gloving. Drape tables as necessary according to standard procedure. Moves remaining contents of the drape pack to a corner of the instrument table if they are not preset on the table drape in a convenient place. Drape the mayo stand. Arranges instruments on the back-up table and count according to the standard basic set or an instrument list for a given operation and the surgeon’s preferences. Arranges instruments on the Mayo stand for making and opening the initial incision. Install blades on knife handles. Prepare sutures in sequence in which the surgeon will use them. Counts surgical needles and other sharp instruments with the circulating nurse according to the accepted practice. Count all sponges with the circulating nurse before doing anything else with them. Fill a syringe with the correct agent if a local infiltration anesthetic is to be used. B. After Surgeon and Assistant(s) Perform Surgical Hand washing 1. Offers sterile towel to the surgeon and assistants as soon as they enter the theater and then serves gown and glove to the surgeon and assistants as soon as they enter the operating room suite. 2. Assist in draping client according to the routine procedures. 3. Request the circulating nurse to move and position the Mayo stand and back table after draping is completed. 4. Serves suction tubing and electrosurgical instrument and if either or both are to be used, attach to drape with a nonperforating clamp. C. During the Operation 1. 2. 3. 4. 5. 6. 7. 8. 9. Hand knife to surgeon and hemostat to assistant. Hand towels and hooks are placed at each side of the incision and secured to cover skin completely during operation. Watches the field and try to anticipate the surgeon’s needs. Hand over sterile instruments in a decisive and positive manner: Place a ligature on the surgeon’s hands. Keep two (2) clean sponges on the field. Saves all specimens of tissues according to hospital policy Perform after care for tissue specimen according to hospital procedure. Maintain sterile technique. Watch for any break. Observe the following points: 9.1 Steps away from sterile when contaminated. 9.2 Change gloves at once and discard needle or instruments if a glove is picked by a needle or engaged by an instrument. 9.3 Discard anything that falls over the edge of the sterile field without touching the contaminated area. 9.4 Keeps hands at waist level when at rest; they should never be below waist. 9.5 Keeps contact to a sterile area to a minimum. 9.6 Leaves a wide margin of safety in moving about the room. 9.7 Do not turn back sterile field or to members of the sterile team. 9.8 Do not reach behind a member of a sterile team, go around. 9.9 Keeps the table and field as dry as possible. 9.10 Discards soiled sponges from the sterile field. 9.11 Keep talking to a minimum. Avoid coughing and sneezing. D. During Closure 1. 2. 3. 4. Count the sponges, instruments, visceral packs and needles with the circulating nurse when surgeon begins closure of the wound, in accordance with established counting procedures. Clear off the Mayo stand as time permits leaving a knife handle with blade tissue forceps, scissors, four hemostats, and two (2) Allis forceps. NOTE: Mayo stand should remain sterile until the patient has left the room. Serves betadinized operating sponge then have a damp sponge ready to wash blood from area surrounding the incision as soon as the skin closure is completed. Have dressing ready. Intraoperative Ng | 2 DUTIES OF CIRCULATING NURSE A. After the Scrub Nurse Scrubs 1. 2. 3. 4. 5. Fasten back of the scrub nurse, surgeon and assistants. Open packages of sterile items such as syringe, suction tubing, sutures, gloves, and sponges. Flip suture packets unto the instrument table, or open over wraps for scrub nurse to take packets. Pours little amount of solution (usually normal saline) into the pail before pouring it into the basin. Counts sponges, sharps instruments, needles and visceral packs with the scrub nurse as required by hospital policy and procedure. Record immediately. B. After the Patient Arrives 1. Greet and identify patient. Introduce yourself to the patient. Check wristband for identification by name and hospital number if applicable. 2. Check nursing care plan and patient’s chart for pertinent information including consent. 3. Cover patient’s hair with a cap to prevent dissemination of microorganism, to protect it from being soiled and to prevent static sparks near the anesthesia machine. 4. Take patient into the operating room after the surgeon sees him and the anesthesiologist is ready for induction. 5. Assist the patient in moving from the stretcher to the operating table. 6. Apply restraints completely. 7. Help anesthesiologist, surgeon or assistant to start IVF. C. During Induction of General Anesthesia 1. Stay in the room and near the patient to comfort him or her with the anesthesiologist in the event of excitement or any other contingency occurs. 