Internship Handbook
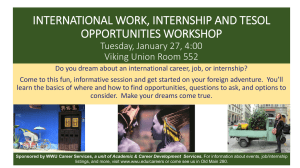
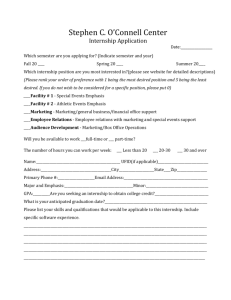
advertisement

Communication Disorders Internship Manual • Educational/Pediatric • Medical/Adult Purpose: The purpose of this handbook is to prepare graduate students, internship supervisors, and university liaisons for success in graduate internships through the Communication Disorders program of the Department of Speech, Hearing and Rehabilitation Services at Minnesota State University, Mankato. Questions or comments about this handbook or about the internship experience should be directed to the Director of Clinical Experiences: Jessica M. Jones, M.S., CCC-SLP Director of Clinical and Internship Experiences (DCIE) AH-103E MSU-Mankato Mankato, MN 56001 jessica.jones@mnsu.edu (507) 389-1414 (507) 389-2821 Links to Content (double click to link) Introduction Objectives Roles and Responsibilities Policies Getting Started The Internship Experience Supervisor’s Information Finishing Up Links to Appendices: Appendix A: Checklist Appendix B: Approval for Off-Campus Internships Appendix C: Application for Off-Campus Internships Appendix D: Site Description Appendix E: Consent for Background Check Appendix F: Health Statement Appendix G: Required Information About Internship Site Appendix H: Continuum of Supervision Appendix I: Session Feedback Appendix J: Feedback Guidelines Appendix K: Clinical Certification Board Interpretations Appendix L: Supervision Requirements Appendix M: Medical Setting Objectives Appendix N: Educational Setting Objectives Appendix O: Student Project Suggestions Appendix P: Student Internship Skills Evaluation Appendix Q: Internship Site Evaluation Form & Exit Questionnaire Appendix R: Complaint Procedure Appendix S: Medicare Ruling Appendix T: Internship Expectations Checklist Revised: September 2013 Introduction The graduate internship experiences represent the culmination of the master's degree program in Communication Disorders. Graduate students who have completed the appropriate coursework are eligible for an internship. Graduate students find and in some cases are assigned to internships in a variety of public school settings as well as a variety of acute and intermediate care facilities, residential rehabilitation facilities, day activity centers, birth to three programs and preschool programs, and private practice. Students may arrange to be in internships within a commuting distance of Mankato or in communities several hours from Mankato. A service agreement contract with the particular facility must be in place prior to a graduate student being placed in a facility. You are expected to sign up for a total of 12 semester credits of Internships, and to complete the full-time equivalent of internships in two separate sites in two separate terms. Typically a school setting is the first internship and a hospital or rehabilitation center the second. A typical internship during the academic year is for 14-15 weeks, depending on the schedule available at the Internship site. A school internship requires at least 50 days on-site and a minimum of 4 days/week. Students are expected to remain at their site for the entire term regardless of whether they have obtained the minimum clock hour requirements. Supplemental Internship - after completing the equivalent of 2 full time internships (12 semester credits), if you have more than 10 ASHA hours to complete, you may sign up for 1 semester credit. If you have 10 or fewer hours to complete, you may take an incomplete and we will work with you to finish up your hours appropriately. Often this means extending your full-time internship, with the onsite supervisor agreeing, until the hours are completed. Graduate Interns follow the calendar of the Internship Clinical Supervisors in the facilities in which they are placed. In some cases, interns may be working with more than one speech-language pathologist; however, one will be designated as the Primary Internship Clinical Supervisor. Typically, interns begin the internship with a brief orientation period followed by a gradual accumulation of the caseload of the Internship Clinical Supervisor. It is assumed that the intern will carry the entire caseload for the final few weeks of the internship. The intern is expected to follow the daily schedule of the Internship Clinical Supervisor and engage in the full range of clinical activities and meetings of the supervisor. In addition, supervisors may require additional responsibilities of the intern in the form of in-service presentations, case presentations, and/or research activities. Examples of these optional student projects are provided in Appendix O. Objectives The internship program provides graduate students in Communication Disorders the opportunity to gain professional, clinical experiences under the supervision of ASHA-certified speech-language pathologists. The primary objective to the internship in Communication Disorders is to provide practical application of theory in the professional clinical setting. Students and supervisors may wish to establish additional objectives for the internship experience (not required). The checklist below can be used to select preferred objectives. √ Objectives for All Settings To understand the organization and structure of rehabilitation and/or educational agencies, including the budgetary and reporting processes. To understand policies regarding the appropriate use and maintenance of patient/client files and records. To determine the adequacy of clinical and supervisory performance. To apply current technology to improve and maintain the quality of service delivery. To identify major characteristics of handicapping conditions as defined by state and federal laws. To explore various alternatives for providing the least restrictive environment for patients/clients/students with communication disorders or exceptional educational needs. To participate in screening, referral, multidisciplinary teams, & intervention program development. To select and apply individual assessment techniques used for identification and program planning decisions. To interpret results for intervention planning and programming for patients/clients/students and their families. To select and implement measurement strategies for monitoring progress of patients/clients/students within the intervention program priorities. To demonstrate methods of managing environments to maximize appropriate use of instructional techniques, materials, equipment, and computer technology. To identify, select, and interact with agencies and other community resources for improving the intervention programs for patients/clients/students. To develop communication skills enabling professionals jointly to plan, implement, and evaluate intervention programs with patients/clients/students, families and other professionals. To understand vocational considerations for patients/clients/students with communication disorders, and to address such considerations in program planning for individual patients/clients/students. To understand a wide variety of handicapping conditions and disabilities, and how those differ from differences, including cultural and dialectical variations. To increase skill in writing clinical reports. To increase understanding of the relationship between learning and cognitive/communication development. To understand and apply principles, procedures, and techniques of standardized testing and interpretation including principles related to validity, reliability, item analysis, and test bias. To become familiar with the billing procedures in the professional setting. √ Objectives for Educational Settings To understand curriculum & instructional approaches that contribute to the preparation of children for school. To study behavioral, cognitive, environmental, psychological, physical, and social models as applied to individual and group management strategies for students with communication disorders. To observe methods of teaching pupils with communication disorders in the regular classroom. To understand current issues relating to children at risk. To understand student service programs and their relationship to other aspects of the total school program. To understand legal, political, and economic aspects of education, including governance of education, policymaking and administration of the schools in the U.S. and the state. To understand methods & materials needed to evaluate & to report pupil progress, including the IEP process. To become familiar with school instructional media programs. To understand the roles and responsibilities of the school board, the school superintendent, principals, and teachers, as well as professional education organizations. To develop a perspective on the current trends in education in the U.S. and the state. Roles and Responsibilities Director of Clinical and Internship Experiences (DCIE) The Director of Clinical and Internship Experiences (DCIE) serves as the primary link between the Communication Disorders Program at MSU, Mankato, the Supervising Clinician, and the Graduate Intern. The DCIE is charged with the following responsibilities: • Prepares a Graduate Internship Handbook and updates it as needed. • Identifies potential internship sites for Graduate Interns and coordinates all internship placements by working with the Graduate Intern and the internship site. (Note: If you are interested in an internship outside of Minnesota, it may be necessary to assist with identifying an internship site.) • Is available during the academic school year to each Supervising Clinician and Graduate Intern for consultation on any concerns regarding a placement. • Conducts regular evaluations of Internship supervision and sites. • Moderates an online discussion for continuous contact with Graduate Interns. The DCIE