NSF for Arrhythmias: A North-West Regional
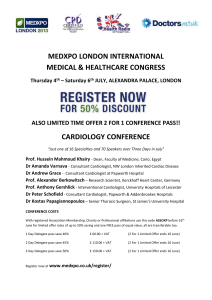
advertisement
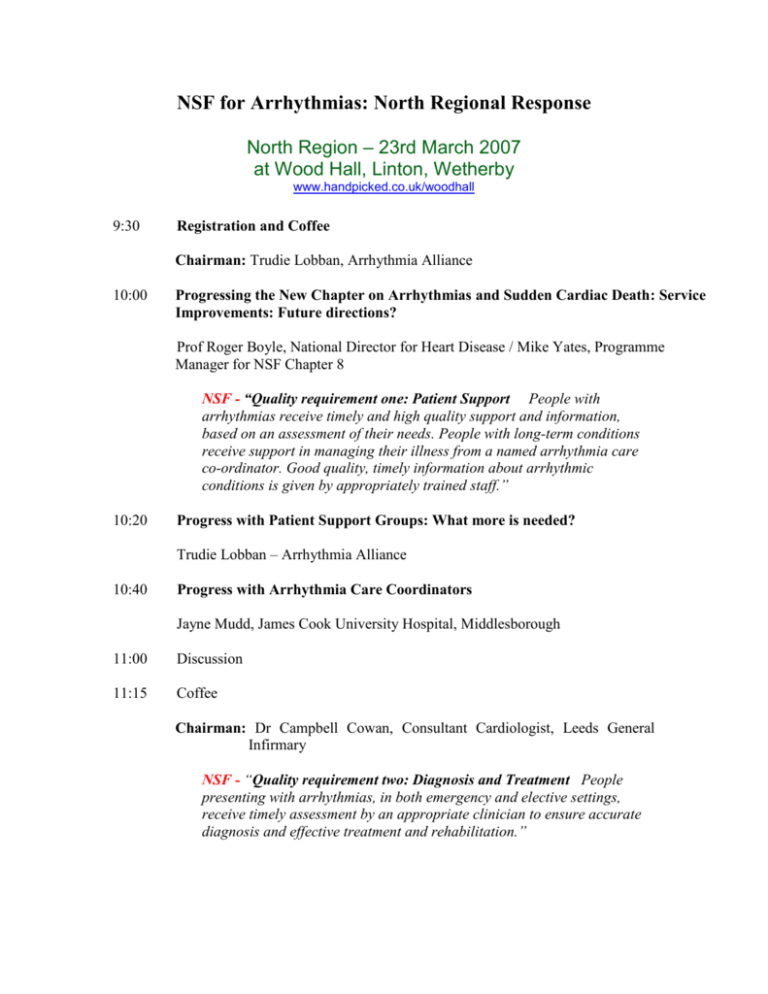
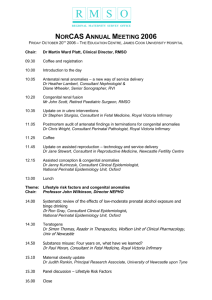
NSF for Arrhythmias: North Regional Response North Region – 23rd March 2007 at Wood Hall, Linton, Wetherby www.handpicked.co.uk/woodhall 9:30 Registration and Coffee Chairman: Trudie Lobban, Arrhythmia Alliance 10:00 Progressing the New Chapter on Arrhythmias and Sudden Cardiac Death: Service Improvements: Future directions? Prof Roger Boyle, National Director for Heart Disease / Mike Yates, Programme Manager for NSF Chapter 8 NSF - “Quality requirement one: Patient Support People with arrhythmias receive timely and high quality support and information, based on an assessment of their needs. People with long-term conditions receive support in managing their illness from a named arrhythmia care co-ordinator. Good quality, timely information about arrhythmic conditions is given by appropriately trained staff.” 10:20 Progress with Patient Support Groups: What more is needed? Trudie Lobban – Arrhythmia Alliance 10:40 Progress with Arrhythmia Care Coordinators Jayne Mudd, James Cook University Hospital, Middlesborough 11:00 Discussion 11:15 Coffee Chairman: Dr Campbell Cowan, Consultant Cardiologist, Leeds General Infirmary NSF - “Quality requirement two: Diagnosis and Treatment People presenting with arrhythmias, in both emergency and elective settings, receive timely assessment by an appropriate clinician to ensure accurate diagnosis and effective treatment and rehabilitation.” 11:30 Update on the Development of Inherited diseases clinic and the progress made at Leeds. Dr Jonathan Parsons, Consultant Cardiologist, Leeds General Infirmary 11.50 Primary Care – What needs to be done? Dr Matt Fay, Bradford 12:10 Rapid Access Arrhythmia and Blackouts Clinics Dr Steve Parry, Consultant Cardiologist, Newcastle 12:30 Discussion 12:40 Lunch Chairman: Jayne Mudd, James Cook University Hospital, Middlesborough NSF - “In recent years there have been significant improvements in both technology and clinical skills that are enabling improved prevention, diagnosis and treatment of these conditions. Implantable cardioverter defibrillators (ICDs) and sophisticated pacing devices have given cardiologists many more treatment options for these patients.3 For some conditions, catheter ablation, which treats malfunctioning parts of the heart ,provides a cure so that patients no longer require medication or suffer from palpitations..” 13:30 Atrial Fibrillation guidelines in Practice - Supporting Primary care through Education Julia Neal 13:45 Arrhythmia Care in the DGH: What Progress? Dr Chris Morley, Consultant Cardiologist, Bradford 14:10 Arrhythmia Care in Tertiary Centres: What needs to be done? Dr Chris Pepper, Consultant Cardiologist, Leeds General Infirmary 14:40 Discussion 15:00 Tea Chairman: Dr Chris Pepper, Consultant Cardiologist, Leeds General Infirmary NSF - “Service improvements can be achieved locally by several means: guidance on making the initial diagnosis and on management by readily accessible approved algorithms; improving access to a higher level of expertise by development of rapid access multidisciplinary arrhythmia and/or blackouts clinics; focused education of key carers; improving access to diagnostics at all stages; and improving acquisition, storage and availability of clinical information such as ECGs and audit of all interventions.” 15:30 Heart Improvement Programme – Future Plans Dr Campbell Cowan, Consultant Cardiologist, Leeds General Infirmary 15.30 Local Cardiac Network perspective – Setting up an AF Clinic in general practice Alison Bagnall and Chris Beith, West Yorkshire Cardiac Network 16:10 Q&A