2. Be quiet as possible. D. After the Patient is Anesthetized 1. Reposition only after anesthesiologist says the patient is anesthetized to the extent that he/she will not be disturbed by being moved or touched. 2. Attach anesthesia screen and after table attachments as needed. 3. Note patient’s position to be certain all measures for his safety have been observed. 4. Place inactive electrode pad or plate in contact with the patient’s skin. 5. Expose appropriate area for skin preparation. 6. Turn on overhead spotlight over site of incision. 7. Arrange sterile prep tray and pour solutions if this has not been done. 8. Cover prep-tray immediately after use. E. F. After Surgeon and Assistant(s) Perform Surgical Hand washing 1. Assist with gowning. 2. Observe for any breaks in technique during draping. 3. Assist scrub nurse in moving Mayo stand and or back instrument table being careful not to touch in drapes. 4. Focus overhead operating light on site of incision, unless sterile handless will be used. 5. Set platform or foot stools for team members who need them or place stools in position for surgeon who prefers to operate seated. 6. Position kick buckets on each side of the operating table and splash basin if any near the surgeon. 7. Connect suction tubing to suction machine if necessary. 8. Connect electrosurgical electrodes and or any other electrical equipment to be used. Place foot pedals within easy reach of the surgeon’s foot. Tell surgeon the setting of all machines. During Operation 1. Be alert to anticipate needs of sterile team such as adjusting operating light, removing perspiration from brows, and keeping scrub nurse supplied with sponges, sutures, saline etc. 2. Stay in room as much as possible. 3. Keep discard sponges carefully collected, separated by sizes and counted. 4. Weigh sponges for blood loss as requested. 5. Obtain blood products for transfusion if necessary. G. During Closure 1. Count sponges, instruments, needles and visceral packs with the scrub nurse. Complete count record. Collect spoiled and place into plastic-lined bucket. 2. If another patient is scheduled to follow: a. Call ward at least 45 minutes before the schedule time of operation to request that the operative medications be given. b. Send an Institutional Worker for patient and notify unit to transport the patient. 3. Prepare for room clean-up at a minimal time. Check with scrub nurse before leaving. 4. Send for recovery room stretcher or bed with a clean sheet, whatever is the practice. H. After the Operation is Completed 1. Open neck and back closure of gowns of surgeons and the assistants so they can remove them without contaminating themselves. 2. Assist with outer layer of dressing. 3. See the patient lies in clean or dry drapes. Wash off blood, feces or plaster. Put on a clean gown and blanket. 4. Have an Institutional Worker bring in clean recovery room stretcher. 5. Help move patient to stretcher or bed. Before moving a patient from the operating table, be sure all arm and leg restraints and table appliances have been removed. 6. Secure IV solution bags on a stand and attached preferably near foot end of the stretcher or bed. 7. Connect all drainage systems as indicated. 8. Be sure chart and proper records, including the Nursing Care Plan accompany the patient. 9. Have nursing assistant assist anesthesiologist in taking patient to recovery room, IV or nursing unit. Intraoperative Ng | 3 THE SURGICAL EXPERIENCE: 1. ANESTHESIA 2. POSITIONING ANESTHESIA types: 1. 2. General Anesthesia Balance Anesthesia 1. General Anesthesia Blocks pain stimulus at the cerebral cortex and induce depression of the CNS that is reversed by metabolic changes and elimination from the body or by pharmacologic means. Produce analgesia, amnesia, unconsciousness and loss of reflex. two methods of administering general anesthesia: 1. inhalation- e.g. halothane (fluotane), enflurane (Ethrane), isoflurane (Forane), sevoflurane (Ultrane) 2. intravenous injection- Substances include: benzodiazepines, barbiturates, opioids, dissociative agents 4 Stages of General Anesthesia: a. Onset/ Beginning b. Excitement c. Surgical Anesthesia d. Dangerous/Medullary Depression - Care of Anesthetized Patient - Team member especially the circulating nurse and anesthesiologist must be constantly aware of potential trauma to the patient since he/she is unable to produce a normal response to painful or injurious stimuli. - The patient’s position must be changed slowly and gently to allow circulation to readjust. - Patient’s ability to detoxify anesthetic agents and rate stress differ greatly, but any anesthetized patient has diminished ability to comprehend for physiologic changed caused by motion or operative conditions. - Anesthetic agents are basically depressants that affect the vasomotor and respiratory centers, predisposing the patient to postoperative respiratory complications. 