5) If the Care Coordinator receives notification of a member's
advertisement

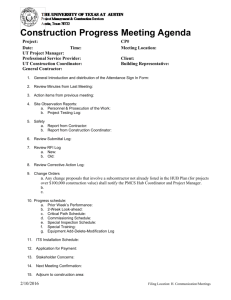
Care Coordination Delegation Guidelines for Community Members Secure Blue—MSHO (Minnesota Senior Health Options) 2012—September Updates Table of Contents RESOURCES …………………………..……………………………………………………….3 INTAKE PROCESS Delegate Responsibilities upon Notification of Enrollment ………………………………….…..4 Blue Plus Members living in a Veterans Administration Nursing Home (added Sept 2012)…….4 Contacting the Member and determining Health Risk Assessment (HRA) tasks (Updated January 2012)……………………………………...…………………………………...…….……5 CARE COORDINATION ASSESSMENT AND CARE PLAN RESPONSIBILITIES Contact Requirements—Member ………………..……………………………….………………6 Contact Requirements—Physician (Updated January 2012)……………………………………...6 Health Risk Assessment for members with an HRA not done within 12 months (Updated January 2012)……………………………………………………………………………...………6 Health Risk Assessment for members with an HRA done within 12 months……………...…..…6 Health Risk Assessment for members on Disability Waivers or residing in an ICF/DD facility or DD member living in the community (Updated January 2012 & Sept updates in purple)…… 7 In-Home Assessment (Updated January 2012 & Sept updates in purple)………………….……..8 Entry of LTC Screening document (Updated January 2012).………………………...….…….....8 Comprehensive Care Plan (Updated January 2012)……………………………………….….…11 Consumer Directed Community Supports (CDCS) (Added September 2012)………….…...….11 Authorization of Home Care Services (Updated January 2012) ………… ……………...….….12 PCA Assessment Process (Updated January 2012)……...…………………………………..….14 Customized Living Process (Updated January 2012)……….………….…………………..…...16 EW Authorization, Service Agreements and Claims Processing (Updated January 2012) (April 2012 updates in blue)……………………………………………………………….…....17 Reassessment Requirements (Updated January 2012)………………………………….…….....20 Reassessment LTC Screening Document entry (Updated January 2012)…………………….....21 ON-GOING CARE COORDINATION RESPONSIBILITIES Primary Care Clinic Change ………………………………………………………..……...……21 Transitions of Care (Updated January 2012 & Sept updates in purple)………..……………..…22 Transfers of Care Coordination to another Delegate (Updated January 2012 & Sept updates in purple)…...…………………………………………………………………….…………...…23 Transfers of Care Coordination within same agency (Updated January 2012 & Sept updates in purple)………….................................................................................................................…..25 Case Closure Care Coordination Responsibilities…...…………………………………….….…25 Special Status/Notification of Change Needed……………………………………………..……25 Coordination of Potential Denials, Terminations, and Reduction of Services……………...…...26 Grievances/Complaint Policy and Procedure ……………………………………………..….....26 EW Conversion/Request to Exceed case mix cap (Updated January 2012)(April 2012 updates in blue).................................................................................................................................…….28 Interpreter Services (Added September 2012)………………………………………………..…30 Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 1 (Table of Contents continued on Page 2) OTHER CARE COORDINATION RESPONSIBILITIES PIPs, Fraud, Waste and Abuse Training, general Care Coordination documentation, member rights, coordinating with local agency case managers (Updated January 2012)…………...……30 Network Providers (Elderly Waiver and Blue Plus Network)……………………………..…….31 Out of Country Care (new for 2012)……………………………………………………………..31 Audit Process………………………………………………………………………….…………32 Records Retention Policy (April 2012 updates in blue)……………………..………....…..……32 Care Coordination Services Overview………………………………………………………...…32 Care Plan Service and Guidelines………………………………………………………………..33 Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 2 These guidelines and all forms, letters and resources are available to our Care Coordination Delegates at: www.bluecrossmn.com/carecoordination For Home Care/PCA Authorization questions contact: IHM Intake/Support at: 1-800-711-9868 or 651-662-5540 Fax: 651-662-6054 or 866-800-1665 Enrollment questions contact: SecureBlue_enrollment@bluecrossmn.com For Other Member-Specific issues contact: Clinical Guide Resource Team at: 1-866-518-8447 or Clinical_Guide_Resource_Team@bluecrossmn.com For EW Claims Processing and Service Agreement questions contact Bridgeview Company (formerly First Solutions): www.bridgeviewcompany.com 1-800-584-9488 Or e-mail: Serviceagreements@bridgeviewco.com EWProviders@bridgeviewco.com General Process questions contact Government Programs Partner Relations Team: Melody Bialke, Manager 651-662-6420 1-888-878-0139 ext. 26420 Kathy Everson 651-662-7424 1-888-878-0139 ext. 27424 Kim Flom-Brooks 651-662-9647 1-888-878-0139 ext. 29647 Karla Kosel 651-662-4166 1-888-878-0139 ext. 24166 Katie Gumtow 651-662-2297 1-888-878-0139 ext. 22297 Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 3 Definitions: Care Coordination is defined as the assignment of an individual who coordinates the provision of all Medicare and Medicaid health and long-term care services for MSHO enrollees, and who coordinates services to an MSHO enrollee among different health and social service professionals and across settings of care. Delegate is defined as the agency, such as counties, private agencies and clinics, that are contracted to provide Care Coordination services for Blue Plus. Required Caseload per worker for Community Well, Nursing Facility, and Elderly Waiver is as follows: Elderly Waiver/Community Well mix = 50-80, Nursing Facility only = 100-130, and Community Well only = 100-125. INTAKE PROCESS Delegate Responsibilities upon Notification of Enrollment—Blue Plus is notified by Department of Human Services (DHS) twice a month via enrollment tape then notifies the Delegate via secure e-mail. Upon notification the Delegate: 1. Assigns a Care Coordinator per Delegate’s policy 2. Informs the member of the name, number, and availability of the Care Coordinator within 10 days of notification of enrollment 3. Notifies BluePlus’ Integrated Health Management-Government Programs (IHM-GP) of the Care Coordinator assigned using form 6.07 Notification of Care Coordinator Assigned. 4. Documents any delays of enrollment notification in case notes 5. Uses the following optional checklist: 6.12 CW EW Checklist SB 6. The Delegate is responsible to verify member’s eligibility prior to delivering Care Coordination services. Blue Plus members living in a Veteran Administration Home (Nursing Home) (Added September 2012) For MSHO members living in a Veteran’s Administration Nursing Home, the care coordinator should follow the processes and timelines outlined in the Care Coordination Guidelines for Members in the Nursing Home. Note: Please be aware that these members are designated by DHS as a Rate Cell A (Community Well) and thus will show up as a Rate Cell A on your enrollment reports. In other words, they will not show up on your enrollment lists as a Rate Cell D like other members in the nursing home. The Delegate should be aware of this and proceed as they would other Rate Cell D nursing home members. Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 4 Contacting the Member and determining Health Risk Assessment (HRA) tasks 1. Welcome call/letter (8.22 Intro Letter) to member within 30 days after notification of enrollment 2. Explanation of Care Coordinator’s role. Optional resource: 6.01 Welcome Call Talking Points. 3. Explanation of Additional 2 Routine Podiatry Visits and Safety Benefit discussed with member using the resource 6.26 Explanation of Additional Benefits for 2012. Additional Safety Benefit should be used as a last resort payer, after Medicare, MA, EW and any other third party payer. 4. Per DHS requirements, a Health Risk Assessment must be completed for all members within 30 calendar days of notification of enrollment. The Care Coordinator will make a determination about whether an on-site HRA is needed, and, if so, schedules the meeting and uses the DHS assessment tool, Long Term Care Consultation (LTCC). See pages 4 and 5 for Health Risk Assessment requirements. An on-site HRA LTCC should be done for members who: Have not had an LTCC within 12 months of enrollment. Have had an LTCC completed within 12 months of enrollment but are experiencing a signification change. Have no current EW services and requests an LTCC. This assessment should be completed within 15 calendar days of the request using the LTCC form and criteria. A Transitional Health Risk Assessment can be used for situations where an on-site HRA is not applicable (See page 6). HRA requirements for members on other waivers (CAC, CADI, DD, BI) and Members in an ICF\DD or DD case managed (See page 7). 5. Discuss In-Home Assessment Program. (See page 8 for details on this program) 6. Confirm the correct Primary Care Clinic (PCC). The PCC is listed on the enrollment list received from Blue Plus. A PCC may have been chosen by the member or auto-assigned if one was not indicated at the time of enrollment. A member, family member, or Care Coordinator may request the change by contacting member services at 651-662-6013 or 888-740-6013. The requestor must provide the member’s name, Blue Plus identification number, name of new PCC clinic, clinic location (town), and effective date. The effective date must be on the first of a month. If this PCC change will create a change in Care Coordination delegate for the member, the process for Transfers of Care Coordination to Another Delegate, as outlined on page 18, must be followed. Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 5 CARE COORDINATION ASSESSMENT AND CARE PLAN RESPONSIBILITIES Contact Requirements—Member 1. Community Well—One face-to-face visit & one 6 month phone contact, at minimum, per year 2. Elderly Waiver—Two face-to-face visits per year at minimum 3. As needed per significant change in member’s health status Contact Requirements—Physician. The Care Coordinator must communicate with the member’s primary care physician: 1. Within 90 days of enrollment the Care Coordinator shall mail 8.28 Intro to Doctor Letter even if unable to contact the member. 2. Annually, the Care Coordinator will complete and mail 8.29 Care Plan Summary Letter to Doctor or send a copy of the care plan. 3. As needed for Transitions of Care (See page 22), assessment, and care planning Health Risk Assessment for newly enrolled members who have not had an LTCC within twelve months from date of enrollment. (For members on other disability waivers, in an ICF/DD or DD member living in the community without DD waivered services, see section on Page 5) 1. The Care Coordinator will thoroughly complete all sections of the Minnesota Long Term Care Consultation Services Assessment Form (LTCC) [DHS-3428] (also Form 6.25 on the web-portal) within 30 days of receiving notification of a member’s enrollment. 2. Include Falls Risk Assessment. If the member is determined to be at risk of falls based on the LTCC assessment outcome (answering yes to any of the 3 falls risk questions), the Care Coordinator will make a referral for a home Physical Therapy (PT) evaluation. The PT may provide education or other support based upon the results of the assessment. 3. Include a discussion regarding the In-Home Assessment Program (see page 8) 4. Document any delays in scheduling of the assessment Health Risk Assessment for newly enrolled members who have had an LTCC within twelve months of enrollment and who have not experienced a significant change. 1. The Care Coordinator is still responsible for completing a HRA within 30 days of notification of enrollment. The Care Coordinator can meet this requirement without conducting a new LTCC by reviewing the current LTCC and care plan/community support plan/collaborative care plan from the member’s previous Health Plan or county. 2. The Care Coordinator should review the LTCC and care plan with the member, either telephonically or in person, to ensure that the assessment information hasn’t change and that the care plan is addressing the member’s needs. 3. The Care Coordinator documents these activities by completing the 6.28 Transitional Health Risk Assessment Form. Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 6 4. Include a discussion regarding the In-Home Assessment Program (see page 8). Health Risk Assessment and care planning for members on Disability Waivers such as Developmental Disabilities, Brain Injury, or Community Alternatives for Disabled Individuals (DD, BI, CAC or CADI) or are living in an ICF/DD or a DD member living in the community (September 2012 updates in purple). These members already benefit from intensive case management by the HCBS waiver case manager or the DD case manager for a member on the DD Waiver, in the community without DD waivered service, or in an ICF/DD. While the SecureBlue (MSHO) Care Coordinator can provide additional support, the primary case management responsibility will remain with the HCBS waiver case manager or the DD case manager for a member in an ICF/DD. All MSHO/MSC+ Care Coordination responsibilities such as contacts with member and physician, health risk assessments, care planning, and all other responsibilities and timeframes outlined in the Care Coordination Guidelines continue to be required. However, to avoid duplication with the case manager, the CC may complete some of the health risk assessment and care planning requirements in conjunction with the case manager’s current assessments and care plans, if available, and if completed within the past 12 months. Thus, the Care Coordinator can review the current assessment and plan of care following the process below. Note: If there is no other assessment and care plan available to review, or the other assessment and care plan is older than 12 months, then an LTCC and Collaborative Care Plan must be done within 30 days of notification of enrollment. 1. Health Risk Assessment— The Care Coordinator is responsible for completing a Health Risk Assessment within 30 days of notification of enrollment. The Care Coordinator can meet the HRA requirement by reviewing the member’s current assessment and care plan and completing the 6.17 ICF/DD and HCBS Disability Waiver Health Risk Assessment and Care Plan Supplement. A copy of the current assessment and care plan reviewed should be placed in the member’s MSHO case file. 2. Care Plan— Health related goals must be entered onto this form. Preventive care should be discussed and documented. The Care Coordinator must sign and date and send a copy to the other Case Manager (if different than the Care Coordinator) and a care plan summary should be sent to the physician. 3. The Care Coordinator should never enter a Screening Document in MMIS. This task is completed by the disability case manager only. 4. Be sure to document your attempts to obtain the assessment and care plan documentation from the other case manager and document any delays in completing your HRA and care planning requirements in your case notes. Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 7 5. Include a discussion regarding the In-home Assessment (formerly MedAssurant) Program (see below). In-Home Assessment Program (Administered for Blue Plus by Inovalon formerly known as MedAssurant) (Excludes Essentia and North Clinics) September 2012 updates in purple. During the Health Risk Assessment the Care Coordinator will introduce the In-Home Assessment program and give the member a copy of an informational flyer, form 6.30 InHome Assessment Program—Member Information. This program has two components: 1. In-Home Assessment. All newly enrolled MSHO members shall be offered a noninvasive in-home assessment by a Nurse Practitioner or Physician from Univita, a new sub-contracted agency replacing Inspiris, contracted with Inovalon. Care Coordinators will explain who Inovalon and Univita are and inform the member of the phone call they will receive offering a non-invasive in-home assessment. The purpose of the assessment is to insure the member’s health care needs are identified early and this information is shared with the member’s primary care physician. Inovalon staff will call newly enrolled members no sooner than 45 days of enrollment to schedule the in-home assessment. A copy of the 3-4 page assessment results will be left with the member and sent to the primary care physician. For questions, the member, or the Care Coordinator on the member’s behalf, can contact Inovalon at 866-359-1626 2. Throughout the year, MSHO members will be identified, according to Blue Plus claims data, with what appears to be undocumented chronic conditions and follow up with either: A letter encouraging members to visit their primary care physician with a corresponding letter to their primary care physician identifying the conditions, or A letter and a phone call encouraging the member to visit their primary care physician with a corresponding letter to their primary care physician identifying the conditions, or An offer of an in-home non-invasive assessment by a Nurse Practitioner or a Physician from Univita, an agency contracted with Inovalon. A copy of the results of the assessment are left with the member and sent to the primary care physician for follow-up as deemed necessary by primary care physician. Entry of LTC Screening Document information into MMIS If no Screening Document in MMIS, then enter full LTC Screening Document into MMIS by cut-off dates listed below. MSHO-CW Screening Documents must be entered within 45 days of enrollment date. CW-members who cannot be found or refuse to have an assessment should have a SD entry using the Refusal code in MMIS. EW Screening Documents (SD) must be entered by the cut-off dates listed below: Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 8 When the First Month of the Eligibility Span is: January February March April May June July August September October November December January 2012 Last Day to Enter Screening Document timely is: 12/19/11 1/19/12 2/16/12 3/20/12 4/18/12 5/20/12 6/19/12 7/19/12 8/21/12 9/18/12 10/21/12 11/18/12 12/18/12 The delegate is responsible for updating LTC Screening Documents into MMIS for either Community Nursing Home Certifiable (EW) or Community Well (CW) populations when the member: moves from another Health Plan to Blue Plus switches products within Blue Plus (i.e., MSC+ to SecureBlue (MSHO)) moves from FFS to Blue Plus The care coordinator must also update the Screening document when there is a change in care coordinator. Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 9 The table below outlines what information should be updated: INSTRUCTIONS for MMIS ENTRY Move from FFS or another health plan to Blue Plus or switch of Blue Plus product Community Non-EW Move from FFS or another health plan to Blue Plus or switch of Blue Plus product Nursing Home Certifiable EW Transfer of Care Coordination Only Transfer of Care Coordination Only Community Non-EW Nursing Home Certifiable EW 02 05 02 05 Activity Date: Date Transitional HRA is completed LTCC Site: Change to BHP Date Transitional HRA is completed Change to BHP Date delegate assumed Care Coordination responsibility n/a Date delegate assumed Care Coordination responsibility n/a Case Managers Name and UMPI Number Use your MCO UMPI number Use your MCO UMPI number Use your MCO UMPI number Use your MCO UMPI number Assessment Result: 03 - remain in community without waiver services 98 - other 03 - remain in community without waiver services 98 - other Effective Date: Date of HRA is completed (the SD does not reset the ReAssessment date) Date of HRA is completed (this will not effect the elig span when using Activity type 05) Date delegate assumed Care Coordination responsibility (the SD does not reset the ReAssessment date) Date delegate assumed Care Coordination responsibility (this will not effect the elig span when using Activity type 05) LTCC Screening Document Fields Activity Type: Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 10 *Refer to the Screening Document manual for complete detailed information. Comprehensive Care Plan—Care Coordinators shall develop a comprehensive care plan in collaboration with the member, caregiver, and/or other interested persons, as appropriate within 30 days of the LTCC assessment using 6.02.01 Collaborative Care Plan. (For members on other disability waivers, in an ICF/DD or DD member living in the community, see section on Page 5) Instructions for the Collaborative Care Plan are available as form 6.02.02. The Care Plan must include: 1. Case mix/caps 2. Collaborative input 3. Assessed needs 4. Member requested services 5. Formal and informal supports 6. Person-centered goals, target dates, on-going monitoring 7. Preventive focused 8. Emergency back-up plans 9. Risk plan for services refused 10. Health Management discussion. BluePlus offers telephonic programs to address members’ current health concerns. Members or their caregivers have access to a dedicated clinician to receive education and support for their health concerns. Dedicated Clinicians are available to provide disease management services for members with asthma, coronary artery disease, congestive heart failure, or diabetes. Dedicated Clinicians may also provide short-term case management services in complex situations involving catastrophic illness/injury due to accident, high cost medical situations, frequent hospitalizations, out-of-state providers, or when additional education or support is requested by a member’s caregiver. Refer to these programs using 6.09 Health Management Referral form. 11. Advanced Directives discussions. The care coordinator can also use the resource 9.19 BCBSMN Advance Directive 12. Care Coordinators can consult with Blue Plus Health Plan resources if needed 13. Educate and communicate to enrollee about good health care practices and behaviors which prevent putting their health at risk. Important: The member must sign the Collaborative Care Plan. A copy of the care plan, including the budget worksheet and the Member Bill of Rights, Form 6.02.03, must be given to the member. Consumer Directed Community Supports (CDCS) (Added September 2012) CDCS is a service option available under the Elderly Waiver which gives members more flexibility and responsibility for directing their services and supports including hiring and managing direct care staff. Refer to the Department of Human Services website (http://mn.gov/dhs) for additional information regarding CDCS. Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 11 Choosing CDCS does not change the Care Coordinator’s responsibilities under the health plan. The Care Coordinator remains responsible for the completion of the Health Risk Assessment (LTCC) and collaborative care plan within the required timeframes. The collaborative care plan should coordinate with the community support plan created by the member or their representative. The Bridgeview Service Agreement web-tool contains two fields specific to CDCS: CDCS Eligible and CDCS Monthly Amount. Please refer to the web tool user guide for details regarding these fields and contact Bridgeview directly with questions. Authorization of Home Care Services Medicare billable skilled home care services do not require a review. The home care agency will determine whether the member qualifies for Medicare home care services. If Blue Plus is notified of Medicare eligible home care services, Blue Plus will advise the home care agency to contact the Care Coordinator to assure continuity of services. BluePlus will review Medical Assistance State Plan home care requests and determine the number of visits based upon medical necessity and state plan guidelines. Per statute, authorization is based upon medical necessity and cost-effectiveness when compared with other care options. Home care services include Skilled Nurse visits, Home Health Aide visits, Private Duty Nursing, Physical, Occupational, Respiratory, and Speech Therapy. This relates to all members receiving Medical Assistance home care services including those on a home and community based service waiver. If a member switches from Fee-For-Service or another health plan to Blue Plus, Blue Plus will honor the current authorization until the authorization end date or a new review occurs. Blue Plus reserves the right to review these requests for medical necessity. The member then will be reassessed at their normal assessment period following the process below. Reminder: For MSHO/SecureBlue, MSC+/Blue Advantage members on EW, extended home care services may be authorized by the Care Coordinator. To be eligible for extended home care services, the member must first be accessing home care under the medical benefits. If the medical benefits alone do not meet the member’s care needs, extended home care services may be authorized by the Care Coordinator. The Care Coordinator should assess for appropriateness of extended home care. The Care Coordinator may only review for the same services already authorized under the medical benefit (i.e., Home Health Aide is approved under the medical benefit, then the EW extended home care service must also be Home Health Aide. Blue Plus does not need to review these services as extended home care services under EW, are not subject to Medical Necessity guidelines. Notes related to billing of state plan and extended home care services: Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 12 Extended home care services and state plan home care services count towards CAP if member is on EW Extended home care services and state plan home care services need to be included on the Service Agreement to Bridgeview Company. Extended home care claims should be submitted to Bridgeview Company. State Plan home care claims should be submitted to Blue Plus The Care Coordinator shall follow the process outlined below and fax in home care requests prior to services starting using either of the following forms: For members who are on disability waivers such as CADI, CAC, BI, or DD use form 6.04.01 Recommendation for Auth of MA Home Care (DHS 5841-ENG 0611) For members on EW or Community Well members not on waivers listed above use form 6.04.03 MA Home Care Services Recommendation/Non-disability form 1. Prior to the services starting, or upon annual reassessment, the Care Coordinator will fax in the 6.04.01 Recommendation for Authorization of MA Home Care Services form for members open to a home and community based disability (after consulting with the disability waiver case manager) or the form 6.04.03 Home Care Services Recommendation-Non Disability to request BluePlus to review the services. Be sure to include a copy of the current authorization if previously on FFS or another Health Plan. Also, if member is residing in a Residential setting such as Customized Living Facility or Adult Foster Care, please include this information in the Summary section. If a member resides in Customized Living and you are requesting home care service, please fax a copy of the Individualized EW Customized Living Plan along with your request. 2. BluePlus will obtain necessary medical information from the home care agency including a medical records request. Sending in this documentation is the responsibility of the home care agency. Blue Plus may contact the care coordinator for additional information. 3. BluePlus will instruct home care agencies to contact the member’s Care Coordinator for consultation regarding the member’s plan of care and to assure services fit under CAP. 4. BluePlus will review the information submitted and make a coverage determination within 10 calendar days of receipt of the request. Requests are reviewed based on the individual’s medical needs and therefore the number of visits and date span authorized may vary. 5. Blue Plus understands that, at times, a member may require an immediate evaluation due to a significant change in medical condition; thus Blue Plus would never deny an evaluation. 6. For an acute change in a member’s medical condition, where the services requested are not Medicare eligible, the care coordinator should fax in the request form as soon as they Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 13 are aware of the home care needs. Up to ten visits of skilled home care services such as PT/OT/ST, RN, or Home Health Aide will be approved immediately to assure patient medical needs are met. Note: For members with chronic conditions, the care coordinator need only fax in one request. Blue Plus may approve 2-3 months at a time. It is the responsibility of the home care agency to send in supporting documentation when the authorization comes to an end. Blue Plus will keep the Care Coordinator informed with each subsequent authorization for management of cap. Care Coordinators do need to fax in the home care request with each annual assessment. 