will use this method for monitoring and information sharing of all interns each semester. Graduate Interns are expected to check in at least twice each week and respond to questions posted. • Facilitates contracts with internship sites. • Along with other department faculty, shares in the responsibility of visiting Internship sites. University faculty members are assigned to have at least one personal contact with the Graduate Intern and Supervising Clinician. This is usually done in a personal, onsite visit toward the end of the Internship. In rare cases, especially if the Internship site is not within 100 miles of MSU, Mankato, the visit will be done by telephone conversations. • Contacts the internship site by mail at the beginning and conclusion of each Internship experience. Offers the Supervising Clinician one MSU Communication Disorders Program CEU or appropriate therapy materials as a token of gratitude. Policies Eligibility for Internships Graduate Interns must have completed the appropriate coursework (see Appendix A), two successful (grade of B or better) on-campus speech clinics at the graduate level through the MSU, Mankato Speech-Language Pathology Clinic. It is anticipated that you will have successfully completed your clinical experience on campus prior to an Internship. It is important to gain as much experience as you can in our clinic by getting started immediately with any client assigned. Any exception to this must be petitioned to the faculty. An internship and an MSU clinical practicum cannot be taken simultaneously. Generally a school-based (or child-focused) internship precedes an adult placement in a hospital or rehabilitation setting. Professional Liability Professional liability coverage is required of all Graduate Interns. This coverage protects the Intern against claims from third parties for personal injury or property damage caused while performing within the scope of duties as a Graduate Intern. You can obtain student professional liability insurance from the Business Office (2nd floor of the Administration Building). The policy is in effect from July 1 to July 1. If you are in a summer internship, that means you typically must renew your liability insurance. If you have current insurance that is valid throughout the internship, it is not necessary to purchase new insurance. Proof of current liability coverage must be on file in the Internship Coordinator's office prior to beginning any internship, and you must not provide any services without proof on file. Vaccinations Before beginning your Internship, all vaccinations must be current, including a vaccination series for Hepatitis B. Consider a "flu shot" prior to your internship. You are responsible to cover the costs of your vaccinations. Complete the Health Statement (Appendix F) and show it to the Internship Coordinator. You must also verify a current TB (Manteaux) Test. Background Studies The amended Minnesota Data Practices Act (1997) requires that you be informed that a background investigation will be conducted as part of your Clinical Internship placement process. This is required by many school districts and some hospital placements. The background investigation will include investigation of information contained in public records including criminal history record and data from other public records. Your internship placement may require this information for the purpose of determining your suitability as a clinician in their facility. The data requested from you are intended solely for screening purposes and will not be used in a discriminatory manner. You are not legally required to provide the requested information or to consent to the background investigation. Accordingly, you may choose to refuse to supply the requested information. If you refuse to provide the requested information or refuse to consent to the background investigation, your internship site may choose not to accept you. The information you provide on the Required Information form (Appendix G) will be provided to Minnesota State University, Mankato and Internship placements that require it. Only individuals who have a legitimate need to have access to the information will be allowed to facilitate and conduct the background investigation. Any data collected, used, or maintained about you is accessible to you, upon request, as provided by the Minnesota Governmental Data Practices Act. Attendance Graduate Interns are expected to follow the calendar, vacation dates, and building policies of the Internship site. Regular attendance is expected. Excessive absences for any reason should be brought to the attention of the Internship Coordinator at Minnesota State University, Mankato. Graduate Interns are expected to function as a regular staff member in terms of arrival and departure times. They are also expected to attend facility and/or organizational functions such as team meetings, staff meetings, in-service sessions, and conferences or staffings. In the event of the Supervising Clinician being absent due to illness or personal/professional leave, interns are advised to follow the direction of the Supervising Clinician. Interns as Substitute Employees Graduate Interns require direct supervision. Our guidelines specify that at least 25% of treatment sessions and 50% of evaluation sessions be directly supervised by the Supervising Clinician. In addition, someone who holds the Certificate of Clinical Competence must be on-site when the Graduate Intern is engaged in clinical activities. In the event of extended absences of a Supervising Clinician, arrangements must be made for a change in supervisor. The Communication Disorders Program cannot condone the use of Graduate Interns as substitute employees. Labor Disputes In the event that a work stoppage occurs in a facility where a Graduate Intern is placed, the interns are to be considered non-participants to either party involved. Do not cross picket lines or participate in any facility-related activities until the issues have been resolved or permission to resume activities has been granted. Notify the DCIE as soon as possible. It may be necessary to the Graduate Intern to complete the Internship experience in another facility. Precautions to Prevent Spread of Infectious Disease The following information is adapted from Beverly Bradley, HIV Infection and the School Setting: A Guide for School Nursing Practice. Kent: American School Health Association, 1990. Contact with bodily fluids presents a risk of infection with a variety of infectious agents. "Bodily fluids" includes blood, drainage from scrapes, cuts, and open lesions, urine, respiratory secretions (e.g. nasal discharge) and saliva. UNIVERSAL PRECAUTIONS as itemized below will help protect you for infectious diseases during your internship. Your internship site may have training or materials for you to read before you begin your Internship. You are expected to follow the guidelines that are in place at your internship site. Skin Contact • Wash hands with soap and warm running water at regular times during the workday. Common infectious diseases (excluding HIV infection, AIDS and hepatitis B) may be contracted from dirt and waste encountered in the workplace. It is important to use warm running water and a circular motion and friction for 10 seconds when washing hands. If any contact is made with bodily fluids, hands and other affected areas should be washed immediately. Proper hand washing requires the use of soap and water and vigorous washing under a stream of running water for 10 seconds. Use paper towels to dry hands. • Handle discharges from another person's body with disposable gloves and wash hands thoroughly with soap and running water when you are finished. Gloves used for this purpose should be put in a plastic bag or lined trashcan, secured, and disposed of daily. If gloves aren't readily available, avoid touching the bodily fluid or at minimum, place some type of barrier between you and the other person's discharge. A barrier may be an article of clothing, towel, or several tissues. • Avoid punctures with objects that may contain blood of others. Equipment Surfaces • Clean surfaces contaminated by body fluids with soap and water and followed with an Environmental Protection Agency (EPA) approved disinfectant or a 1:10 solution of household bleach and water. (This solution should be fresh daily to assure proper strength). • Sanitary absorbent agents can be used to clean up spills. Apply the dry material to the area, leave for a few minutes to absorb the fluid and then vacuum or sweep it up. The vacuum bag or sweepings should be disposed of in a plastic bag. Non-disposable cleaning equipment (broom, dust pan, mop, pail) should be thoroughly rinsed in the disinfectant (bleach solution). Disposable cleaning equipment and gloves should be placed in a plastic bag and sealed. Disinfectant solution should be promptly disposed down a drainpipe. Disposal Procedures • Carefully dispose of trash that contains bodily discharges and sharp objects. Use special containers with plastic liners for disposal or refuse that contains bodily discharges. • Disposed of sharp objects in containers that cannot be broken or penetrated. Do not bend, break, or recap needles. Removal of Graduate Student Interns The Department of Speech, Hearing, and Rehabilitation Services recognizes the right of the cooperating internship facility and the university to terminate a Graduate Intern's participation in an Internship. The Communication Disorders Program may remove a Graduate Intern from an internship placement if participation in the experience is judged by the Supervising Clinician, the participating facility, or the DCIE to affect adversely the students, patients, or clients served in the facility or the Graduate Intern. When a situation is such that removal