2. Balance Anesthesia refers to a combination of agents used to provide hypnosis, analgesia, muscle relaxation and obtunding of reflexes with a minimum disturbance of physiologic functions variations/types: a. Conscious Sedation b. Regional Anesthesia c. Conduction Blocks d. Local Infiltration Anesthesia a. Conscious Sedation- Midazolam or Diazepam is frequently used for intravenous conscious sedation. b. Regional Anesthesia- Anesthetic agent is injected around the nerves so that the area supplied by these nerves is anesthetized. c. Conduction Blocks Spinal Anesthesia- A type of extensive conduction nerve block that occurs by introducing a local anesthetic into the subarachnoid space at the lumbar area between L4 and L5 - Nausea, vomiting, pain and incidence of headache are common side-effects. Epidural Anesthesia- Achieved by injecting a local anesthetic into the spinal canal in the space surrounding the dura mater. Other Nerve Blocks: - Brachial Plexus block – produces anesthesia of the arm - Paravertebral anesthesia- produces anesthesia of the nerves supplying the chest, abdominal wall and extremities. - Transsaccral (Caudal) block- produce anesthesia of the perineum and lower abdomen. d. Local Infiltration Anesthesia- Injection of a solution containing the local anesthetic into the tissue at the planned incision site. Intraoperative Ng | 4 POSITIONING (SURGICAL POSITIONS) The position in which the patient is placed on the operating table depends on the surgical procedure to be performed as well as on the physical condition of the patient. Factors to consider includes the following: - The patient should be in as comfortable a position as possible, whether asleep or awake - The operative are must be adequately exposed. - The vascular supply should not be obstructed by an awkward position or undue pressure on a part. - There should be no interference with the patient’s respiration as a result of pressure of the arms on the chest or constriction of the neck or chest caused by a gown. - Nerves must be protected from undue pressure, improper positioning of the arms, hands, legs, feet may cause serious injury or paralysis. Shoulder braces must be well padded to prevent irreparable nerve injury, especially when the Trendelenburg position is necessary. - Precautions for patient safety must be observed, particularly with thin, elderly, or obese patients. - The patient needs gentle restraint before induction, in case of excitement. - Arms are secured with the lift sheet or placed on arm boards. - Used for procedures on the anterior surface of the body, such as abdominal, abdominothoracic and some lower extremity procedures. Types of Surgical Position: 1. Supine 2. Trendelenburg 3. Reverse Trendelenburg 4. Fowlers Position 5. Lithotomy Position 6. Prone Position 7. Modified Prone Position 8. Lateral (Side-Lying) Position - Modifications of the supine position are used for specific body areas: 1. Supine- lying down with the face up, as opposed to the prone position, which is face down. (a)Procedures on the face or neck Neck may be slightly hyperextended by lowering the head section of the operating bed or by placing a shoulder roll. Head may be supported on a head rest or donut and/or turned toward the unaffected side. Eyes are protected from injury by shields, goggles, or nonallergic tape. (b) Shoulder or anterolateral procedures A small sandbag, water bag, roll or pad is placed under the affected side to elevate the shoulder off the operating bed for exposure. Length of body is stabilized to prevent the spine from rolling or twisting. Hips and shoulders should be kept in a straight plane. Operating bed can also be tilted laterally to elevate the affected part. (c)Dorsal Recumbent position For some vaginal or perineal procedures. Patient in supine position except that the knees are flexed upward and the thighs are externally rotated. Soles of the feet rest on the Operating bed. Pillows maybe placed under the knees if needed for support. (d) Modified dorsal recumbent (frog-legged) position For some surgical procedures on the region of the groin. Patient lies on back with arms at sides. Knees are slightly flexed with pillow under each knee. Thighs are externally rotated. (e) Arm extension For surgical procedures of the breast, axilla, upper extremity or hand. Arm on the affected side is placed on an arm board or upper extremity table extension that locks into position at right angle to the body. Hyperextension of the arm is avoided to prevent neural or vascular injury, such as brachial plexus injury or occlusion of the axillary artery. The arm board is well padded. 2. Trendelenburg Position 3. Reverse Trendelenburg Position- Patient lies on back in supine position with soft roll under shoulders for thyroid, neck or shoulder procedures. The entire operating bed is tilted 30-40 deg. So the head is higher than the feet; a padded foot board is used to prevent the patient from sliding toward the tilt. Thigh safety belt is positioned 2 inches above the knees. Intraoperative Ng | 5 - Small pillow may be placed under the knees and the lumbar curvature. Venous stasis can cause complications, and prevention of deep vein thrombosis is an important consideration. The use of sequential compression devices, antiembolic stockings, or foot pumps is suggested to improve venous return. 