7. After a determination is made, BluePlus will notify the member and the home care provider of the outcome via a letter. 8. Blue Plus will fax the determination back to the Care Coordinator for their records, EW case mix cap management, and disability waiver budget management. The Care Coordinator must communicate with the other waivered case manager, if any. 9. Denials, Terminations or Reduction (DTR) of MA State Plan Home Care services will be processed by Blue Plus for home care denials, reductions or terminations. Note: Fluctuations in a member’s plan of care is not a DTR. See page 26 for detailed instructions on the process for Potential Denial Termination Reduction of Services that are initiated by the Care Coordinator. PCA Authorization Process Blue Plus will review all PCA requests for medical necessity. A member is entitled to up to two PCA evaluations per year. Care Coordinators should contact Blue Plus if additional evaluations are needed. All Secure Blue (MSHO) and MSC+ members receiving or requesting PCA services will be required to be assessed using the DHS tool, Personal Care Assistance (PCA) Assessment and Service Plan (DHS-3244-ENG), or if on any HCBS Waiver, use the DHS tool Supplemental Waiver Personal Care Assistance (PCA) Assessment and Service Plan (DHS-3428D-ENG). Blue Plus will review all PCA requests to determine the number of units the member is eligible for under state plan services. Assessors may be a Care Coordinator or a PHN but they must attend DHS training before qualifying to perform PCA assessments. 1. Upon completion of the PCA assessment, the assessor (PHN or Care Coordinator) is responsible for providing a copy of the Completed PCA Assessment and Service Plan to the member and PCA provider within 10 days. Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 14 2. The assessor must also fax the PCA assessment, prior to services starting, to Blue Plus for a coverage determination and authorization at 866-800-1665 or 651-6624022. Note: Blue Plus will not accept LTCC Assessment tool for determination of PCA services 3. If Blue Plus has questions regarding an assessment, we may contact the Care Coordinator or the PHN assessor to discuss. 4. As a reminder, reduction or termination in services requires a 30 day notice. 5. BluePlus will send any letters (approval or denial) to the member and agency via mail and the care coordinator via fax. Requests for PCA Temporary starts or increases: All temporary PCA starts or temporary increases may be approved on an as needed basis. The Care Coordinator should complete section, PCA Temporary Start/Temporary Increase, on the form 6.04.03 MA Home Care Services Recommendation-Non Disability and fax it to BluePlus for entry. PCA temporary starts and temporary increases are only valid for up to 45 days and must include the reason for the temporary start/increase. On-going PCA Services: If services are reduced, the current authorization will be extended to accommodate the 30 day notification period. A new authorization will be entered for services beyond the 30 days with the new number of units approved. If services are an increase, the increase will start the day of the BluePlus determination. If the Care Coordinator is requesting a future start date, please indicate the start date on your request (see first case example below). Case Examples: Mildred, a MSHO/SecureBlue member is currently receiving 3 hours per day. The new PCA assessment indicated that the member now qualifies for 4 hours per day. Her current authorization does not expire until 1/31/12. The member’s waiver date span does not end until 1/31/12 and the member does not have room in her CAP for an increase until that time. Blue Plus received the PCA assessment and makes a determination that the increased hours are appropriate. The decision is made on 12/4/11. The new authorization for 4 hours per day will start on 2/1/12. Henry, a MSHO/SecureBlue member is currently receiving 4 hours per day. At his annual assessment the PCA assessment indicates that he only qualifies for 2 Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 15 hours per day now. His current authorization was up on 12/31/10. BluePlus receives the PCA assessment and makes a determination to decrease the hours to 2 hours per day. The decision is made on 12/30/10. Henry’s current authorization for 4 hours per day will be extended until 1/29/11 to accommodate the 30 day notification period. A new authorization is entered for 2 hours per day effective 1/30/11 through 12/31/11. Extended PCA Requests for members on EW: For MSHO/SecureBlue and MSC+/Blue Advantage members on EW, extended PCA hours may be authorized by the Care Coordinator. Extended PCA services cannot be a “stand-alone” PCA service. To be eligible for extended PCA, the member must first be accessing PCA services under the medical benefits. If the medical benefits alone do not meet the member’s care needs, extended PCA services may be authorized by the Care Coordinator. The Care Coordinator should assess for appropriateness of extended PCA. Blue Plus does not need to review as extended PCA is not based on medical necessity criteria. Notes related to billing of state plan and extended PCA services: Extended PCA services and state plan PCA services count towards CAP if member is on EW Extended PCA services and state plan PCA services need to be included on the Service Agreement to First Solutions. Extended PCA claims should be submitted to First Solutions. State Plan PCA claims should be submitted to Blue Plus PCA Reassessment—Per DHS, the PCA assessment is valid for 12 months from the assessment date. Statute for reference: 256B.0659, subd.3(a) and 4. Customized Living Process Blue Plus uses the approved DHS EW Customized Living Tool Kit which is available for download from the DHS website at: http://www.dhs.state.mn.us/dhs16_143983. Care Coordinators authorizing Customized Living Services need to complete the full tool kit which includes four separate documents. Upon completion, the entire tool kit is to be submitted to DHS through the use of MNITS. If you have questions please refer to the “Instructions for Use of the Customized Living Tools- Individual Care Plan,” which can also be found at the DHS website. For recent changes to the CL Tool or process updates, please refer to the EW Customized Living Tool Newsletter that is sent out to Care Coordinators from DHS. The Care Coordinator will assist members who are moving to a registered Housing with Services establishment to obtain or recover a verification code from the Senior Linkage Line. Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 16 Note: Please follow the new Customized Living standards per DHS Bulletins and 8/19/11 Communiqué. Elderly Waiver Authorizations, Service Agreements and Claims Processing Bridgeview Company (formerly FirstSolutions), a third party administrator, processes most Elderly Waiver provider claims and Service Agreements for MSHO/SecureBlue and MSC+/Blue Advantage. When authorizing an EW service, the Care Coordinator is expected to be compliant with all EW program rules, follow all appropriate bulletins related to MSHO/EW, and follow directions found in the Provider Manual Chapter 26A: Elderly Waiver and Alternative Care. Care Coordinators will submit Service Agreements directly to Bridgeview Company through their web-based tool and are responsible to become familiar with this web-tool and its accompanying manual. Care Coordinators are also responsible for EW Provider inquiries related to their Service Agreement entries. Extended home care services are to be authorized through the Bridgeview Company web tool with the appropriate HCPCS service code. These services are billed to Bridgeview Company. State Plan Home Care Services, Care Coordination and other services included in Case Mix Cap but Billed to Blue Plus Care Coordinators must calculate the monetary total of state plan home care services (X5609-PCA, HHA, SN, PDN), care coordination (T1016 UC, T1016 TF UC), adult day bath (S5100 TF), and CDCS case management (T2041) services that are being rendered to the member during the waiver span and are counted against the member’s monthly case mix service cap. This total amount must be placed in the Bridgeview Company web tool under the LTCC/Case Mix section. These services are not billed to Bridgeview Company; they are billed to BluePlus. Extended Supplies and Equipment (T2029) 1. To assist with the authorization the Care Coordinator shall use the resource Extended Supplies and Equipment (T2029) Grid. This tool is to be used as a resource for EW eligibility and/or proper first payer. This document is not all inclusive and will be updated regularly. It is available on the Bridgeview Company web site: www.bridgeviewcompany.com 2. If an item is listed on the Extended Supplies and Equipment resource as not Elderly Waiver Eligible, the Care Coordinator should not authorize it. If an item has not been included on the resource list and the Care Coordinator is uncertain if it meets the EW Service Criteria as outlined in the MHCP Manual, contact the Clinical Guide team at 1-866-518-8447 or Clinical_Guide_Resource_Team@bluecrossmn.com. Note: Telemonitoring is not an eligible service under EW. Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 17 When completing the Service Agreement, each Extended Supply and Equipment item authorized should be listed on a separate line with a narrative description of what is being authorized, the number of units, and the specific rate per unit. Inquiries related to EW claims and Service Agreements should be directed to Bridgeview Company: www.bridgeviewcompany.com 1-800-584-9488 Or e-mail: ServiceAgreements@bridgeviewco.com EWProviders@bridgeviewco.com Prior Authorization Process for Specialized Supplies and Equipment/Items over $500 and Exceptions to SSE/T2029 Guide (Updated April 2012) Both delegate Care Coordinators and Blue Plus Utilization Management (UM) now have a role in authorizing Specialized Supplies and Equipment for members on Elderly Waiver (EW). Coordination and communication is key. Delegate Care Coordinators—authorize EW Services Blue Plus UM—authorize: o SSE items over $500 o Exceptions to the SSE/T2029 Guide Process 1. To request a prior authorization for a SSE item over $500 or an Exception to items listed as ‘no’ for EW eligibility in the SSE/T2029 Guide, the Care Coordinator must fax all of the following to Blue Plus Utilization Review at 651-662-4022 or 1-866-800-1665: a. Completed 6.06 Elderly Waiver Prior Authorization Request form which should include: b. Extenuating circumstances that warrant an exception to the SSE/T2029 Guide. c. How the item will prevent institutional placement. d. Is the item the most cost effective alternative? e. Description of other alternatives that have been tried and failed or considered prior to this request. 2. Blue Plus will make a coverage determination within 10 business days and notify the Care Coordinator and Bridgeview Company via secure e-mail. a. The Care Coordinator is responsible to notify the member of the approval and document all approved services on the member’s service agreement and the budget worksheet. 3. DTR Appeal Notices Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 18 a. If the Over $500 or Exception requested item is denied, Blue Plus UM will issue a DTR to the member and e-mail a copy to the Care Coordinator. 4. Authorization entry a. The Delegate Care Coordinator will enter the authorized EW items in the Bridgeview Company service agreement web-tool. This would include: UM approved items over $500 Approved exceptions to the SSE/T2029 Guide Note: Do not enter a Service Agreement until the item has been approved. Prior Authorization Process for Lift Chair and Mechanism Both delegate Care Coordinators and Blue Plus Utilization Management (UM) now have a role in authorizing lift chairs for members on EW. Coordination and communication is key. Delegate Care Coordinators—authorize EW services Blue Plus UM authorizes o Lift mechanisms under member’s medical benefit (Medicaid/Medicare) o Prior authorize chairs paid for under EW over $500. Process 1. To request authorization for a lift chair, the Care Coordinator must fax the following to Blue Plus Utilization Review at 651-662-4022 or 1-866-800-1665: a. A completed 6.06 Elderly Waiver Prior Authorization Request form, b. the Specialized Supplies and Equipment Providers written quote the seperates out: the cost of the chair vs. the lift mechanism, and includes a description of any specialized chair features Note: Providers have been notified of the requirement for prior authorization of chair/seat lift mechanisms. 2. Blue Plus will make a coverage determination within 10 business days and notify the appropriate parties of the approval determination as follows: a. Motorized lift portion authorization under Medicare/Medicaid—notification will be sent to: The member Specialized Supply and Equipment/Durable Medical Equipment Provder Care Coordinator b. Chair portion over $500 authorization under EW—notification will be sent via secure e-mail to: Care Coordinator Bridgeview Company 3. DTR Appeal notices Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 19 a. If the lift portion is determined ineligible under Medicare/Medicaid Blue Plus UM will not send a DTR; the Care Coordinator will be authorizing the lift under the EW benefit. b. If the Over $500 chair is denied, Blue Plus UM will issue a DTR to the member and a copy the Care Coordinator. 4. Entry of Authorization a. Blue Plus UM will enter an authorization into the claims payment system for approved Medicare/Medicaid covered chair lift mechanisms. b. Delegate Care Coordinators will authorize EW covered items in the Bridgeview Company service agreement web-tool. This should include: Lift mechanisms not covered under Medicare/Medicaid Chair portions at or below $500 UM approved chair portions over $500 Note: Do not enter Service Agreements until an approval is received. Reassessments A reassessment must be completed within 12 months of the previous assessment for EW and CW members. The following steps are to be completed with each reassessment: 1. The Delegate is responsible to verify member’s eligibility prior to delivering Care Coordination services. 2. The Care Coordinator will thoroughly complete all sections of the Minnesota Long Term Care Consultation Services Assessment Form (LTCC) [DHS-3428] (also Form 6.25 on the web-portal). (For members on other disability waivers, in an ICF/DD or DD member living in the community, follow process outlined on Page 7) a. The same LTCC tool should be used for no more than three assessments. 3. The Care Coordinator shall complete the 6.02.01 Collaborative Care Plan within 30 days of the LTCC (refer to page 11). a. Document on-going monitoring of goals, interventions, and target dates b. The member must sign the Collaborative Care Plan. A copy of the care plan, including the budget worksheet and the Member Bill of Rights, Form 6.02.03, must be given to the member 4. The Care Coordinator will complete 8.29 Care Plan Summary Letter to Doctor or send a copy of the care plan. 5. If state plan home care services are needed, the Care Coordinator shall fax in the new request for authorization of home care services as outlined on page 12. Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 20 Entry of Reassessment LTC Screening Documents into MMIS by 4:30 of the cut-off date listed below. When the First Month of the Eligibility Span is: January February March April May June July August September October November December January 2013 Last Day to Enter Screening Document timely is: 12/19/11 1/19/12 2/16/12 3/20/12 4/18/12 5/20/12 6/19/12 7/19/12 8/21/12 9/18/12 10/21/12 11/18/12 12/18/12 Note: If a Community Well member refuses an annual assessment, a Screening Document should be entered in MMIS as a refusal. ON-GOING CARE COORDINATION RESPONSIBILITIES The Delegate is responsible for confirming member’s eligibility before providing Care Coordination Services Primary Care Clinic (PCC) Change When a member makes a permanent PCC change, Blue Plus must be notified so our systems are updated and the member can receive a Blue Plus identification card listing the name of their new PCC. A member, family member, or Care Coordinator may request the PCC change by contacting member services at 651-662-6013 or 888-740-6013. The requestor must provide the member’s name, Blue Plus identification number, name of new PCC clinic, clinic location (town), and effective date. The effective date must be on the first of a month. If this PCC change will create a change in Care Coordination delegate for the member, the process for Transfers of Care Coordination to Another Delegate, as outlined on page 23, must be followed. Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 21 Requesting a change to a member’s PCC is very important when a member moves to a nursing facility and their care coordination will be done by a new delegate. It is also vital to ensure physician communication is sent to the appropriate PCC. Transitions of Care (September 2012 updates in purple) 1. The Care Coordinator will provide transition of care services for members when they move from one care setting to another due to a change in health status. The goal of this process is to reduce incidents related to fragmented or unsafe care and to reduce readmissions for the same condition. Examples of transitions include: moving from their usual care setting to a hospital, skilled nursing facility, custodial nursing facility, regional treatment center or rehabilitation facility. Any movement between sites of care is a separate transition including the member’s transition back to his/her usual care setting. Follow up is required regardless of how or when the Care Coordinator learns of the transition. See 9.23 Transition Training Videoconference Q&A located on the web-portal for additional information. 2. The Care Coordinator will document transition services on the 6.22 Individual Care Transitions Log. Use 6.22.01 Individual Care Transitions Log Instructions for detailed information on the completions of the log. Use one log for each transition. The Individual Transition Log should be kept in the member’s file along with additional case note documentation as appropriate. 