or termination is being considered, the following procedures should be followed: • The DCIE or Department Chair shall make a preliminary evaluation of the reliability of the information available, making further inquiries as circumstances necessitate. • Once information is obtained suggesting a need to remove a student from placement, the DCIE or Department Chair will notify the Supervising Clinician, the Graduate Intern, and the facility that removal is imminent. Each individual involved will have an opportunity to respond to concerns. • If all reasonable efforts to notify the Graduate Intern are unsuccessful, the student may be removed without notice; however, attempts to notify the Graduate Intern shall continue, and the intern shall be afforded an opportunity to be heard informally at the earliest opportunity. • A Graduate Intern who has been removed from an internship placement by the DCIE or Department Chair may appeal that decision to the faculty of the Communication Disorders program through the Student Complaint Policy. (Appendix R ) Getting Started Graduate Interns must have completed appropriate coursework, required on-campus clinical practicum, a background check, required vaccinations, and proof of liability insurance as well as completing the required forms (see checklist, Appendix A) prior to registration for an Internship. The Placement Process Do not contact any site without first discussing it with the DCIE. Arrangements for the placement of interns are made between the university, the student intern, and the internship site. The DCIE will make all initial contacts for students planning internships in Minnesota. The student must receive prior approval from the department to take part in the internship experience. The first step is to fill out all of your coursework on an Application for Off-Campus Practicum (Internship) form (Appendix C) and meet with your graduate advisor to determine that you will have completed the required course work prior to placement and to determine the type of sites suitable for your needs. Your advisor will sign the Off-Campus Practicum Approval Form (Appendix B). The Clinic Director, verifying that you have completed on-campus clinic sufficiently to be eligible for an internship, must also sign this form. Only after you have completed these steps should you meet with the DCIE to start discussing potential internship sites. The Internship Coordinator will help you brainstorm potential settings and review with you the appropriate forms that must be completed prior to placement. Note: You need to be flexible in where you will go. The Internship Coordinator maintains a list of several places that have accepted our interns in the past, and will suggest places for you. However, if you want a specific area outside of Minnesota, you may have to do searching on your own, and you may or may not be successful in finding a placement. You may need to contact several places before you find a spot. Our practice is that your first internship should be in a child setting (preferably in a school setting) and the second in an adult setting (usually a hospital or rehabilitation company). Most adult settings require that you have completed one internship before they will consider an intern. Most students seek placements in Minnesota, but we have been successful in placing interns out of state as well. Although there are some placements that are driving distance from Mankato, you may have to re-locate for an adult internship. Once you have received permission from the Internship Coordinator to contact a site, cover these points in your initial telephone contact: • Your name • That you are a graduate student in speech-language pathology at MSU, Mankato • That you have completed all the required coursework and practicum experience for an (school/hospital/rehabilitation setting) internship placement. • The student may need to go out to interview at the sites of interest. Application for Off-Campus Practicum (Internship) should be completed before going out for an interview. Discuss with your supervisor in the interview or at the beginning of your internship, what kind of hours you hope to obtain in this internship. • Before your internship begins, you may need to find and assume financial responsibility for housing and/or transportation to the internship site. • Submit a schedule by email for the internship, including days on site, starting and ending dates, contact information for the Intern and the Supervising Clinician, and the Supervising Clinician(s) ASHA number(s). (Appendix G) • Show the Internship Coordinator that you have filled out Student Rating-Initial column of the Student Internship Skills Evaluation (Appendix P) that must be completed prior to beginning your internship. The Internship Experience Work Load The Graduate Intern is expected to assume more responsibility throughout the Internship experiences and eventually assume the full caseload and professional obligations of the Supervising Clinician. The workload of the Graduate Intern should consist of the full range of activities for which the Supervising Clinician is responsible. These activities may include: • screening, identifying, assessing and interpreting, diagnosing, rehabilitating, and preventing disorders of speech (e.g., articulation, fluency, voice), language, cognitive, oral-pharyngeal function (e.g., dysphagia), and related disorders. • assessing, selecting and developing augmentative and alternative communication systems and providing training in their use. • enhancing speech-language proficiency and communication effectiveness (e.g., accent reduction). • screening of hearing and other factors for the purpose of speech-language evaluation and/or the initial identification of individuals with other communication disorders • providing aural rehabilitation and related counseling services to individuals with hearing impairment and their families. • documenting services and learning about billing for services. Clinical Clock Hours It is expected that students will earn a minimum of 50 clock hours in each of three separate sites. Additional hours may be necessary to fulfill disorder type, clinical activity, or age group requirements. Graduate Interns may find it necessary to register for "supplemental internships" after the two required internships are completed in order to acquire the required clock hours. Only direct contact hours with the client and/or family present may be counted. If you participate in a team meeting, only portions where you are contributing can be counted. Diagnostic and therapy planning, report writing, and so forth are part of an internship’s responsibility, but cannot be counted toward ASHA clock hours. The following clock hour standards are set by ASHA and are in effect for students applying for certification after January 2005. Graduate Intern Responsibilities during Internship The Graduate Intern is expected to fulfill the following responsibilities during the Internship: • Report to the Internship facility at the designated time each day and remain on site for the workday of the Supervising Clinician. • • • • Prepare for clinical activities as specified by the Supervising Clinician. Participate in clinical activities as specified by the Supervising Clinician. Assist with making entries in logs/charts of individuals with whom the Graduate Intern in involved. Attend and participate in staffings for individuals with whom the Graduate Intern is involved in providing evaluation or treatment services at the Internship site. • Maintain client confidentiality in all matters. • Establish and maintain an effective working relationship with the Supervising Clinician. • Attend and participate in the in-service and other continuing education programs that are made available for the professional staff members of the Internship site. • • • • Actively participate in the Minnesota State University, Mankato online discussions at least a twice a week. Keep accurate clock hour records. (The DCIE will provide the spreadsheets for you to use). Participate in a mid-term and final evaluation with the Supervising Clinician. (Appendix P) Fulfill any additional responsibilities as required by the Supervising Clinician. Information for the Supervising Clinician(s) The site must be willing to provide for appropriate supervision by an ASHA-certified professional who has a minimum of two years of experience. Only an individual holding a current ASHA Certificate of Clinical Competence in speechlanguage pathology is eligible to supervise a Graduate Intern. The Supervising Clinician's certification must remain current throughout the internship. The Supervising Clinician must have personal and direct involvement with the Graduate Intern during the internship. Supervision must include direct observation of diagnostic and treatment procedures. The Supervising Clinician may wish to review ASHA's Position Statement regarding Clinical Supervision in SpeechLanguage Pathology and Audiology. Supervisors in a setting that has Medicare Part B services should review ASHA’s statement on Medicare Coverage of Students and Clinical Fellows: Speech-Language Pathology at: http://www.asha.org/practice/reimbursement/medicare/student_participation_slp/ Supervision varies according to the student's level of experience and competency in performing the tasks assigned; therefore, supervision may involve three different stages: (1) the Evaluation-Feedback Stage, (2) the Transitional Stage, and (3) the Self-Evaluation Stage. Appendix H contains a handout that discusses these stages in more detail. Having a clear understanding of the internship expectations is very important both for the student interns and their supervisors. "Suggested Objectives for Graduate Student Internships" for both schools (Appendix N) and medical settings (Appendix M) are provided, and supervisors may wish to use this as they discuss their expectations with the intern. Appendix O provides guidelines for a student project which can be included as part of the internship assignment at the discretion of the onsite supervisor. Appendix T may be used as a checklist of weekly expectations, if desired. The Supervising Clinician should be willing to provide goal setting and performance feedback throughout the internship experience. This requires two-way communication that allows both the Supervising Clinician and the Graduate Intern to share important information about the intern's performance of clinical activities. The Clinical Certification Board of the American Speech-Language and Hearing Association suggests "a specific time should be set aside for each performance feedback session." These sessions should be used to identify performance strengths and weaknesses and, through discussions and goal-setting, to assist the Graduate Intern in developing skills necessary for success in the internship setting. Guidelines for Providing Feedback to Students (Appendix J) as well as an outline for a Supervised Therapy Session (Appendix I) may assist in this process. Supervising Clinician Responsibilities during the Internship: • Review ASHA's Clinical Certification Board Interpretations (Appendix K) regarding who may supervise and how to count treatment and evaluation clock hours. • Meet the minimum guidelines for supervision established by the American Speech-Language and Hearing Association. (Appendix L) This includes direct supervision of at least 25% of treatment sessions and 50% of evaluation sessions. • Coordinate the Graduate Intern's clinical experiences by preparing a plan of observation and experiences to move the Graduate Intern from entry-level proficiency to a higher level. • Introduce the Graduate Intern to the specific type of employment setting and to the specific internship site. Explain the lines of communication and the administrative organization of your facility. • Provide appropriate guidance and direction for improvement of the performance of the Graduate Intern. • Serve as a resource person to the Graduate Intern. • Help the Graduate Intern become familiar with your policies regarding data collection, criteria, and other relevant information. • Review your procedures and format for report writing. Discuss your specific expectations, frequency, and type of reports and lesson plans at the beginning of the internship. All reports written by the Graduate Intern should be approved by the Supervising Clinician and countersigned. • Instruct the student to be responsible for complying with procedures for legal, ethical, regulatory, and confidentiality aspects of professional practice. • Explain the fees charged for services, billing procedures, and budget issues. • Assist the Graduate Intern in developing and refining evaluation skills. • • • • • • • Assist the Graduate Intern in developing clinical goals and objectives for clients. • • • • • Assist the Graduate Intern in self-evaluation of clinical performance. Assist the Graduate Intern in developing and refining clinical management skills. Assist the Graduate Intern in observing and analyzing evaluation and treatment sessions. Interact with the Graduate Intern in planning, executing, and analyzing goal-setting and feedback conferences. Encourage the student to consult and collaborate with other professionals. Inform the student of required reading, special projects, or in-service requirements of your facility. Evaluate the Graduate Intern's clinical performance on an ongoing basis and keep the Graduate Intern informed about expectations and his/her performance. (Appendix P) Assist the Graduate Intern in developing skills of verbal reporting, writing, and editing. Share information regarding clinical, legal, regulatory, and reimbursement aspects of professional practice. Model and facilitate effective clinical practice and professional conduct. Communicate any major concerns to the Internship Coordinator or Department Chair. Finishing Up √ Student Responsibilities Checklist Submit signed records of accumulated clock hours to the Internship Coordinator. Evaluate the Internship experience and placement on the form provided (Appendix R) and return to the Internship Coordinator. Write a thank you letter to the Supervising Clinician. √ Supervisor’s Responsibilities Checklist Provide the Graduate Intern with a written evaluation of clinical performance and review this evaluation with the Graduate Intern prior to completion of the internship. (Appendix P and Appendix T) Initial the summary of clinical clock hours earned verifying the hours claimed by the Graduate Intern and return to the Graduate Intern. Submit a "satisfactory" or "unsatisfactory" grade for the Graduate Intern to the department chair. APPENDIX A Checklist for Internships (print and use as checklist) Task Complete the following courses prior to a child-based internship: • Language Therapy in Children • Naturalistic Language Evaluation • Seminar: Speech Sound Disorders • Organization & Management • Dysphagia • Augmentative/Alternative Comm. Complete the following courses prior to an adult-based internship: • Motor Speech Disorders • Organization & Management • Dysphagia Related Information Task Related Information • Augmentative/Alternative Comm. Complete at least 2 on-campus clinics with a grade of B or better through the MSU, Mankato Speech-Language Pathology Clinic Some students may be required to do an additional on-campus clinic prior to an internship. You must complete both on-campus graduate clinics prior to your internship unless the faculty approves a petition. You cannot do an internship and an MSU Clinical Practicum simultaneously. Have the Director of Clinical and Internship Experiences sign the appropriate section of the Off-Campus Approval Form (Appendix B) verifying you have met the minimum clinical standards for an internship placement. Determine with your graduate advisor, the type of sites suitable for your needs, along with verification that you will have completed the required coursework for the site selected by the time you start. Your graduate advisor should sign the top section of the OffCampus Practicum Approval Form (Appendix B). Meet with the DCIE to review necessary forms and possible sites. This should be done two or three semesters prior to beginning an internship. Internships are not allowed when faculty are not on duty (during semester breaks). Complete a background check. Fill out the form labeled Informed Consent for Background Check (Appendix E) and give it to the DCIE. Complete then Health Statement (Appendix F) and complete any missing vaccinations. Complete the Mantoux (TB skin test) less than one year prior to the end of the first internship. Note: Hepatitis B is required by most hospitals. WARNING: the Hepatitis B vaccination takes 3-6 months to complete. If you are currently not vaccinated, begin now. Consider obtaining or updating certification in First Aid/CPR. Some hospital sites require proof of certification within 2 years prior to beginning an internship site there. Provide DCIE with proof of liability insurance. You can use the same liability insurance used for on-campus clinics if it is still current. Insurance is available at the Cashier’s Office on the 1st floor of the Wigley Administrative Building. Ask for Student Professional Liability Insurance. Complete the Application for OffCampus Practicum (Appendix C). Provide one copy to the DCIE and retain the other for your files. Complete the Initial Student Rating column on the Student Internship Skills Evaluation form (Appendix P). This must be completed before the DCIE will give permission to register. The Student Internship Skills Evaluation is then given to your Internship site supervisor. Contact and interview with proposed site supervisor as appropriate to determine interest and appropriateness for your needs. The site supervisor must hold ASHA Certification. Read the ASHA Supervision Requirements (Appendix L). Task Related Information Complete Required Information About Internship Site form (Appendix G) and Site Description form (Appendix D). These must be signed by the DCIE for the Department Chair and placed in your student internship file. Obtain Permission to Register form (bottom of Appendix B) from the DCIE after all other forms have been returned. Register for CDIS 698. Give the permission form to the department administrative assistant who will register you). If you are not enrolled in class, clinical hours will not be credited. A typical internship during the academic year is for 14-15 weeks, depending on the schedule available at the internship site. A school internship requires at least 50 days on-site and a minimum or 4 days/week. Supplemental Internship: After completing the equivalent of 2 full-time internships (12 semester credits), if you have more than 10 ASHA hours to complete, you may sign up for 1 semester credit. Via email, provide the DCIE with the dates you are beginning and ending and the days you will be on site. Know how to access the threaded discussion (via D2L) associated with the internship experience). Optional: Set up a time to observe/shadow at your future internship. You are now ready to begin your internship experience. If any of the above is NOT completed prior to beginning your internship, any hours accrued will not be allowable until all the paperwork is in and in some cases, you may be prohibited from continuing the internship. At the midpoint of your internship, you and your internship site supervisor should complete the mid-term evaluation columns of your Student Internship Skills Evaluation form (Appendix P). At the end of the internship, have the site supervisor complete the final evaluation