4. Fowler’s Position- Patient on his back with the buttocks at the flex in the operating bed and the knees over the lower back. (a)Sitting Position (High-fowler’s) (b) Beach chair or modified sitting position Arms are typically placed across the abdomen, and a safety strap is across the thighs. Head and feet are elevated 10-20 degree angle above the level of the heart. 5. Lithotomy Position- Used for female pelvic exam Client lies on back with the knees well flexed and separated Frequently stirrups are used ( adjust for proper feet and lower leg support) 6. Prone Position- Client lies on his abdomen Head turned to one side on small pillow or a flat surface Small pillow just below diaphragm to support lumbar curve, facilitate breathing, and decrease pressure on female breasts. Pillow under lower leg to reduce plantar flexion and flex knees. May be modified in amputees where flexion of hips and knees may be contraindicated. 7. Modified Prone Position (a) Kraske (Jackknife position) Patient remains supine until anesthetized and then turned into his abdomen (prone position) Hips over the center break of the operating table. Chest rolls or bolsters are placed to raise the chest. Arms on arm boards with elbows fixed and palms down Head to the side and supported on a donut or pillow. Feet and toes rest on pillows. Safety belt placed below the knees. Leg section is lowered at desired amount and operating bed tilted head downward to elevate hips above the rest of the body. (b) Knee-Chest position Client first lies on the abdomen with head turned to 1 side on a pillow Arms flexed to either side of the bed. Finally the client is assisted to flex and draw knees up to meet the chest 8. Lateral (Side-Lying) Position Client lies on his side Pillow under neck to prevent lateral neck flexion and fatigue Both arms are slightly flexed in front of the body. Rolled pillow behind client’s back. (a)Sims recumbent position A modified left lateral recumbent position Similar to lateral, but with weight supported on anterior aspects of the ileum, humerous, and clavicle. Client placed on side with head turned to side on a pillow. Upper arm flexed in front of body and supported by a pillow. Upper leg is sharply flexed over pillow with the lower leg slightly bent. (b) Kidney position Patient is in lateral position with kidney region over operating bed break, or body elevation bar. Table is flexed, straps across hips to stabilize the body Raised kidney elevator for hyper extending surgical site, and pillow between legs Lower leg is flexed more than the upper leg. Patient’s side is horizontal from shoulder to hip. Arms supported by a double airplane board. (c)Lateral Jackknife position Similar to kidney position, the lateral jackknife position is not well tolerated. Bed is flexed at the level of the patient’s flank or lower ribs; this drops the legs into a dependent position (d) Lateral chest ( thoracotomy) position Turned to unaffected side and positioned as described in lateral position. A gel pad under axilla elevates the surgical site and relieves pressure on the lower arm. SKIN PREPARATION Hair Removal, Depilatory Creams, and Preoperative Showers Intraoperative Ng | 6 DRAPING Is the procedure of covering the patient and surrounding areas with a sterile barrier to create and maintain an adequate sterile field. Eliminates or minimizes passage of microorganisms between non-sterile and sterile areas. during draping of a table or a patient the sterile table is held above the surface to be covered and is positioned from front to back. - CRITERIA TO MEET IN ESTABLISHING AN EFFECTIVE BARRIER. MATERIALS USED MUST BE: Blood and fluid resistant to keep drapes dry and prevent migration of microorganisms. Resistant to tearing, puncture or abrasion that causes fiber breakdown and thus permit microbial penetration Lint-free to reduce airborne contaminants and shedding into the surgical site. Antistatic to eliminate risk of a spark from static electricity. Sufficiently porous to eliminate heat buildup so as to maintain an isothermic environment appropriate for the patient’s body temperature. Drapable to fit around contours of the patient, furniture and equipment. Drape, nonglaring to minimze color distortion from reflected light. Free of toxic ingredients such as laundry residues and nonfast dyes. Flame resistant to self-extinguish rapidly on removal of an ignition source. DRAPING MATERIALS 1. Self-adhering sheets- sterile, waterproof and antistatic and transparent or translucent plastic sheeting may be applied to dry skin. 2. Incise drape- the entire clear plastic drape has an adherent backing that is applied to the skin. This may be applied separately or the sheeting may be incorporated into the drape sheet. The skin incision is made through the plastic. - Skin may be prepped with alcohol and allowed to dry before drape is applied. 