3. The Care Coordinator must document all care transition contacts in compliance with the following timelines: a. For planned transitions, contact the member prior to the admission day to ensure they have the Care Coordinator’s phone number and understand how the Care Coordinator will assist during the member’s care transitions b. Share essential information with the receiving facility (discharge planner, Social Worker, etc.) within 1 business day of learning of the admission. Examples of essential information include: services currently being received by the member and who provides them; the name of the Primary Care Provider/Specialty Care Provider to use as a resource for current medications, chronic conditions, and current treatments; the Care Coordinator contact information and a brief explanation of their role in assisting the member with care transitions. Work with the discharge planner to ensure continuity in home care, if needed, upon discharge. c. Notify the Primary Care Physician and/or Specialty Care Physician of all transitions including the transition to home, within 1 business day of learning of the transition, if they were not the admitting physician. Optional fax form: 6.22.2 Fax Notification of Care Transition is available for this communication d. Communicate with the member and/or member’s Rep within 1 business day of learning of the transition to explain your role and how to contact you during their stay and after they return home. Talk about what happened, changes in Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 22 health status, what might occur while in the hospital/nursing home, and any discharge plans leading to or delaying discharge. Communication with the Customized Living or Nursing Facility does not replace the requirement to contact the member/member’s representative. e. Reach out to the member after the return to their usual setting of care no later than 1 business days from notification to assess the member’s needs. Suggested topics to review: medication changes/new prescriptions filled, DME/supply needs, scheduling of follow-up appointments, transportation or other services needs, changes in functional needs (bathing, eating, dressing, transfers, etc.), and the member’s understanding of what to do if their condition worsens. f. Provide education to the member or the member’s authorized representative related to prevention of unplanned transitions and/or how to maintain their health and remain in the least restrictive setting. This education should be tailored to the member’s specific needs, diagnoses, health issues, etc. and should be in a format that best works for the member based on their abilities. Members with chronic conditions who are frequently hospitalized can still benefit from educational discussions about their conditions, appropriate care, treatment options and relationship building with the Care Coordinator. Members in a nursing facility can benefit from an opportunity to reinforce or develop what is in their nursing facility plan of care. Educational examples include (but are not limited to): Use of written materials related to a member’s medical condition. (These can be found in the Resource Management section of the Care Coordination web portal.) A referral to Disease Management A referral to Medication Therapy Management (Medicare recipients can receive this through a local pharmacy, or directly from a Blue Plus Pharmacist – see Key Contact List) Falls risk education Caregiver support/training Discussion with member (or authorized representative) during a nursing facility care conference Transfers of Care Coordination to Another Delegate Enrollment reports are distributed to delegates twice a month. The “Newly Enrolled” member enrollment report is sent via secure email the first week of each month. A “Full Detail” report is sent via secure email 3-5 days following the newly enrolled report. The Full Detail report contains all current members as well as newly reinstated members and termed members. Blue Plus relies on the financial worker to update the information timely and due to DHS's report cut off dates, there could be a delay of up to two months in the information showing up on our report. So, it is important, when a care coordinator becomes aware that a member has moved from their county, out of the Delegate’s service Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 23 area, the following shall be done to expedite communication to the new delegate and assist our members with smooth transfer of care coordination services and minimize any gaps in care: 1. The current Care Coordinator is required, at a minimum, to share assessment and plan of care information with the new delegated entity when the current Care Coordinator is made aware of a members move to another county, health plan, etc. 2. Be sure to communicate address changes to your county financial worker for timely updating of this information to the DHS tapes. 3. If the member is on EW, the current Care Coordinator shall keep the Waiver Span open in MMIS, as they remain eligible for EW. 4. The Care Coordinator must also notify the county financial worker and Blue Plus IHM-GP department when a member moves from their county by completing and faxing a 6.08 Notification of Member Change Needed form. This is the only way Blue Plus will be notified of the change and thus be able to communicate to the receiving Delegate in a timely manner. 5. The delegate must also notify Blue Plus when the transfer involves a move from the community to a nursing home for long term placement or from the nursing home back to the community and the case needs to be transferred to a Care Coordinator outside of the current agency. Notify Blue Plus using 6.08 Notification of Member Change form. 6. If a member enters an in-patient setting such as a hospital, Residential Treatment Center, etc. outside of the county the member resides in, the Care Coordination responsibility continues with the current Care Coordinator. Once it is determined the member will not be returning to the original county, the Care Coordinators should precede with the Transfer directions in #4 above. 7. Blue Plus will securely e-mail this form to the receiving Delegate as official notification that the new Delegate is now responsible to follow this member. 8. Receiving delegate has 10 days from the faxed date to assign a Care Coordinator and notify the member. The 8.30 CM Change Intro letter may be used to notify the member of a change in Care Coordinator. 9. The Care Coordinator will notify the physician using 8.28 Intro to Doctor Letter. 10. Keep copies of all forms and letters related to the transfer for your records 11. If no current Health Risk Assessment/Care Plan is received, the receiving Delegate must follow the process for completing the health risk assessment and care plan. 12. 9.01 Blue Plus Service Area Map 2012 can be used as a resource to determine if a move will take the member out of our service area. Implications of a move outside Blue Plus service area should be discussed with the member. Member questions related to selecting a new plan can be directed to Senior Linkage Line at 1-800-333-2433. Important: The current Care Coordinator is responsible for all care coordination activities until the case is formally transitioned. However, there may be tasks associated with the transfer that may make sense that one or the other completes and thus it is expected that the current and receiving Care Coordinators will work together throughout Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 24 the transition. Both Delegates can be reimbursed for their care coordination services during the overlapping time period. Transfers of Care Coordination within your agency If there is a change in Care Coordinator within the Delegate agency, the Care Coordinator must inform the member of the name, number, and availability of the Care Coordinator within 10 days of this change. The new Care Coordinator may use the 8.30 CM Change Intro letter for this purpose. The Delegate must also notify Blue Plus of the change by faxing the 6.07 Notification of Care Coordinator Assigned form. Case Closure Care Coordination Responsibilities 1. Please refer to the Bridgeview Company manual for requirements related to closure of current Service Agreements. 2. Inform the County Financial Worker of any permanent moves so that they may update their systems accordingly. 3. If a SecureBlue/MSHO member has Medicare and loses eligibility for Medical Assistance, Blue Plus will continue to provide Medicare-covered Plan benefits for up to three months. If after three months, the member has not regained Medical Assistance, coverage with Blue Plus will end. The member will need to choose a new Part D plan in order to continue getting coverage for Medicare covered drugs. If the member needs assistance, they can call the Senior Linkage Line at 1-866-333-2466. Care Coordination services continue to be provided during this three month period. 4. Determine the appropriate closing activity for the MSHO member by referring to DHS Instructions for Completing and Entering the LTC Screening Document into MMIS for MSHO/MSC+ Programs https://edocs.dhs.state.mn.us/lfserver/Public/DHS-4625-ENG. If the EW member is placed in a Nursing Facility for more than 30 days, the waiver span must be closed If the member dies the SD must be updated to reflect the death for EW members If the EW member loses eligibility for MA, and therefore loses EW, the waiver span must be closed Special Status Notification/Notification of Change Needed The Delegate must notify Blue Plus about the following by completing and faxing the 6.08 Notification of Member Change Needed to IHM—GP at 651-662-6054 or 1-866-800-1665: Member moves and requires a change in care coordination. Date of death Institution-based services: Fax this form if the member moves from the Community to a nursing facility for a long term placement (> 180 days) and the case needs to be transferred to a Nursing Home Care Coordinator outside of your agency. Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 25 Coordination of Potential Denials, Terminations, and Reduction of Services—Blue Plus will review notifications of Denial, Termination, and Reduction of Services for State Plan and Elderly Waiver Services. State Plan Home Care Services If the Care Coordinator, not the provider, recommends a DTR of State Plan Home Care Services, the Care Coordinator shall fax in the 6.05 Notification of Potential Denial Termination or Reduction of Services form to Blue Plus IHM-GP. Blue Plus will review the request for Medical Necessity and if a DTR is needed will the fax a copy of the DTR to the Care Coordinator and will mail a copy to the member. Note: Fluctuations in a member’s plan of care is not a DTR. Elderly Waiver Services The care coordinator will evaluate waiver services and if it has been determined that the members needs can be met with fewer or different waiver services, and the member has not initiated the reduction or termination, the care coordinator shall fax the 6.05 Notification of Potential Denial, Termination or Reduction of Services form to Blue Plus within 24 hours of the determination. Blue Plus will review the request to determine if a DTR should be issued according to Blue Plus’ guidelines. BluePlus may contact the Care Coordinator with any questions. If a DTR is determined to be appropriate, Blue Plus will then fax a copy of the DTR to the Care Coordinator and will mail a copy to the member. Grievances/Complaint Policy and Procedure Definitions Grievance Grievances are verbal or written expressions of dissatisfaction about any matter other than an Action (see definition below), including but not limited to, the quality of care or services provided or failure to respect the member’s rights. Some examples of grievances include: the quality of home delivered meals (food is cold), transportation providers being late, dislike of a roommate in the nursing home, impolite staff, in ability to access services appointment, missed or delayed diagnosis, or lack of treatment. Grievances can be filed either orally or in writing. Grievant The grievant is the person that is submitting the grievance for consideration. This may be a member, any individual acting on behalf of the member, or a provider with the member’s written consent. Action An action is a denial or a limitation of an authorization of a requested service, which includes: • The type or level of service, • the reduction, suspension or termination of a previously approved service Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 26 • the denial, in whole or in part for the payment for a service • The failure to provide services in a timely manner • The failure of the health plan to act within the required timeframes for resolution of appeals and grievances. • For a resident of a rural area with only one Health Plan, the denial of a Medicaid member’s request to exercise services outside of the network. Appeal An appeal is a request to change a previous decision or action made by the health plan. Appeals may be filed orally or in writing. Authorized Representative An authorized representative is an individual that is authorized by the member, or a surrogate who is acting in accordance with State law on behalf of the member in order to obtain an organization determination or deal with any level of the appeals process. Delegate Responsibilities The delegate must have a Policy and Procedure and system in place for handling grievances for MSHO/SecureBlue, and MSC+/Blue Advantage. A copy of written grievances, if submitted to the Delegate, must also be retained in the member’s file. A contact person will need to be established by each delegate for grievances. The contact person will be responsible to obtain any necessary information to resolve written or oral grievances submitted directly to us. The delegate must be able to retrieve records within two business days. Required Oral Grievance Member Assistance Care Coordinators should direct members to report all oral grievances to Blue Plus by calling member services, seven (7) days a week 8:00 a.m. to 8:00 p.m. Central Time. Care Coordinators may also call Blue Plus to report an oral grievance on behalf of the member if the member requires assistance. MSHO/MSC+ Member services number is: MSHO (651) 662-6013 or 1-888-740-6013 (Calls to this number are free) TTY users call: (651) 662-8700 or 1-888-878-0137 (Calls to this number are free) MSC+ 651-662-5545 or 1-888-711-9862 (Calls to this number are free) TTY users call: (651) 662-8700 or 1-888-878-0137 (Calls to this number are free) Written Grievances If a member requests the assistance of the Care Coordinator in filing a written grievance, the grievance should be transcribed in the member’s words and faxed to Blue Plus Consumer Service Center within one business day of the receipt of the grievance. Fax: 651-662-9517 or call 651-662-5545 or 1-800-711-9862 Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 27 The information faxed to Blue Plus should include both the written grievance and all other pertinent information or documentation related to the grievance. Blue Plus Consumer Service Center may contact the delegate for additional information during investigation of the grievance. Blue Plus 6.11 Grievance Form may be used to document the written grievance. Original documentation should be maintained on file by the delegate. EW Conversion/Request to Exceed case mix cap Conversions: A request for a higher monthly case mix budget cap may be submitted to Blue Plus for review and consideration if an EW eligible member; wishes to live in the community and is a resident of a certified nursing facility and has lived there for 30 consecutive days or more and their needs cannot be met within the assessed Case Mix budget Cap: Please see DHS Bulletin 12-25-01 Elderly Waiver- Conversion Rates and Maintenance Needs Allowance changes. Requests to exceed Diversion Case Mix Budget Cap: If a member has a unique set of assessed needs that require care plan services above their budget cap and there are no other informal support options, a request for a higher monthly case mix budget cap may be submitted to Blue Plus for review and consideration First-time requests must take place prior to the service initiation. A reauthorization request of a previously approved rate must be made at least 30 days prior to the end of the current authorization period. To request a Conversion/Exceed Cap rate, the Care Coordinator must fax the following information to the attention of EW Review Team, at 651-662-6054 or 1-866-800-1665 following the time frames above: Either the DHS EW Conversion Rate Request form (Attachment C of Bulletin 12-2501) or the 6.27 Blue Plus Exceeds the Case Mix Cap form Copies of member Care Coordination case notes for previous 2 months A copy of the member’s LTCC assessment completed within the previous 60 days A copy of the Plan of Care A description of what other options within the member’s current budget have been considered and why they are not possible A copy of Customized Living tool, if appropriate, or a copy of the budget which differentiates between service costs vs. room and board if moving in or living in a foster care Any other supporting documents deemed appropriate Other documents requested by the EW Review Team Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 28 The Blue Plus Review Team will: Review the request within 10 business days/14calendar days, whichever is sooner, of the receipt of all the required information/documents Will confer with the Care Coordinator if the documentation provided does not support the requested level of service Consult with the submitting Care Coordinator to ask for clarification or request further documentation as needed Consult with the IHM-GP Medical Director as needed Approve, deny, or recommend a change in the budget rate request If request is approved, Review Team will: Determine the length of time for the approval. Initial Conversion Rate for members transitioning out of a nursing facility, authorization will be given for a six month period. This will allow the Care Coordinator and the EW Review team time to determine if the member is stable in their new community environment and if services and rates need to be adjusted to meet any changes in the identified needs of the member Reauthorization without Change in Level of Service: If the EW Review team agrees with the level of services authorized for members who have previously transitioned to the community using an approved EW conversion budget, Blue Plus will reauthorize the budget for a twelve month period. This applies to current and newly enrolled MSC+ /MSHO members Reauthorization with Change in Level of Service: If the EW Review Team assesses the member to need a different level service than what was previously authorized for a member who has transitioned to the community using an approved EW conversion budget, the authorization period will be for six months. This will allow the Care Coordinator and the EW Review Ream time to determine if the member is stable with the new service levels and if services and rates need to be adjusted to meet any changes in the identified needs of the member Requests to Exceed Case Mix Cap: Requests to