N222 Lecture 12 - College of San Mateo
advertisement

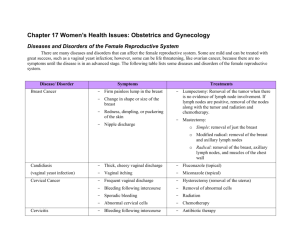
1 Disorders of the Female/Male Reproductive Systems Lecture 12 I. Breast Masses A. Screening for breast masses 1. Breast self exams a. best if done 5-7 days after menses has stopped b. if periods are not regular, chose the same day each month c. while on back, palpate each breast in a circular or vertical motion to cover whole breast d. use finger pads to ck for indentations, change in contour/texture, lumps e. compress nipple to ck for discharge f. may also do while standing/in the shower g. note size and shape usually equal but not always symmetrical h. vary with woman’s age, nutritional status, and heredity i. contour should be smooth without puckering or dimpling j. assess nipples for shape, direction, rashes, ulcerations, and discharge k. 90% of brst lumps found by women -20-25% will be malignant 2. Exam by clinician a. usually done with yearly pelvic exam b. should not be on period at time of exam c. may request mammogram for women with dense breast tissue or palpable changes -mammograms-ACS guidelines-updated 10/2015 -for women at average risk age 40-44-annual if desired (risks vs benefits) age 45-54-annual age 55 and older-every 2 years or have the choice of yearly →Screening should continue as long as a woman is in good health and is expected to live 10 more years or longer. B. Benign Breast Disorders 1. Fibroadenoma a. occurs in women from puberty to menopause b. risk factors -nulliparity -low parity -later menopause -estrogen therapy -family h/o of brst CA c. masses are solid and made of connective tissue d. cause unknown e. usually solitary lump < 1cm to 15 cms in diameter 2 f. g. h. i. lump may be tender during menses diagnosed by mammogram, U/S, MRI doesn’t respond to changes in diet/hormones may need surgical excision if lump suspicious or symptoms are severe 2. Fibrocystic breast condition a. most common breast problem-mostly found in upper, inner quadrant of breast b. characterized by lumpiness, with/without tenderness, and may be associated with changes in menstruation c. 70% nonproliferative (benign growing cells) d. others are proliferative lesions with atypical hyperplasia (↑ risk of brst CA) e. ↑ risk of brst CA with relative having brst CA f. etiology-unknown-possibly R/T imbalance of hormones g. usually in both breasts but may be singular h. S & S develop one week before menses -dull, heavy pain -sense of fullness -increasing tenderness i. cysts are usually soft, well differentiated, movable j. deeper cysts may not be differentiated from carcinomas k. U/S to determine if fluid filled-if so-aspirate l. if solid, mammogram followed by fine needle aspiration (FNA) or core biopsy m. management -dietary changes-↓ caffeine -↓ Na intake -Vit. B, C, and E supplements -use NSAIDS -some relief with ↓ smoking/alcohol intake -supportive bra -heat packs to breasts 3. Ductus ectasia a. inflammation of ducts behind nipple b. etiology-unknown c. occurs most often in perimenopausal women d. characterized by thick, sticky nipple discharge either white, brown, green, or purple in color e. other S & S: burning pain, itching, palpable mass behind nipple f. workup: mammo, aspiration, culture of fluid g. Tx: symptomatic -no stimulation -good breast hygiene -I & D if abscess develops -abx -may need affected duct excised 4. Intraductal papillomas a. found in women 30-50 years of age b. rare, benign lesion in the terminal nipple ducts -may be too small to palpate (2-3 cm) c. may note nipple discharge-serosanguinous d. do fluid Pap smear of nipple discharge 3 e. C. Tx: excision Breast cancer-Cancer.org (American Cancer Society) 1. Pathophysiology a. most common infiltrating ductal carcinoma -abnormal cells grow in the epithelial cells which line the mammary ducts -needs 5-9 years to be palpable b. noninvasive if stays in duct (ductal carcinoma in situ or DCIS) c. invasive if penetrates the tissue around the duct d. invasion of lymphatic channels/lymph ducts carry abnormal cells to lymph and