3. Towel drape- Towel sheeting has a band of adhesive along one edge. - Used as a draping towel, it will remain on the skin without towel clips. 4. Aperture drape- adhesive surrounds fenestration in the plastic sheeting. This secures the skin around the surgical site. 5. Non-woven fabric disposable drapes- are compressed layers of synthetic fibers combined with cellulose and bonded together chemically or mechanically without knitting, tufting or weaving. - May either be absorbent or non absorbent. - Laser resistant drapes - Thermal drape STYLE/TYPE OF DRAPES: 1. Woven textile fabrics Tightly woven textile fabric may inhibit the migration of microorganisms. Cotton fibers swell when they become wet. This swelling action closes pores so that liquid cannot diffuse through tightly woven fibers. 2. Fenestrated sheets Drape sheet has an opening that is placed to expose the anatomic area where the incision will be made. a. Laparotomy sheet- the longitudinal fenestration is placed over the surgical site on the abdomen, back or comparable area. b. Thyroid sheet- fenestration is transverse or diamond shaped and is positioned closer to the top of the sheet over the neck area. c. Chest sheet- similar to a laparotomy sheet except that the fenestration provides a larger exposure. It is used for chest and breast procedures. d. Hip sheet- covers the orthopedic fracture table, similar to laparotomy sheet but somewhat longer. e. Perineal sheet- is of adequate size to create a sterile field over the patient in the lothotomy position, has 1 or 2 openings to accommodate the perineum and/or rectum. f. Laparoscopy sheet- a combination of laparotomy and perineal sheet. It is used for gynecologic laparoscopy in lithotomy or combined abdomino perineal resection with patient in the lithotomy position. 3. Separate sheets- with smaller opening used for small incisions, such as taking specimens for biopsies, or procedures in the hands or feet. Exposes only the small surgical area and it provides additional drapes on the surgical field. a. Split sheet- same size as laparotomy sheet, one end is cut longitudinally up the middle at least 1/3 the length of the sheet to form 2 free ends. The upper end of the split sheet may be in the shape of a “U” Intraoperative Ng | 7 b. Minor sheet- is 35x45-inch (89X114 cm). If wrapped around the extremity it permits the extremity to remain in the sterile field for manipulation during the surgical procedure. - It is used under an arm to cover an arm board for shoulder, axillary or arm/hand procedures. c. Medium sheet- is about 36x72 inches; used to drape under the legs, as an added protection above or below the surgical area, or for draping areas in which a fenestrated sheet cannot be used. d. Single sheet- is 108x72 inches; folded lengthwise, place above the sterile field to shield of the anesthesia provider and anesthesia machine or other equipment near the patient’s head or operating bed. Also used to cover the pt. and operating bed below the surgical area around the face. e. leggings- leg drapes are supplied to cover the legs of a patient in the lithotomic position. A rectangle approx 36x72 inches is closed in 2 sides to form a tent-like pocket. One open edge is folded into a cuff to protect the gloves from contamination during application. f. stockinette- used to cover an extremity. This seamless tubing of stretchable woven material contours snugly to the skin. The material is very porous and absorbent, so it is not a microbial barrier. 4. Stockinette drape - - BASIC PRINCIPLES OF DRAPING 1. Place drape on a dry area. 2. Allow sufficient time to permit careful applications. 3. Allow sterile space to observe sterile technique. 4. Handle drapes as little as possible. 5. Never reach across the operating bed to drape the opposite side; go around it. 6. Take towels and towel clips, if used, to the other side of the operating bed from which the surgeon is going to apply them before handing them to him/her 7. Carry folded drapes to the operating bed. 8. Once a sheet is in place do not adjust it. 9. In unfolding a sheet from the prepped area toward the foot or head of operating bed, protect the gloved hand by enclosing it in a turned back cuff of sheet provided for this purpose. 10. If a drape becomes contaminated, do not handle it further. Drop it and use another. If the end of the sheet falls below the waist level, do not handle it further. Drop it and use another. If in doubt about the sterility, consider it contaminated. If a drape is incorrectly placed, discard it. The circulator peels it from the operating bed without contaminating other drapes or the prepped area. 11. A towel clip that has been fastened through a drape has its points contaminated. 