column of your Student Internship Skills Evaluation form (Appendix P) This form should be returned to the DCIE and will become part of your student file. Complete Internship Site Evaluation Form & Exit Questionnaire (Appendix Q). This form should be returned to the DCIE to help determine desirability of continued use of this site for other students. Complete Clock Hour Documentation and have the site supervisor sign them. Retain one copy for your records and return one copy to the DCIE. These clock hours will be entered into your permanent clock hour record by the department administrative assistant and will then be placed in your graduate student file. Send a thank you letter to your cooperating clinician, as well as his/her immediate supervisor. No grade will be assigned until all paperwork is in. After everything is completed, the materials will be placed in your graduate student file. Appendix B Off-Campus Approval Form (Type information into boxes, print, & obtain signatures) ↓ enter information below ↓ Name: Today’s Date: Internship Setting (e.g., school, hospital) Semester for Internship: This student will have completed the required coursework prior to the internship, has met with me and discussed appropriate types of Internship placements. _________________________________________ (Graduate Advisor) This student has completed on-campus clinical practicum in a satisfactory manner and is prepared for an Internship. ________________________________________ (Clinic Director) -----------------------------------------------------------------Clip Here -------------------------------------------------------------Permission to Register for Internship Form (Type info. obtain signature, and present to Dept. Secretary) ↓ enter information below ↓ Semester for Internship: 4-digit course ID#: Student’s Name: Tech ID: This student has completed requirements to register for CDIS 698 _________________________________________________________ Signature of Internship Coordinator _________________________ Date Appendix C Application for Off-Campus Internships (type information into boxes & send via e-mail to DCIE) ↓ enter information below ↓ Proposed Time frame (semester & yr.): Name (last, first, middle): Student’s College Address/Phone: Student’s Home Address: Academic Information Undergraduate Degree (University/College & Yr.): Expected date of completion for Graduate Degree: Graduate credits earned to date: Date enrolled @ MSU-Mankato: Enter CDIS Courses Completed to Date Undergraduate Courses Course # Title Graduate Courses Course # Title Undergraduate Courses Course # Graduate Courses Title Course # Title Yes Have you completed the required courses to be placed in this Internship? (check one)→ No Practicum Site Information (if known) (agency name, address, phone): Enter Clock Hours Totals to date Clock Hour Category: Evaluation Either Treatment Adult Child Any Adult Child Any Any (Min) total (Min) total (Min) total (Min) total (Min) total (Min) total (Min) total Speech Articulation (5) (5) (5) (5) Fluency (5) Voice (5) Language Dysphagia (8) (10) (20) (10) (20) (10) Hearing (5) A/AC (10) TOTALS Total Child Hours: (80) Total Adult Hours: (80) Total Group Hours: (25) Total Grad. Hours: (325) Grand Total Hours -400 List the areas in which you feel most competent (e.g., artic., lang., voice, fluency, A/AC, (etc.) Provide a summary of your clinical experience/competencies for each disorder classification (artic, language, voice, fluency, dysphagia, A/AC). For each disorder, estimate your level of skill for evaluation & treatment. List any specific tests or procedures you are familiar with. Check One: For each question below, check a box to the right. Yes Have you met the ASHA requirement of 25 clock hours of practicum (speech and language only -- do not include audiology hours) supervised by a regular member(s) of the Communication Disorders faculty? Will you have completed all required vaccinations and tuberculin tests before the start of your Internship? Do you have a current First Aid/CPR certification? (required for some sites) Have you provided evidence of current liability coverage? Have you completed a background check? Will you have a car available for use during this practicum? Applicant’s electronic signature (enter name): -- For Office Use Only -Internship Coordinator’s Signature: No APPENDIX D Site Description Form (Type or write information boxes & submit to Internship Coordinator) Name of Facility: Category: Average number of clients per week Evaluation Children Speech Language Hearing Voice Fluency Dysphagia Modalities Cognitive Social/Behavioral Aspects of Comm. Screening (Sp. & Lang.) Screening (Hearing) Treatment Speech Language Hearing Voice Fluency Dysphagia Modalities Cognitive Adults Total Social/Behavioral Aspects of Comm. Age Range for Adults: Age Range for Children: Appendix E Informed Consent for Background Check Minnesota State University, Mankato Department of Speech, Hearing & Rehabilitation Services (Type info. in boxes, sign, and submit to Internship Coordinator) Date: The following named individual has made application with Minnesota State University, Mankato for Graduate Internship. Last Name: First Name: Maiden, Alias, or Former: Date of Birth (M/D/Y): Social Security Number : Phone Number : Sex: Note: Background checks are valid for one calendar year. I authorize the Minnesota Bureau of Criminal Apprehension to disclose all criminal history record information to the Department of Speech, Hearing & Rehabilitation Services, Minnesota State University, Mankato and to any public or private agency where the applicant has made application for the purpose of clinical and/or educational speech/language pathology service provision. This releases the aforesaid parties from any liability and responsibility for collecting the above information. I understand that this report may contain negative information about background, character, and personal reputation and will be used solely for the purposes of placement. I also understand that providing false and/or incorrect information will result in dismissal from clinical and student teaching field experiences. The expiration of this authorization shall be no longer than one year from the date of my signature. Signature of Applicant (enter name for electronic permission): By entering my name in the box above, I hereby provide my electronic signature Note: The background check is nontransferable and cannot be obtained or used for academic purposes other than internship experiences. Appendix F HEALTH STATEMENT Minnesota State University Communication Disorders - Internship Minnesota Law (M.S. 135A.14) requires that all students born after 1956 and enrolled in a public or private post-secondary school in Minnesota be immunized against diphtheria, tetanus, measles, mumps, and rubella, allowing for certain specified exemptions. Students who have graduated from a Minnesota High School in 1997 or after are in compliance with the state law and do not need to submit the immunization information to MSU. This for is designed to provide the school with the information required by the law and will be review by the Minnesota Department of Health and local community health board. INSTRUCTIONS: Enter the month, day (if available), and year of the most recent “booster” for diphtheria and tetanus and for measles, mumps, and rubella. M/D/Y of last “booster” Vaccine Measles (rubeola, red measles) (must be at least 12 months after birth or be repeated) Mumps (must be at least 12 months after birth or be repeated) Rubella (German measles) (must be at least 12 months after birth or be repeated) Diphtheria & Tetanus (Td) (must be within last 10 years of current month/year or be repeated) Please check all true statements below: √ Statement I have had chicken pox, or been vaccinated against it. I have completed vaccinations for Hepatitis B I have completed a Manteaux test within the past year. Date:_________________________________________ I have read information/received CDIS training about General Infection Control outlines in the OSHA Blood borne Pathogens Standard (standard/universal precautions, signs/symptoms, practices to prevent transmission, etc.) For the student: I certify that the above information is a true and accurate statement of the dates on which I received the immunizations required by Minnesota law. Student’s electronic signature (enter name in box below): Date: Students wishing to file an exemption to any or all of the required immunization must complete the following: Conscientious Exemption (print & complete if used) I hereby certify by notarization that immunization against_______________________________ is contrary to my conscientiously held beliefs. Student’s Signature ___________________________________________ Date_________________ Subscribed and sworn before me on the _________________ day of _____________________20_________ Signature of Notary________________________________________ Date___________________ Student’s electronic signature for exemption(s) (enter name in box below): Date: Appendix G Required Information About Internship Site Minnesota State University, Mankato Communication Disorders (Type information in boxes and submit) Student Information Name: Address: E-mail: Site & Supervisor Information Site Name: Supervisor: Supervisor’s ASHA #: MN Dept. of Ed. &/or Dept. of Health #: Address: Phone: Schedule Information Beginning Date: Ending Date: Days & Hrs. on site: Student Information Appendix H Continuum of Supervision Taken from Anderson, J. (1988) The Supervisory Process in Speech-Language Pathology. Boston: College Hill (Little Brown). The Continuum of Supervision and Appropriate Styles The 13 tasks of supervision and their related competencies provide a comprehensive description of what it is that supervisors need to