to metastatic sites e. staging of disease must include lymph node examination, especially axillary nodes f. metastatic sites include bone, lungs, brain, liver 2. Etiology/risk factors/incidence a. exact cause unclear b. ↑ risk with ↑ of woman’s age c. other risk factors-family history -previous h/o brst CA -family history -h/o ovarian, endometrial, colon, or thyroid CA -early menarche (before age 12) -later menopause (after age 55) -nulliparity -first preg. ≥ age 30 -HRT -obesity -h/o benign breast disease with hyperplasia -Caucasians -African-Americans have a higher mortality rate due to late diagnosis -sedentary lifestyle -high SES d. incidence -in US, 1 out of 8 women will develop brst CA -risk factors help identify less than 30% of women -5% of brst CA attributed to heredity -↑ risk for women with abnormal BRCA1/BRCA2 genes -testing expensive -often not covered by insurance -debate R/T prophylactic mastectomies or Tamofixen use -↑ risk of brst CA with use of HRT -occurs in men < 1 % 3. Clinical manifestations a. physical -most lumps in upper outer quadrant -may feel lump or thickening of brst -hard and fixed, soft and spongy 4 -well-defined or irregular borders -may cause dimpling due to fixed to skin (orange peel) -may have nipple discharge-bloody or clear b. c. d. e. f. g. h. i. psychosocial -denial -grief and loss behaviors mammogram/U/S/MRI nipple discharge exam-culture/specimen to lab ductogram-fine plastic tube placed into duct, contrast media injected, assess duct FNA biopsy-aspiration or core-may use guide wire Triple test-physical exam, mammogram, FNA -if any benign-98% of lesion being benign staging-TNM-T=size, N=nodes, M=metastases -Stage 0-ductal carcinoma (in situ)-earliest form -Stage 1-2 cm tumor/hasn’t spread -Stage 2-tumor >2 cm-in axillary nodes on same side -Stage 3-tumor >5 cm-spread to lymph nodeslocalized spread, no other organs -Stage 4-metastasis to distant-bones, lungs, liver lymph nodes not local 4. Nursing diagnoses a. pain R/T surgical procedure b. risk for infection c. body-image disturbance R/T loss of body part 5. Management a. surgery -lumpectomy (tylectomy, partial mastectomy) -removal of tumor -removal of small surrounding area -sampling of axillary lymph node -doesn’t effect pectoral muscle -may follow-up with 6-7 weeks of radiation -modified radical mastectomy -removal of entire breast -sample of lymph nodes -spares pectoral muscle -risks: infections, hematoma lymphadema, limitation of arm/shoulder mobility -sentinel lymph node biopsy (SLNB) -radioactive tracer/dye injected -carried by lymph to sentinel node which is first node to receive lymph from tumor 5 -most likely to contain metastasis if CA has spread -if sentinel node is cancerous, more nodes are excised b. c. 6. II. -reconstructive surgery -goal is achievement of symmetry with preservation of body image -3 types of autologous flap reconst. -latissimus dorsi -TRAM-transverse rectus abdominis myocutaneous -inferior gluteus free -monitor skin flap for ↓ cap. refill, hematoma, infection, necrosis -may also receive breast expanders→ implants adjuvant therapy-radiation -after lumpectomy in non/microinvasive cases -any invasive ductal carcinoma <1 cm diameter -interstitial or balloon brachytherapy -intraoperative radiation adjuvant therapy-drug therapies -chemotherapy started soon after dx -most useful in premenopausal women with brst CA with + nodes -can increase time without CA -may be given alone or with HRT -tamoxifen attaches to hormone receptor on CA cell-cell unable to grow -side effects-leukopenia, neutropenia, anemia, thromobocytopenia, GI problems, hair loss Discharge planning -resources ACS Reach for Recovery program NCCN-National Comprehensive Cancer Network ACS home page Sexually Transmitted Diseases/Infections A. Infections associated with ulcers 1. Syphilis a. caused by treponema pallidum-spirochete b. transmission thru abrasion of tissue, kissing, biting, oral-genital sex c. can cross the placenta d. 120,000 new cases each year e. higher rates in young African-Americans