12. If a hole is found in a drape after it is laid down, the hole must be covered with another piece of draping material or the entire drape is discarded. 13. A hair found in a drape must be removed, and the area must be covered immediately. SUTURES Surgical sutures as defined by the United States Pharmacopeia are divided into two classifications: absorbable and non-absorbable. I. Absorbable sutures are sterile strands prepared from collagen derived from healthy mammals or from a synthetic polymer. They are capable of being absorbed by resistance to absorption. Types of absorbable sutures: 1. Surgical gut is collagen derived from submucosa of sheep intestine of the serosa of beef intestine. It is digested by body enzymes and absorbed by tissue thus no permanent foreign body remains. 2. Plain surgical gut is used to ligate small vessels and to suture subcutaneous fat. It losses tensile strength relatively quickly, usually in five to ten days and is digested within 70 days because collagen strands are not treated to resist absorption. 3. Chromic surgical gut is treated in a chromium salt solution to resist absorption by tissues for varying lengths of time depending on strength of the solution, duration and method of process. It is used for ligation of larger vessels and for suture of tissues in which nonabsorbable materials are not usually recommended because they may act as nidus for stone formation, as in the urinary and biliary tracts. 4. Collagen sutures are extruded for a homogenous dispersion of pure collagen fibrils from tendons of beef. They are used primarily in ophthalmic surgery. 5. Synthetic absorbable polymers are used for ligating or suturing except in tissues where extended approximation of tissues under stress is required. Intraoperative Ng | 8 6. Polydioxanone is a monofilament suture extruded from the polyester and is particularly useful tissues where both an absorbable suture and extended would support are desirable. 7. Polyglycolic 9/0 are controlled combination of glycolide and lactide resulting in a copolymer with a molecular structure that maintains tensile strength longer than a surgical gut. These sutures are available in two forms: uncoated monofilament and coated multifilament. 8. Polyglycolic acid is a homopolymer which loses tensile strength more rapidly and absorbs within 30 days. It is braided suture material available in two forms: uncoated and coated. II. Non-absorbable sutures are strands of natural or synthetic material that effectively resist enzymatic digestion of absorption in living tissue. Types of non-absorbable sutures: 1. 2. 3. 4. 5. 6. 7. 8. Surgical silk is animal product made from the fiber spun by the silkworm larvae in making cocoons. It gives good support to wounds during ambulation and generally promotes wound healing a little more rapidly than surgical gut. Virgin silk suture consists of several natural silk filaments drawn together and twisted to form 8-0 and 9-0 strands for tissue approximation of delicate structures primarily in ophthalmic surgery. Surgical cotton suture is made from individual, long-staple cotton fibers that are combed, aligned and twisted into a smooth multifilament strand. Surgical linen is spun from long-staple, flax fibers, and then twisted into tight strands and thread from smooth passage through tissue. It is used almost exclusively in gastrointestinal surgery. Surgical stainless steel sutures are drawn from 316L-88(L for low carbon) iron alloy wire. It is used in surgical stainless steel implants and prostheses. Synthetic nonabsorbable sutures are used to replace silk because they have higher tensile strength and elicit less tissue reaction. Surgical nylon is a polymide polymer derived by chemical synthesis from coal, air and water. Polymer fiber is a polymer of terephthalic acid and polyethylene such as silicone, mersilene, person and others. Polypropylene is a long-chain plastic polymer extruded into a blue dyed monofilament suture strand. This is an acceptable substitute for stainless steel in situations where strength and reactivity are required and the suture must be left in place for prolonged healing. SURGICAL NEEDLES A. Point of Needles: 1. Cutting point – a razor-sharp hand cutting point may be preferred when tissue is difficult to penetrate such as skin, tender and tough tissues or eye. 2. Conventional cutting tissues – two opposing cutting edges form a triangular configuration with a third edge on the body of the needles. 3. Reverse cutting needles – a triangular configuration extends along the body of the needle. 4. Side cutting needles – relatively flat on top and bottom angulated cutting edges on the sides. 5. Taper points – these needles are used in soft tissues, such as intestines and peritoneum, which offer a small amount of resistance to the needle as it passes through. B. Body of Needles: The body of shaft varies in wide gauge, length, shape and finish. The nature and location of the tissue to be sutured influence selection of needles with variable features. 