do. Even so, the ways in which they carry out the tasks and demonstrate the competencies will vary substantially from one supervisee to another. Some supervisees need more assistance than others Consider Task 2 as an example: assisting the supervisee in developing clinical goals and objectives. The kind of assistance needed by a student in the first clinical practice obviously differs from that needed by a clinician with many years of work experience. And yet, even the most experienced clinician faces situations in which some type of assistance is necessary. Furthermore, throughout their professional careers, supervisors have different expectations as well as different needs from supervision. Anderson (1099, p. 50) provided a framework to account for these differences with a 3-stage continuum of supervision, shown below. Please refer to her text for a comprehensive discussion. Evaluation Feedback Transitional Stage SelfSupervision Stage The Evaluation-Feedback Stage. In this stage, the supervisor provides direction, evaluation, and feedback; the supervisee functions, largely as a receiver of information. Beginning students, for example, expect and need explicit instruction about what to do and how to do it, along with direct feedback about what was accomplished and how well it was done. Anderson said that in this stage, supervisors use a direct-active style while supervisees employ a passive style (1988, p. 53). She emphasizes (p. 52) that the aim for both supervisor and supervisee is to leave this stage as rapidly as possible to a point further along on the continuum. The Transitional Stage. This is a stage where shared responsibility begins and shifts gradually from the supervisor to the supervisee for all aspects of the interaction. The supervisee shows emerging competence. The supervisor is able to recognize the increasing knowledge and skill, and to facilitate and accept the supervisee’s growing ability to assume responsibility. A collaborative style is appropriate (Anderson, 1988, p. 57). Some direction and feedback may come from the supervisor, but the supervisee is an active participant and may assume the lead role in some instances. The Self-Supervision Stage. Here the supervisee assumes the dominant role and is accountable for effectiveness. The person is able to self-analyze accurately, and to both plan and implement changes based on the analysis. This is the level of independent functioning that is the goal of supervision. It is not synonymous with total expertise. Rather, persons in the self-supervision stage know when and how to ask for help and strategies for problem solving are well developed. All students do not achieve self-supervision by the end of their graduate program. In fact, it remains an “elusive goal” for some clinicians even after many years of work experience (Anderson, 1988, p.52). The appropriate style for this stage is the consultative style. Brasseur (1978, p. 2) characterized the consulting relationship when she said “the consultant helps the consultee to use his or her (own) knowledge, skills and expertise to solve a problem.” Anderson says it is “critical…that the supervisor recognizes and accepts the supervisee’s options, 3especially that of rejecting suggestions” (1988, p. 61). Stages of the continuum are not time bound. That is, although both supervisors and supervisees should expect to move through the stages in sequence, they may shift temporarily to either a less or more advanced stage for particular tasks or interactions. For example, some students make steady progress along the continuum, working well into the transitional stage for a particular clinical assignment, but with a new client or different supervisor, they may return to the evaluation-feedback stage. This is true particularly for some students when they begin an off-campus placement. Supervisees also may function at different points on the continuum for different tasks in managing even a single client. The supervisee who plans, administer, and interprets a test battery with skill and confidence, selects appropriate therapy targets and make appropriate recommendations, may need specific direction and feedback to counsel parents or provide programming suggestions to school personnel. Experienced clinicians, too, may shift back and forth on the continuum. An employee in the self-supervision stage and with special expertise in treating clients with fluency disorders, may function briefly in the evaluation-feedback stage when reassigned to manage persons with dysphasia. Along with changes in job responsibilities, illness and other personal problems are additional events that may cause a temporary shift on the continuum. The continuum describes supervisor behavior, as well as that of the supervisee. Supervisors use different skills and styles for different points on the continuum. It may be that many of out mismatches between supervisors and supervisees can be explained by failure to determine where on the continuum each is functioning. Only when both participants know where they are, can they jointly determine where they want to be and plan procedures to get there. With the concept of the continuum in place, we are better equipped to apply the tasks. Appendix I Supervised Therapy Session - Feedback Form (optional use) Date of session: Patient/Client: Activity/Task: Diagnosis: Were goals addressed? Were tasks modified Were activities based on patient adequately explained? response/need? Was feedback provided appropriately (schedule & type)? Y/N? Comment Y/N? Comment Y/N? Comment Y/N? Comment Y/N? Comment Y/N? Comment Y/N? Comment Y/N? Comment Y/N? Comment Y/N? Comment Y/N? Comment Y/N? Comment For the student: What could you do in the next session for this patient? What would you change for today’s session, if anything? (can be filled out independently or with your supervisor). ___________________________________________________________________________________________________________ ___________________________________________________________________________________________________________ ___________________________________________________________________________________________________________ ___________________________________________________________________________________________________________ ___________________________________________________________________________________________________________ _______________________ Appendix J Providing Feedback to Students: Guidelines for supervisors (Adapted from form used by Loma Linda University) The following information pertains to feedback given to students during the evaluation process. Positive feedback with specific observations, i.e., not simply saying that the student did a nice job. A common characteristic of students, especially beginning clinicians is that they are not sure of when they are doing something right. They need to be told specifically what they are doing well. Instructive feedback that includes rational. Telling students to do or not do something without rationale leaves them unable to know how to generalize to other situations. General positive statements that would build a student’s self-confidence; Use of underlining to impress a student that a point needs to be given attention and the change needs to occur soon. Overuse of underlining may serve to reduce the effectiveness. Provide cues in the feedback (see “Pix” in example 3) so that student immediately knows the portion of the session to which the comment pertains. Provide feedback on how the patient is responding, both during the session and in comparison to the last session since students may not be skilled enough to identify clinically significant changes in behaviors. Outline specific procedures to be followed that will serve as a good reference to help the student remember the steps for late sessions. Ask questions that will require students to review course content and use the observation form for follow-up discussion. Provide rational for what you suggest to the student, which will help, students develop a more comprehensive understanding of the reasons underlying therapeutic/diagnostic decisions. Comment on what the student needs to do to be more prepared for a session. Supervisors should let students know that the differences between a planned session and one that is created along the way are easily identified. Scheduling problems may demand spontaneity at times; however, the expectation is that careful thinking and preparation be done before the session, not during. EXAMPLES OF SUPERVISOR COMMENTS The following examples were collected from previous observation reports written to several students assigned at the Loma Linda University Medical Center. Although some terms are unique to that setting, the types of feedback provided to the student are appropriate for any site. In the examples, look for the types of feedback discussed n the previous page. Example 1 You established rapport nicely and incorporated patient’s interests that were good. Nice prompting and consistent reminders to monitor rate. Glad you re-explained rationales. Be careful to say, “I can’t understand you” only when you truly don’t. I think sometimes you were saying this when you just wanted him to be clearer. Very nicely done today! It certainly didn’t look like it was your first day. Example 2 This was a little trickier having family here. You did well. Response delays increased compared to last week. Because of delays, you need to be patient and wait for his response. You are seeing significant cognitive deficits. Be careful to keep your tallying discreet. Example 3 Pix – good explanation of rationale. You might have just reminded him to concentrate on “clear speech” as well. I might have had him describe the pix, w/o you seeing it so you can provide more naturalistic feedback. It’s hard