f. attributed to use of sex for drugs/money g. primary-chancre appears day 5-90 post infection-nontender, shallow, indurated h. secondary-occurs 6 weeks-8 months 6 i. j. j. 2. -wide spread maculopapular rash on palms/soles -fever, headache, malaise -may have condylomata lata tertiary-neurologic, CV, MS, or multiorgan system complications screening: -microscopic exam of lesions -serology-VDRL/RPR-may have false + -MHA-TP-microhemagglutination assays for antibody to T. pallidum used to confirm + tests -seroconversion takes 6-8 weeks post exposure management: -PCN G IM -treats primary, secondary, and early latent -if syphilis older than 1 year, weekly shots for 3 wks -alternatives: doxycycline, tetracycline -not used in pregnancy - erythromycin-unlikely to cure fetal infection Genital herpes simplex a. results in painful, reoccurring ulcers b. HSV-1-usually nonsexually transmitted -oral labial ulcers -gingivostomatitis c. HSV-2-transmitted during oral/genital sex d. not a reported disease e. 20% Americans infected with virus-over 50 million people f. estimated 1 out of 4 women will get HSV-2 g. initial infection: -fever, chills, malaise -severe dysuria -painful lesions-may last 2-3 weeks h. lesions may progress from macule→papule→ vesicle→pustule→ulcer that crusts→scar i. can cause cervical problems, purulent vaginal vaginal discharge and urinary retention j. reoccurring episodes not as severe k. HSV-2 can have adverse effects on mom/fetus -viremia -congenital infection -60% infant mortality if infant contracts HSV l. association between cervical CA and HSV-2 m. screening: -physical exam with complete H & P -viral culture of ulcer n. management: -chronic/reoccurring -proper hygiene -systemic antiviral medications -acyclovir, valacyclovir, famiciclovir -sitz bath with baking soda -oral analgesics -diet rich in Vit. C, B, zinc, and calcium 7 -kelp powder, sunflower seed oil -relaxation techniques -support groups -condoms to prevent transmission to new partner -C/section delivery if primary outbreak -counseling to deal with shame, guilt, anger 3. 4. 5. B. Lymphogranuloma venereum-CDC.gov-look for Facts Sheets Chancroid Granuloma inguinale Infections of Epithelial surfaces 1. Human papilloma virus-HPV a. 100+ HPV types, 40 known mucosal serotypes b. 90% of cases cleared by immune system in 2 years c. if not cleared, can lead to genital warts, warts in the throat, cervical cancer d. ages at risk for HPV 14-19yrs old→26.8% 20-24yrs old→44.8% 25-29yrs old→27.4% e. may look like a cauliflower-mass f. rarely transmitted to neonate at birth g. screening: -S & S-dyspareunia, itching, discharge, bumps -may need to change gloves between vaginal and rectal exams to prevent spread h. Diagnosis -cervical exam to include Pap smear & HPV test -pap only 30-60% sensitive -HPV screen is 90% sensitive -cervical screening guidelines-start at age 21 (whether or not sexually active) -intervals-every 2-3 yrs 21-29 if pap neg -every 3 yrs 30-65 if pap/HPV neg -age 30-HPV neg-1% risk (99% cx CA from HPV-low progression-8.1 to 12.6 yrs) -age 65 w/ 3 consequential neg paps in last 10 yrs -stop needing paps -colposcopy to view growth with biopsy i. need to differentiate between HPV &: -molluscum contagiosum-white papules -condylomata lata-secondary syphilis j. Prevention-vaccine Gardisil-start at age 9-26 -killed vaccine -give prior to sexual debut or early after -not given after >5 partners -series of 3 injections/6 mo -$$$, unaffordable to uninsured -lifetime immunity but still needs paps since not all strains covered k. Tx-no treatment can eradicates HPV-only symptoms 8 -imiquimod, podophyllin, podofilox-topical -cryotherapy 2. Gonorrhea a. caused by Neisseria gonorrhoeae-bacteria b. 700,000+ contract gonorrhea each year c. rising incidence of drug-resistance d. transmission: oral, genital, anal e. higher incidence in people under 20 years old f. higher incidence in African-Americans g. women most often asymptomatic h. may present with pain/burning with urination, vaginal discharge, low back pain h. men may c/o pain