1. Tough or fibrous tissue requires a heavier gauge needle than the fine gauge wire needed in microsurgery. 2. Depth of bite through tissue determines appropriate length. 3. Body may be round, oval, flat or triangular. 4. Curve needles that have longitudinal ribbed depressive or grooves along the body inside and outside curvatures create a cross-looking action of the needle in the needle holder. 5. Body of all needles must have smooth finish. C. Eye of Needle: 1. Eyed needle – the closed eye of an eyed surgical needle is like that of any household sewing needle. Shape of the enclosed needle may be found oblong, or square. 2. Eyeless needle – is continuous unit with the suture strand. The needle is swigged onto the end of strand in the manufacturing process. Types of Eyeless Needle-suture Attachments: a. Single-armed attachments have one needle swigged to the suture strand. b. Double-armed attachments have one needle swigged to each end of the suture strand. c. Permanently swigged needle attachment is secure so that the needle will not separate from the needle inadvertently but does not released when pulled off intentionally. DOCUMENTING Documentation by a circulator of direct intraoperative patient care: 1. Initial assessment of the patient on arrival to the OR. The identity of the patient and verification procedure should be validated. 2. The significant times, such as arrival, start, completion, and room exit. 3. Disposition of the sensory aids or prosthetic devices accompanying the patient on arrival in the OR. Intraoperative Ng | 9 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. Placement of monitoring and electrosurgical unit (ESU) electrodes, tourniquets, and other special equipment and identification of units or machines used as applicable, the setting and duration of use should be recorded. The names and titles of all personnel in the room for the procedure. The type of anesthetic used and by whom. The surgical site preparation, the antiseptic agent administered and by whom. Medications, solutions and doses administered and by whom. A description of the actual surgical procedure performed. Contact with the patient’s family or SO. Type, size and manufacturer’s identifying information (Lot No.) of prosthetic implants, or the type, source, and location of tissue transplants o inserted radioactive materials. Use of X-ray study or imaging. Disposing of tissue specimens and cultures. Correctness or incorrectness of surgical counts (if incorrect, the remedial measures taken to locate the lost item) Placements of drains, catheters, dressings, and packing. Output is recorded if receptacle is emptied in the OR. Wound classification. Charges the patient for supplies according to hospital routine. Piece of equipment sent from OR with pt. to the unit. Disposition of the pt. after leaving the OR. Any unusual events or complication. POTENTIAL INTRAOP COMPLICATIONS A. Nausea and Vomiting B. Hypoxia and Respiratory problems C. Hypothermia D. Malignant Hyperthermia INTRAOPERATIVE NURSING CARE MANAGEMENT I. ASSESSMENT 1. Identifying the surgical client 2. Assess the emotional and Physical status 3. Verify information in the Preoperative checklist II. ANALYSIS III. PLANNING & IMPLEMENTATION Caring for the Patient During Surgery: (a) Reducing Anxiety (b) Protecting patient’s safety (c) Preventing intraoperative positioning injury (d) Serving as patient advocate IV. EVALUATION TRANSFERRING PATIENT TO THE PACU - - Transport from OR to PACU, anesthesia provider remains at the head of the stretcher (to maintain pt’s airway) and a surgical team member remains at the opposite end. Transporting the patient involves special considerations of the patient’s incision site, potential vascular changes, and exposure. Pt. is positioned so that he/she is not lying on or obstructing drains or drainage tubes. Serious arterial hypotension may occur if the patient is moved from 1 position to another, such as from lithotomy to horizontal position, or from lateral to supine position. Therefore patient must be moved slowly and carefully As soon as the pt. is placed on the stretcher or bed, the soiled gown is removed and replaced with a dry gown. Pt. is covered with lightweight blankets and warmed. Side rails are raised. The nurse who admits the pt. to the PACU reviews the ff. information with the anesthesiologist/anesthetist. Med. Dx and the type of surgery performed. Pt’s age and general condition, airway patency and v/s. Anesthetic and other medications used ( opioids and other analgesics, muscle relaxants, antibiotics, etc.) Any problems that occurred in the OR that might influence postop care ( hemorrhage, Cardiac arrest, shock) Pathology encountered ( if malignancy, whether the pt. or family has been informed) Fluid administered, estimated blood loss and replacement. Any tubing’s, drains, catheters, or other supportive aids. Specific info about which the surgeon/ anesthesiologist wish to be notified. Intraoperative Ng | 10