exceed the case mix cap approval period will be determined based on the member needs and reason for exception, not to exceed a twelve month period EW Review Team will then: Send notification to Bridgeview Company Send notification to Care Coordinator The Care Coordinator must: Place the full CAP amount (rather than the higher conversion rate/approved amount that exceeds case mix cap) in the Case Mix/DRG Amount field on the LTC screening document. If the request is not approved, the EW Review Team will: Advise the Care Coordinator on how to assist the member to look at other options which may include adjusting the level of service to more appropriately reflect the documented need and/or explore other provider options Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 29 IHM-GP Clinical Guides will then: Issue a Denial, Termination, or Reduction (DTR) letter to the member and Care Coordinator within 10 business days/14calendar days, whichever is sooner, of the receipt of all the required information/documents. Interpreter Services (Added September 2012) The Blue Plus contract with the Minnesota Department of Human Services requires that persons with limited English proficiency receive language assistance as necessary. If a Blue Plus member does not speak English as their primary language and has a limited ability to read, speak, write or understand English, the Care Coordinator may initiate the use of a Blue Plus contracted interpreter to assist in assessment, care planning and on-going care coordination. Blue Plus prefers the use of a formal interpreter over a family member, as best practice. A list of Blue Plus contracted providers is available in the Blue Cross Blue Shield provider manual, chapter 3. You can click on the link below or copy and paste this web address into your browser: http://www.bluecrossmn.com/bc/wcs/groups/bcbsmn/@mbc_bluecrossmn/documents/public/pos t71a_023249.pdf To initiate the process for interpreters or for any questions contact our Member Services at 651662-6013 or 1-888-740-6013. For Face-to-Face Interpreters: The Care Coordinator can also initiate the process by contacting an in-network provider directly. For Over-the-Phone Interpreters: The Care Coordinator may contact Via Language or Language Line as described in the instructions provided by your Partner Relations Consultant. If the Blue Plus member is requesting information about the use of an interpreter for their medical appointments (such as a clinic visit), the member should be directed to Member Services. OTHER CARE COORDINATION RESPONSIBILITIES 1. PIPs—The Care Coordinator will participate in the on-going performance improvement projects that are designed to achieve significant favorable health outcomes for members. These projects incorporate standards and guidelines outlined by the Centers for Medicare and Medicaid (CMS) with input by the Minnesota Department of Human Services (DHS). 2. Fraud, Waste, and Abuse Training is required for 2012. Curriculum will be provided annually. 3. Documentation—The Care Coordinator shall document all activities in the member’s case notes. Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 30 4. The Care Coordinator shall comply with any applicable Federal and State laws that pertain to member rights including HIPAA laws and the Minnesota Data Privacy Act and your organization’s confidentiality policy. 5. The Care Coordinator should be coordinating with local agency case managers (mental health, developmental disabilities, adult protection, etc), financial workers and other staff as necessary to meet the member’s needs. This includes using the Case Manager/Financial Worker Communication Form (DHS # 5181) when: A member requests waiver services A member receiving waiver services has a change in circumstances (exits waiver, moves to SNF, expires, etc) For more information refer to DHS Bulletin #07-21-09 Out of Network Providers Elderly Waiver Network—Blue Plus does not contract directly with EW service providers. 1. Vendors within the Delegate’s County Network. If the Care Coordinator determines that a member needs covered services from a vendor with no current contract, the Delegate may enter into a one-time service agreement. This one-time contract will include the procedures needed to reimburse the provider for the services. 2. Vendors Outside of the Delegate’s County. If the Care Coordinator determines that a member needs covered services from a vendor not in the county’s network, the Care Coordinator will determine if the requested vendor has a Lead County contract in another county. The Care Coordinator will contact the Lead County to determine if services may be authorized under the Lead County contract. Blue Plus Network 1. Blue Plus members do not have out of network benefits for services that are not emergent/urgent. (i.e., Our member, Mildred, is visiting her daughter in Missouri and needs outpatient I.V. therapy. This service is not emergent/urgent and thus would not be covered) Note: Questions related to in-network providers and benefit questions should be directed to Provider Services at 1-800-262-0820 or 651-662-5200. Out of Country Care—Medicaid. Effective 1/1/12, Medicaid payments, including EW, will not be made: 1. For services delivered or items supplied outside of the United States; or 2. To a provider, financial institution, or entity located outside of the United States. United States includes the fifty states, the District of Columbia, the Commonwealth of Puerto Rico, the Virgin Islands, Guam, American Samoa, and the Northern Mariana Islands. Reminder: Any Benefit questions should be directed to Member Services. Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 31 Audit Process—The BluePlus contract with DHS and CMS requires the auditing of care coordination activities on an annual basis. Records Retention Policy The Delegate must have policies and procedures to address record retention in accordance with DHS and Center for Medicare and Medicaid Services rules and regulations. Files, either in electronic or hard copy format, are to be kept for 10 years from the date the files are closed. After 10 years the files may be destroyed. File information includes: patient identification information, provider information, clinical information, and approval notification information. All documents pertaining to pending litigation or a regulatory matter must be retained despite general disposal policy until Blue Plus advises that such documents may be returned to the general disposal policy. Care Coordination Services Overview The Care Coordinator will work with the member with support from IHM-GP staff and/or Government Programs staff to assure that the member has access to the following services as needed: 1) Rehabilitative Services. These are services that promote the rehabilitation of members following acute events and for ensuring the smooth transition and coordination of information between acute, sub acute, rehabilitation, nursing home and community settings. 2) Range of Choices. The care coordinator is key in ensuring access to an adequate range of choices for members by helping the member identify formal as well as informal supports and services, ensuring that the services are culturally sensitive. Interpreter services are available for all BluePlus members. 3) Coordination with Social Services. The Care Coordinator will collaborate with the local Social Service Agency when the member may require any of the following services: Pre-petition Screening OBRA Level II Screening Spousal Impoverishment Assessments Adult Foster Care Group Residential Housing and Board Payments; or Extended Care or Halfway House Services covered by the Consolidated Chemical Dependency Treatment Fund Targeted Mental Health Case Management Adult Protection 4) Coordination with Veteran’s Administration (VA). The Care Coordinator shall coordinate services and supports with those provided by the VA if known and available to the member. 5) If the Care Coordinator receives notification of a member’s hospital admission, contact will be made with the hospital social worker/ discharge planner, to assist with Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 32 discharge planning. The Care Coordinator can work with the discharge planner, member or home care nurse (if appropriate) to complete the following: Assess the member’s medical condition; Identify any significant health changes; Reassess and revise the CSP for the member to meet their new health needs, if required; and Schedule an interdisciplinary team conference, if needed at this time. 6) Identification of Special Needs and Referrals to Specialists. The Care Coordinator should have the ability to identify special needs that are common geriatric medical conditions and functional problems such as polypharmacy issues, lack of social supports, high risk health conditions, cognitive problems, etc. and assist the member in obtaining specialized services to meet identified needs. Care Plan Service and Guidelines Delegate staff use professional judgment interpreting the following guidelines to make decisions related to the care and treatment of their SecureBlue members: MN rules and statutes, DHS policies and training, County program training and guidelines, Provider training and guidelines, Medicare coverage criteria, Long Term Care Screening Document, Disease Management protocols, Case mix caps/budget, and SecureBlue Certificate of Coverage Care Coordination Delegation Guidelines for Blue Plus MSHO Community Members Page 33