with urination and yellowish discharge from penis i. may take up to 3-10 days before symptoms present j. screening: cultures taken from endocervix, rectum, and possibly pharynx k. people are frequently coinfected-should be tested for other STI’s l. management: usually single dose antibiotic: ceftriaxone m. 45% women will also have chlamydia so should have concomitant tx 3. Chlamydia a. caused by Chlamydia trachomatis b. most common/fast spreading STI in women c. untreated leads to PID and acute salpingitis d. may caused ulcers on the cervix increasing 9 e. f. g. h. i. j. k. l. m. n. 4. risk to acquire HIV higher incidence in women under age 20 sexually active individuals ≤ 25 yrs old-screen for chlamydia yearly all pregnant women should be screened at first PN visit repeat cultures if woman was previously + or has multiple partners may have spotting, postcoital bleeding, cervical discharge, or dysuria dx thru culture management-doxycycline or azithromycin if pregnant-erythromycin/amoxicillin since usually asymptomatic, must encourage completion of all the medication women tx with erythromycin need to be retested in 3 weeks due to poor validity of tx PID-Pelvic Inflammatory Disease a. involves fallopian tubes (salpingitis), uterus (endometritis), and possibly ovaries and peritoneal surfaces b. caused by multiple organisms and occasionally caused by more than one c. most commonly caused by C. trachomatis d. also caused by gonorrhea and other aerobic and anaerobic bacteria e. microorganisms spread from vagina to upper genital tract-usually occurring at the end of or just after menses f. during menses, spread supported by open cx, decrease cervical mucus, and blood used as a medium for growth g. each year, 1 million women will experience symptomatic PID h. risk factors: teens, multiple partners, new partners, history of PID, use of IUD i. leads to: risk for ectopic pregnancy, infertility, chronic pelvic pain, dyspareunia, pyosalpinx, abscesses, adhesions j. S & S: dull, cramping, or severe pelvic pain, bleeding, adnexal tenderness, pain with cervical movement (Chandelier sign), bilateral pelvic tenderness k. screening: good history taking to r/o other causes, temp ↑38.3 0 C, abnormal cervical/vaginal discharge, ↑ sed rate, lab documentation of chlamydia or gonorrhea l. need to teach prevention of causes to help prevent disease m. need to screen asymptomatic women with 10 n. o. p. q. III. history of risky behavior tx: usually broad-spectrum abx, use analgesics, semi-fowlers position while resting encourage rest, proper nutrition, and hydration will need follow-up lab work to confirm cure teaching to include use of barrier methods, no sexual relations until completion of meds, follow-up pelvic exams, and other contraceptive methods other than IUD’s Gynecologic Disorders A. Postmenopausal bleeding-bleeding 12 months post menses cessation 1. Related factors a. atrophic vaginitis-tissues more sensitive, bleed easily b. polyps-masses in/on the cervix c. endometrial problems -endometrial hyperplasia may be a precursor to endometrial CA-need a D & C to evaluate d. ↓ ovarian function → ↓ estrogen/progesterone 2. Management a. for vaginitis-use of creams to protect tissues b. for polyps-removal c. HRT 3. Discussion regarding HRT a. most studies show ↑ risk factors and adverse reactions R/T dose and length of tx b. controversy R/T method of administration, doses, and efficacy c. must individualized to pt’s S & S , lifestyle, and medical history -need to deal with philosophy/beliefs regarding exohormones d. if ERT alone, 5-10X risk of endometrial CA e. problem with adding progesterone, bleeding f. new studies proving that HRT may lead to ↑ risk for brst CA g. short term HRT (1-5 years)-no protections against osteoporosis or CVD -risk factors for osteoporosis family history short, thin European or Asian descent early menopause smoker, alcohol use caffeine use, low calcium intake sedentary lifestyle use of steroids, synthyroid, diuretics -risk factors for CVD 11 h. B. ↑ LDL, ↓ HDL, ↑ total serum