to know whether it’s true work finding or decreased vocabulary secondary to ESL. He seems to have problems with logical reasoning, i.e., determining consequences of an action or what caused a problem. It was good you had him doing some “predicting” of “why.” You did well at cueing him to provide more information after he said “a lot of times.” Example 4 (note: a/c = auditory comprehension; v/e = verbal expression) Body parts – OK after imitation. Did well with trying cures. You can also provide function cues, as appropriate. You had done 2 a/c tasks in a row. Vary between v/e and a/c usually. Good, you were consistently using rhythm. Sometimes reinforcing in between messes her up. I would do: Say phrase simultaneously with rhythm (2-3x) with “again” in between Fade out your voice as she says it Shadow as she says it Then, “what do you?” patient says phrase. You should have a list of approximately 10 phrases ready to go, rather than making up as you go, and then repeating. You might have made use of pix/ or words. A/C – you could also use description cues to assist with increasing a/c. Example 5 (Note: ADLs = activities of daily living) Yes/no – make sure you know the answer. I don’t think it’s worth pushing specifics with him at least about T.V. Good you gave him choices with ADLs. You did better at waiting for a response. Except he was quite off the mark most of the time. Do you think using objects would have been any different? Example 6 Let me show you how I “score” intelligibility. You did well at modeling during your turn. Categories – he was doing well with these, but you might need to provide more structure. Retelling - +++++/+++--/+++++/+- 14/17 Nice pacing of reading. Help him recall if he’s omitting some major points. Did you notice how he was self-correcting at times? Example 7 Slow processing do you think? What did you notice about her performance level? I don’t know if you were stalling or providing decreased amount of information on purpose. Sometimes it seemed you were holding out a little too long. Were you challenging her enough do you think? You did better at explaining rationale. Example 8 Remember to provide periodic reminder to increase intelligibility. Hearing about her “life” make you appreciate what you have, right? Writing – I was intending to have her construct complete sentences. Notice this is R hemisphere damage, different form L, right? In what ways? Example 9 Y/N – Good that you said her name to alert her prior to asking questions. Focusing inconsistently. Good interaction of first time doing this. Remembering to provide direct instructions/rationale prior to task, even for this level of patient. Example 10 A/C – Good explanation of task, also provide rationale (increase your understanding/listening ability). Glad you read paragraph again to assist him with recall. When you are picking material for a/c tasks, you have to remember to find material that is novel, not relying so much on long-term memory. V/E – 45% accuracy. Nice job with providing model and picking up on the “rate” aspect. Remember the goal is for shorter sentences and trying to keep them about the same length. You were definitely trying to keep these more consistent at end. You provided good and appropriate feedback. Appendix K Clinical Certification Board Interpretations I. Persons who hold the CCC_SLP may supervise: A. Assessment, rehabilitation, and prevention of disorders of speech (e.g., articulation, fluency, voice) and language; B. Assessment and rehabilitation of cognitive/communication disorder; C. Assessment and rehabilitation of disorders of oral-pharyngeal function and related disorder; D. Assessment, selection, and development of augmentative and alternative communication systems and the provision of training for their use; E. Aural habilitative/rehabilitative services and related counseling services; F. Enhancement of speech-language proficiency and communication effectiveness (e.g., accent reduction); and. G. Pure tone air conduction hearing screening. II. Clinical Practicum Hours A. Direct supervised clinical practicum involves direct time spent in actual evaluation or treatment of clients who present communication disorders. B. Time spent with the client or caretaker giving information, counseling or training for a home program may be counted as direct contact time if the activities are directly related to evaluation and treatment. C. Ancillary activities such as writing lesson plans, scoring tests, transcribing language samples, and preparing D. E. treatment activities and materials may not be counted. Meetings with practicum supervisors may not be counted under the 25 clock hours for staff meetings. If a client presents communication disorders in two or more of the disorder categories, accumulated clock hours should be distributed among these categories according to the amount of treatment tie spent on each III. Evaluation Clock Hours A. Evaluation refers to those hours in screening, assessment, and diagnosis that are accomplished prior to the B. C. D. initiation of a treatment program. Evaluation shall include collection of relevant information regarding case history (past and present status, function), selection and administration of reliable evaluation procedures, interpretation of results and appropriate referrals for additional evaluation and/or treatment based on the evaluation. Clock hours devoted to counseling associated with the evaluation/diagnostic process may be counted in these categories. Hours to be counted in the evaluation category may also include a formal reevaluation. Periodic assessments during treatment are to be considered in the treatment category. Appendix L ASHA Supervision Requirements for Speech-Language Pathology The following guidelines must be used for supervision and for the counting of clock hours: Individuals who hold a current CCC in the area in which the practicum hours are being obtained must supervise all observation and clinical practicum hours. Only the supervisor who actually observes the student in a clinical session is permitted to verify the credit given to the student for the clinical practicum hours. Persons holding a CCC in speech-language pathology may supervise all speech-language pathology evaluation and treatment services, nondiagnostic audiologic screening for the purpose of performing a speech and/or language evaluation or for the purpose of initial identification of individuals with other communicative disorders, and aural habilitative and rehabilitative services. The welfare of the client served by the Graduate Intern must be protected. A person holding the appropriate ASHA CCCs must be available on site for consultation at all times when the student is providing clinical services. (Current means the clinical supervisor must hold certification at the time the supervision is provided.) Supervision of the clinical practicum must include direct observation, guidance, and feedback by the currently certified supervisor to facilitate development of the student's clinical competence. Persons who hold the CCC and appropriate state-level credentials in speech-language pathology may supervise: Assessment, rehabilitation, and prevention of disorders of speech (e.g., articulation, fluency, voice) and language; assessment and rehabilitation of cognitive/communication disorders; assessment and rehabilitation of disorders of oralpharyngeal function (dysphagia) and related disorders; assessment, selection, and development of augmentative and alternative communication systems and the provision of training for their use; aural habilitative/rehabilitative services and related counseling services; enhancement of speech-language proficiency and communication effectiveness (e.g., accent reduction); and pure tone air conduction hearing screening. Clock hours may be obtained from participation in staffings in which evaluation, treatment, and/or recommendations are discussed or formulated, but only with the client or family present. Direct supervised clinical practicum involves direct time spent in actual evaluation or treatment of clients who present communication disorders. Time spent with the client or caretaker giving information, counseling, or training for a home program may be counted as direct contact time if the activities are directly related to evaluation and treatment. Ancillary activities such as writing lesson plans, scoring tests, transcribing language samples, and preparing treatment activities and materials may not be counted. Meetings with practicum supervisors may not be counted under the 25 clock hours for staff meetings. Major decisions by the Graduate Intern regarding evaluation and management of a client must be implemented or communicated to the client only after approval by the supervisor holding ASHA certification. (Major decisions refer to such activities as feedback to the clients and their families with respect to diagnostic conclusions, referrals to allied professionals for additional evaluation, recommendations for trial use or purchase of a prosthetic device such as a hearing aid, termination of treatment, etc.) Evaluation Hours – Refers to those hours in screening, assessment, and diagnosis of language and speech disorders (articulation, fluency, voice, dysphagia) that are accomplished before the initiation of a treatment program. Hours to be counted in the evaluation category may also include a formal reevaluation. Clock hours devoted to counseling associated with the evaluation/diagnostic process may be counted in these categories. Periodic assessments during treatment are to be considered in the treatment category. The majority of evaluation hours in each category must be in areas other than in screening activities. At least 50% of each student's time in each diagnostic evaluation, including screening and identification, must