histo 17 [3-20
advertisement

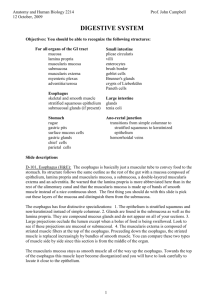
Chapter 17 GI doodles and stuff 1. What contributes to a selectively permeable barrier in the stomach and intestines? Tight junctions between simple columnar epithelial cells of the mucosa 2. What intestinal feature provides additional surface area (beyond microvilli) and contains digestive enzymes? glycocalyx 3. 4. Where are Peyer’s patches located? Mucosa of ileum Where is Meissner’s plexus? Auerbach’s plexus? What cell bodies are located here? = submucosal plexus = myenteric plexus; in the muscularis externa; contains postganglionic parasympathetic cell bodies 5. Name the layers of tissue, starting in the lumen: Mucosa i. epithelium ii. lamina propria iii. muscularis mucosae Submucosa i. Meissner’s / submucosal Muscularis externa i. Auerbach’s / myenteric Serosa 6. How is stomach musculature different? Muscularis externa contins oblique layer of muscle What is the main cell type of the serosa? Mesothelium: simple squamous epithelium 7. 8. What are the two kinds of glands in the esophagus, and where are they located? Esophageal glands proper; tubuloalveolar glands mostly in upper half Esophageal cardiac glands; in terminal and beginning portion i. Neutral secretions to protect from stomach acid 9. What epithelium lines the gastric pits? Simple columnar “surface mucous cells” 10. Which cells secrete acid? Which secrete intrinsic factor? Parietal cells Also parietal cells 11. What can happen with long term use of H2 receptor antagonists? Something about h pylori cross reaction??? Pernicious anemia, because they inhibit all functions of parietal cells 12. How is mucus different when it comes from gastric glands? Mucous neck cells secrete insoluble mucus when the stomach is active 13. How do chief and parietal cells stain? Basophillic Eosinophillic cytoplasm, spherical nucleus 14. How is acid excreted by parietal cells? Carbonic anhydrase produces H+ (and HCO3- which is put into the blood) H+/K+ ATPase pumps acid out and K+ in K+ and Cl- excreted by uniporters 15. What is the most common site for neuroendocrine (gastroenteropancreatic) tumors? What is a common syndrome they produce? What is a common paracrine hormone they produce? Appendix Carcinoid syndrome Somatostatin 16. What are the primary chemoreceptors in the stomach? Open enteroendocrine cells i. Clear cytoplasm 17. Which protective glands are tortuous? Coiled and branched? Cardiac Pyloric (located in the antrum [between fundus and pylorus]) 18. What enzyme kicks off digestion in the brush border? Enterokinase, which activates trypsin, which activates the rest 19. How are amino acids absorbed? Either as dipeptides or free amino acids; by Na+ dependent transporters In Hartnup disease, nonpolar AAs can’t be absorbed well 20. What provides vertical structure to enterocytes, and what does it connect to? Actin microfilaments Terminal web: horizontally oriented microfilaments, which attach to the zonula adherens 21. What happens when the terminal web contracts? Microvilli spread apart, increasing surface exposure 22. What mechanism is used by enterocytes to reabsorb water? What happens when lateral plications (lateral enterocyte surfaces) separate during absorption? Solvent drag The intercellular compartment is enlarged; hydrostatic suction increases flow into lamina propria 23. What do goblet cells do? Produce mucus; apex appears empty 24. What is the funciton of Paneth cells? Where are they found? How do they look (base and apex)? What do they contain? Secreting antimicrobial substances and phagocytosis of certain microbes Bases of intestinal glands (= crypts of Lieberkuhn) in the lamina propria Basophilic base, intensely acidophilic secretory vesicles Lysozyme, a-defensins, zinc, and other glycoproteins; can also phagocytose bacteria 25. What is the function of M/microfold cells? Pinocytose antigens from the apex and exocytose them out the base Cover the Peyer’s patches in the lamina propria 26. What are intermediate cells and where are they located? What do they look like? What determines the fate of differentiating cells? Stem cells in the lower intestinal glands Short irregular microvilli with long core filaments and tons of desmosomes Transcription factor Math1 27. What is the structure of sIgA? IgA dimer plus a chunk of the polymeric immunoglobulin receptor pIgR i. This “secretory component” gets clipped off with the IgA dimer at the apex 28. What’s another name for submucosal glands? What do they make? Brunner’s glands Most important for bicarb production, which neutralizes acid in the duodenum 29. How is colonic mucosa different? What is a caveolated “tuft” cell? No Paneth cells There an approximately equal number of goblet cells and absorptive cells near the rectum Putative exhausted goblet cell 30. What four features about the lamina propria are different in the colon? Collagen table to help regulate water and electrolyte transprot Pericryptal fibroblast sheath, thought to produce macrophages GALT is more developed Only a few tiny lymphatic vessels at the bases of intestinal glands 31. What’s special about the appendix? Lymphatic nodules everywhere Muscularis externa has a very thick circular layer and thin longitudinal layer 32. How can you tell if endoscopic removal of a polyp is enough? It’s fine as long as the polyp didn’t invade the mucosa 33. Two features of the upper anal canal? Columns and sinuses haha gross 34. Where do fistulas form? Through diffuse lymphatic tissue