cholesterol ↑ risk of atherosclerosis MI emboli thromboses long term-may use estrogen alone or in combination with progesterone or testosterone -may be continuous or cyclic Endometriosis 1. Assessment a. benign disease characterized by implantation of endometrial tissue outside the uterus b. implanted on the ovaries, cul-de-sac, uterine ligaments, rectovaginal septum, sigmoid colon, pelvic peritoneum, cervix, and inguinal area c. endometrial lesions can be found in the vagina, surgical scars, vulva, perineum, bladder, and other sites such as thoracic cavity, gallbladder and heart d. tissue responds to hormonal stimulation e. tissue bleeds during or after menses causing inflammatory response by adjacent organs/tissues f. can lead to scars and adhesions g. incidence -10% in women of reproductive age -25-35% infertile women -28% of women with chronic pelvic pain h. each year account for almost 50,000 hysterectomies i. may remain asymptomatic and disappear after menopause j. may worsen with repeated cycles k. found across all SES levels l. most widely accepted cause-retrograde menstruation -estimated to occur in 96% of women who menstruate m. possible reasons why some women develop the condition -individual immune system fails to destroy tissue -differences in genetic make-up -environmental challenges n. S&S -pain (dysmenorrhea)-possibly prior to menses -lower abdomen pain -dyspareunia -painful defecation -hypermenorrhea -sacral back pain -infertility 12 2. C. Management a. NSAIDs b. suppression of endogenous estrogen production medically induced menopause -GnRH agonists (gonadotropin-releasing hormone) i.e. Lupron, Synarel ↓pituitary gonadotropin secretion→ ↓FSH/LH stimulation of ovaries→ ↓ovarian function→hot flashes, vaginal dryness limited to 6 months R/T bone loss potential teratogen -androgen derivatives Danocrine (danozol) suppress FSH/LH secretion produces anovulation regression of endometrial tissues may produce masculinizing traits weight gain edema deepening of voice oily skin hirsutism ↓ in brst size other side effects H/A hot flashes vaginal dryness ↓ libido insomnia fatigue dizziness ↓HDLs ↑ LDLs contraindicated-h/o liver disease use with caution if h/o heart or renal disease fetus-pseudohermaphroditism c. may use OC’s with low E to P ratio to shrink endometrial tissues SE: N & V, bleeding, edema d. mifepristone (RU-486) being used with success e. surgery-nd to consider age, desire for children, location of disease -TAH-BSO -laser surgery to remove adhesions/tissue f. 40% reoccurrence-except in TAH-BSO cases Dysfunctional uterine bleeding-abnormal uterine bleeding 1. Wide variety of menstrual irregularities a. menorrhagia b. irregular cycles 2. Possible causes a. anovulation-polycystic ovary syndrome b. pregnancy-related-SAB 13 c. d. e. f. g. D. genital infections-chlamydial cervicitis neoplasms-CA of cx trauma-foreign body systemic diseases-DM iatrogenic-herbal preparations-ginseng 3. Severe bleeding with Hgb ↓8g/100ml=hospitalization a. given IV cong. estrogen (Premarin) b. possible D & C c. endometrial biopsy to r/o endometrial CA 4. Incidence a. teens-20% b. women under 50-50% 5. Management a. oral cong. estrogen X 21 days with progesterone (medroxyprogesterone-Provera) added for the last 7-10 days b. low dose OCP c. ablation of endometrium d. hysterectomy Inflammations and Infections 1. Vaginitis/Vulvitis a. inflammation of vagina and/or vulva b. S&S -irritation, malodorous abnormal discharge -itching, burning, urinary frequency -spotting c. causes -infections -lack of hormone estrogen -irritants/allergies chemicals medicines latex condoms spermicides diaphragm/cervical cap scented/colored toilet paper bubble baths douches laundry detergents hot tubs horseback riding wearing tight garments rubbing on a bicycle seat d. infections -candidiasis-yeast causes-abx, pregnancy, DM, problems immune system thick white odorless discharge in the mouth-called thrush tx-antifungal agents -bacterial vaginosis-BV caused by a variety of bacteria 14 e. 2. E. including gardnerella associated with PTL and birth etiology unknown heavy gray frothy malodorous D/C tx-oral metronidazole-Flagyl antiprotozoal/antibacterial contraindicated in women who breast feed may affect the CNS and hematopoietic systems with alcohol-can cause abdominal distress, N & V, H/A -trichomoniasis-anaerobic protozoan may be asymptomatic or have frothy musty-smelling discharge itching on or around the vagina spotting, urinary urgency tx-Flagyl-treat both partners since a STI-should screen for other STIs atrophic vaginitis-irritation without discharge -lack of estrogen due to childbirth, menopause, bilateral oophorectomy, radiation tx -estrogen creams restore lubrication and decrease soreness/irritation Toxic Shock Syndrome a. assessment -primarily a disease of the reproductive age -caused by S. aureus→produces toxin TSST-1 -risk factors-retained tampons, barrier devices left in place, surgery, recent delivery -S & S-fever >102 F, 38.9 C, hypotension, widespread macular rash, dizziness, N & V, diarrhea myalgia, inflamed mucous membranes -lab tests-↑ BUN, Cr, SGOT, SGPT, ↓ platelets b. management -mainly supportive -antibiotics-limited value -need to teach prevention, reoccurrence Problems R/T Pelvic Support Structures 1. Uterine Prolapse a. round ligaments hold uterus in anteversion uterosacral ligaments pull cx up and back b. 2 months PP, ligaments should return to normal length-1/3 of women, uterus remains retroverted c. causes: congenital or acquired pelvic relaxation -pregnancy -perimenopausal period -pelvic surgery 15 -pelvic radiation d. e. F. tx: -pessaries -estrogen creams -abdominal/vaginal hysterectomy education: use of Kegel exercises to strengthen pelvic floor muscles 2. Cystocele a. downward displacement of bladder-bulge in anterior vaginal wall b. causes: genetics, obesity, childbirth, advanced age c. S & S: urinary incontinence, vaginal fullness bulge in vaginal wall d. complete emptying of bladder difficult R/T the cystocele sags below the bladder neck e. tx: vaginal pessary or surgical repair colporrhapy (anterior repair)-shortens pelvic muscles to better support bladder 3. Rectocele a. herniation of anterior rectal wall b. may lead to constipation, hemorrhoids, fecal impaction, feeling of vaginal/rectal fullness c. found by rectal exam or barium enema d. need to promote bowel elimination e. surgery-posterior colporrhaphy or A & P repair f. follow surgery with low residue diet Common Benign Neoplasms 1. Types/Management a. ovarian masses -70-80% benign -S & S-asymptomatic -mass may be palpated on pelvic exam -may have a feeling of fullness, cramping -can lead to dyspareunia, irregular bleeding -may resolve on own -use of OC’s -diagnostic laparoscopy with possible laparotomy b. uterine masses -fibroids-leiomyomas -minimal CA risk -S & S-frequently asymptomatic -low abdominal pain, fullness, pressure -menorrhagia, dysmenorrhea -metrorrhagia (intermenstrual bleeding) -may shrink with menopause -myomectomy, D & C, hysterectomy 16 2. G. Total abdominal hysterectomy a. removal of uterus and cervix thru abdominal incision b. may include removal of fallopian tubes/ovaries BSO-bilateral salpingo-oophorectomy castration in females c. 600,000+ are done yearly d. questionable reasons for surgery e. may want to consider alternatives LAVH-laparoscopic assisted vaginal hyster. f. pre-op: lab work, ECG, chest x-ray, informed consent-must understand means sterility g. IV, shave, abdominal prep, Foley cath h. post-op care similar to post-op C/section i. need to deal with psychosocial issues Reproductive cancers 1. Endometrial a. most frequently occurring reproductive cancer b. 5th most common after skin, lung, breast, and colorectal c. asymptomatic in early development d. endometrial cancers are nearly all adenocarcinomas (80%) -cancer of glandular cells e. S &S-postmenopausal bleeding f. risk factors: obesity, advanced age, unopposed ERT, nulliparity, late menopause >age 52 Caucasians g. found by endometrial biopsy h. tests: CBC, liver function, renal function, BE, CT, liver and bone scan, CA-125 j. tx: radiation-intracavity (brachytherapy) -external beam chemo surgery-TAH/BSO 2. Cervicala. 3rd most common CA of reproductive tract b. risk factors -age (50-55) -early childbearing -non-Caucasians -smoking -multiple sexual partners -HPV→Gardasil vaccine c. testing -Pap smear -colposcopy -punch biopsy -ECC d. staging: Stage 0-carcinoma in situ-superficial Stage 1-invaded the cervix without spreading 17 e. Stage 2-CA has spread but remains in pelvis -5 year survival rate 65-80% Stage 3-CA spread to lower wall of vagina -5 year survival rate as low as 20-40% Stage 4-CA spread to distant organs tx: Stage 0-cryosurgery, laser surgery, LEEP/LEETZ, cone biopsy, hysterectomy (loop electrosurgical excision procedure) Stage 1-simple hysterectomy if cancer is more than 3mm-may want radical hysterectomy with removal of lymph nodes in the pelvis Stage 2-hysterectomy with high-dose radiation and chemo Stage 3 & 4-treatment and predictive prognosis varies on severity of spread and response 3. Ovariana. most often occurs in 5th decade (age 45-65) b. most occur after menopause c. risk factors -fertility drugs -early menstruation -nulliparity -high fat diet -smoking -alcohol -1st child after age 30 -h/o breast, colon, or endometrial CA -family h/o breast or ovarian CA d. ↓ risk -use of OC’s -h/o BTL -BSO e. 5 year survival rate-90% (Stage 1), 10% (Stage IV) -discovery of CA not until advanced stage f. S&S -irregular menses -PM tension -menorrhagia -breast tenderness -early menopause -abdominal discomfort -dyspepsia -pelvic pressure -↑ abdominal girth -urinary frequency g. in 75% of cases, CA had metastasized before dx -60% beyond the pelvis h. dx: transvaginal U/S, laparoscopy, laparotomy i. tx: -TAH/BSO -tamoxifen -chemo -radiation j. CA 125-associated with various epithelial CA may be used to assess response to tx in women with known ovarian CA 4. Vulvar a. 90% squamous cell carcinomas b. accounts for 4% of Gyn malignancies c. more than 50% of cases occur in 18 d. e. f. g. IV. postmenopausal women (age 65-70) usually localized, slow-growing, and marked by late metastasis to regional lymph nodes risk factors: HTN, obesity, DM S & S: bleeding, malodorous D/C, pain, pruritus tx: excision, laser, radiation, vulvectomy Male Reproductive DisordersA. Testicular Cancer 1. Leading cause of cancer deaths in men 15-35 yrs old a. highly treatable b. usually curable-over 90% in all stages combined c. rarely bilateral d. CA most commonly dx-solid tumor-age 15-40 e. most often in Caucasians, rare in African-Amer. 2. Pathophysiology a. germinal-sperm-producing cells-95%of cases -2 types seminomas- (40%) -occur in men late 30’s to early 50’s -localized-grow slow -metastasized later -response well to radiation -5 year survival rate-95% with surgery and radiation nonseminomas-not sensitive to radiation -occur in men late teens to early 40’s -need surgery or chemo -embryonal carcinomas common in men 19-26 yrs old may spread via bloodstream -teratomas rarely occur often mixed with other tumors -choriocarcinomas lethal, fast spreading initial dx often in metastatic stage -25%-teratocarcinomas b. stromal-hormone producing -interstitial cell tumors(arise from Leydig cells) ↑ androgenic hormone secretions rare, usually benign -androblastomas rare, usually benign may secrete estrogen-feminization gynecomastia 19 3. Causes a. mainly unknown b. may be R/T cryptorchidism -if develops CA, 75% will be in the undescended testis (assoc. with seminomas) c. may be R/T trauma, infection 4. Testing a. tumor marker study -benign tumors never elevate marker proteins -AFP and HCG-for nonseminoma -in seminomas-↑ hCG/LDH but not AFP if ↑ AFP, think mixed tumor-diff. Tx -if tx effective, markers should fall b. CT scan, U/S c. Chest x-ray to r/o metastasis d. lymphangiography to ck retroperitoneal lymph nodes 5. Physical exam a. palpate for lump b. may see painless enlargement c. heaviness, dragging sensation d. dull ache in abdomen, inguinal 6. Nursing diagnosis a. risk for sexual dysfunction R/T disease/surgery b. dysfunctional/anticipatory grieving c. disturbance of body image R/T dx and tx d. acute/chronic pain e. anxiety R/T dx of cancer 7. Management a. sperm banking-before radiation and chemo b. chemo c. radiation-seminomas -used after orchiectomy -external beam therapy →nonseminomas-radical lymph node dissection saves sympathetic ganglia d. stem cell transplantation-used with chemo to help prevent infection/anemia e. unilateral orchiectomy f. radical retroperitoneal lymph node dissection -helps to stage the disease and reduce tumor 8. Post-op teaching a. watch for fever, chills, increasing tenderness, pain around the incision, drainage, or dehiscence of the incision 20 b. c. d. B. no stair climbing or heavy lifting (>20 lbs) resume normal activities 1 week after discharge needs follow-up studies/TSE Other Reproductive Disorders 1. Hydrocele a. cystic mass with straw-colored fluid forming around the testis b. disorder of lymphatic drainage of scrotum c. no tx necessary unless compromises testis circulation d. aspirated or surgically removed e. may need surgical drain and hospitalization f. directed to wear scrotal support 2. Spermatocele a. sperm-containing cystic mass on the epididymus alongside the testicle b. usually small/asymptomatic-no intervention c. may be excised thru small incision in scrotum 3. Varicocele a. cluster of dilated veins posterior/above testis b. uni or bilateral c. usually asymptomatic-no tx d. if painful-surgically removed -inguinal incision -may need to elevate scrotum with towel when in bed to help with drainage e. can cause infertility by ↑ scrotal temperature 4. Scrotal trauma a. torsion of testes-twisting of spermatic cord -considered a surgical emergency -S & S-pain, N & V b. ice, elevate, avoid heavy lifting, scrotal support Cryptorchidism a. undescended testis b. mainly a pediatric problem -3% full term males -20% male premies c. 80% will spontaneously descend d. orchidopexy-surgical placement of testis into the scrotum 5. 6. Cancer of the Penis a. less than 1% of male malignancies b. carcinoma is a painless, wartlike growth/ulcer c. small areas may be excised or cured with radiation d. penectomy-partial (glans only) or total -with total-need a perineal urethrotomy for urinary drainage 21 7. Phimosis a. prepuce constricted-can’t retract over glans b. tx-circumcision 8. Priapism a. uncontrolled, prolonged erection b. penis remains large, hard, and becomes painful c. causes -neurological -vascular -pharmacological d. urologic emergency e. need to improve venous drainage to corpora cavernosa f. tx: Demerol, warm enemas, catheter, aspiration of corpora cavernosa 9. Epididymitis a. infection of the epididymis-tx with abx b. may come from infection of the prostate c. men under 35 yrs, chlamydia trachomatis d. c/o pain along inguinal canal and vas deferens e. may have pain and swelling of the scrotum f. if untreated, pyuria and bacteriuria may develop g. abscess may form necessitating an orchiectomy 10. Orchitis a. acute testicular inflammation b. results from infection or trauma c. caused by bacteria from urethra or other sources d. may be uni or bilateral e. risk for sterility R/T testicular atrophy f. tx: bedrest, scrotal elevation, ice, analgesics, and antibiotics g. mumps orchitis-20% of males who have mumps after puberty-given gamma globulins -childhood vaccination is a good preventative measure 11. Prostatitis a. may be bacterial or abacterial (more common) b. abacterial-after a viral illness or assoc. with STI -also called prostatodynia c. bacterial-assoc. with urethritis -common bad guys-E. coli, Proteus, Enterobacter and group D streptococci -S & S-fever, chills, dysuria, urethral discharge, and boggy, tender prostate d. can lead to inflammation of the bladder and epididymus e. sexual dysfunction may occur R/T pain 22 f. g. h. i. j. tx: antimicrobials-Geocillin, Cipro encourage sitz baths and completion of meds use analgesics prn if UTI develops, may be put on Septra instructions on activities to drain prostate -sexual activities -masturbation -prostatic massage 01/16