be observed directly by a supervisor. Observations may take place on site or by closed-circuit television. In addition to observations, it is recommended that other means of evaluating performance--such as conferences, audio and video recordings, written evaluations, rating instruments, inspection of lesson plans, and written reports--be used in the supervisory process. Treatment Hours – For language and speech disorders (articulation, fluency, voice, dysphagia) refers to clinical management (including direct and indirect services), progress in monitoring activities, and counseling. Clock hours devoted to counseling associated with the treatment process may be counted in these categories. At least 25% of each student's total contact time with each client in clinical treatment must be observed directly by a supervisor. These are minimum requirements and should be adjusted upward if the student's level of competence and experience warrants. Observations may take place on site or by closed-circuit television. In addition to observations, it is recommended that other means of evaluating performance such as conferences, audio and video recordings, written evaluations, rating instruments, inspection of lesson plans and written reports be used in the supervisory process. If a client presents communication disorders in two or more of the disorder categories, accumulated clock hours should be distributed among these categories according to the amount of treatment time spent on each. For example, if a client with both articulation and language problems received 20 hours of treatment and approximately 75% of each treatment session was spent on articulation, the clinician should record credit for 15 hours of treatment for speech disorders and 5 hours of treatment for language disorders. Up to 20 clock hours in the major professional area may be in related disorders. Audiology Hours – Clinical experience may include screening, evaluation and/or treatment of children and adults with a variety of types and severities of hearing disorders. Treatment for hearing disorders refers to clinical management and counseling, including auditory training and speech reading, as well as speech and language services for those with hearing impairment. During the course of training, at the university and at internship sites, the student must accumulate a total of at least 20 clock hours must be in audiology. Appendix M Suggested Objectives for Graduate SLP Student Internship in a Medical Setting By the end of the internship, the graduate student should be able to: Administer a speech/language and/or cognitive battery to patients with a diagnosis of CVA, brain injury, or other neurological diagnosis. Write a comprehensive initial report to include background information, speech/language/cognitive diagnosis, prognosis, recommendations, and functional goals. Conduct individual and group therapy. Participate and report on initial assessment, progress, and discharge plans at team conference for acute rehabilitation patients. Conduct an oral peripheral exam, and assist with or conduct a bedside dysphagia evaluation. Observe and/or participate actively in the at least one video fluoroscopic evaluation and its interpretation. Give an in-service to the communication disorders staff or to rehabilitation staff. Be able to provide education to family members regarding speech/language/cognitive deficits. Learn the differential diagnosis between various speech/language/cognitive disorders within the neurological impaired population. Have some experience and general understanding of the differences between acute medical, acute rehabilitation, day treatment and outpatient therapy operations. Appendix N Suggested Objectives for A SLP Graduate Student Internship in an Educational Setting By the end of the internship, the graduate student should be able to: Select an appropriate battery of assessment tools for a referred child on the basis of referral information and preassessment observation. Administer formal and informal assessment tools appropriate to the age of the student and the anticipated area of communication impairment. Write a comprehensive assessment summary report according to procedural guidelines, and make recommendations for services according to State eligibility criteria. Write an IFSP or IEP for a child eligible for school speech services according to procedural guidelines, and with appropriate goal and objectives. Complete all other due-process paperwork within mandated time frames and according to procedural guidelines. Participate in team planning conferences for an eligible student. Conduct individual and group therapy sessions in which strategies are planned and modified to meet changing student needs, using feedback from the supervising clinician. Provide appropriate informal feedback on student progress to parents and other professionals. Write a periodic review for a student receiving school speech services. Demonstrate basic competencies for typical disorders of language, articulation, fluency, and voice. Demonstrate initiative in seeking information about low-incidence disorders that may require special skills. Appendix O Suggestion for Student Project Description: A student project, completed during the assignment, is presented to the disciplinary team at the end of the internship. During the student internship students develop or expand on a diagnostic method or treatment technique. The project is designed to be a learning experience that will enable the student to problem solve and, thus, to improve the clinical skills. The final project is duplicated for staff and the student to keep. The student has access to all hospital material and may be reimbursed for material that needs to be purchased. The clinical coordinator approves all purchases. Project Examples: Analysis of new diagnostic procedures/test material and adaptation to facility needs. Development of a home program with handout for patients and families. Teaching material for patients. Hierarchy of material for a specific deficit or diagnosis. Screening tools to be used for inpatients. Appendix P Minnesota State University-Mankato Department of Speech, Hearing, & Rehabilitation Services Communication Disorders Program: Speech/Language Pathology 103 Armstrong Hall Mankato, MN 56001 (507)389-1414 Student Internship Skills Evaluation: CDIS 698 Student Clinician:____________________________________________________ Semester/Yr:____________________________ Supervisor:___________________________________________________________ ASHA #___________________________________ Site:___________________________________________________________________ Rating Scale: NA = Not Applicable/Not addressed yet 1 = Needs 100% Assistance/Feedback: Inadequate (inability to make changes) 2 = Needs 75% Assistance/Feedback: Nominal (regularly needs specific direction/demonstration) 3 = Needs 50% Assistance/Feedback: Adequate (often needs some general direction/ demonstration) 4 = Needs 25% Assistance/Feedback: Good (needs occasional direction/demonstration) 5 = Independent with Minimal Assistance/Feedback: Excellent (takes initiative and performs effectively) Diagnostic Skills 1. Conducts a thorough chart review and client interview. 2. 2. Utilizes appropriate diagnostic instruments. 3. Student Supervisor Initial Midterm Mid-term Final 3. Effectively administers and records tests according to published guidelines. 4. Accurately interprets test results. 5. Makes appropriate prognosis and recommendations based on diagnostic results. 6. Effectively shares results and recommendations and answers questions appropriately. 7. Accurately administers and interprets informal diagnostic procedures. 8. Quickly learns and incorporates new tests or procedures suggested by supervisor. 9. Demonstrates ongoing evaluation of client’s skills, tasks, and materials. Comments:____________________________________________________________________________________________________________ _________________________________________________________________________________________________________________________ _________________________________________________________________________________________________________________________ _________________________________________________________________________________________________________________________ Treatment Skills Student Supervisor Initial Midterm Mid-term Final 1. Develops and writes appropriate long- and short-term objectives. 2. Sequences treatment to meets the client’s need and maximizes the client’s performance. 3. Utilizes a variety of appropriate materials. 4. Utilizes a variety of appropriate treatment techniques and tasks that are clearly related to goals. 5. Effectively manages treatment contingencies (e.g., reinforcement) and behavior. 6. Appropriately uses data collection methods. 7. Provides consistent and appropriate feedback to clients regarding results of treatment sessions and overall progress. 8. Actively involves client in treatment by training self-monitoring of skills, providing regular home assignments, etc. 9. Adapts treatment methods based on ongoing assessment of client’s needs and adjusts pacing when needed. Comments:____________________________________________________________________________________________________________ _________________________________________________________________________________________________________________________ _________________________________________________________________________________________________________________________ _________________________________________________________________________________________________________________________ Practicum/Internship as a Learning Experience Student Supervisor Initial Midterm Mid-term Final 1. Implements recommendations quickly. 2. Seeks clarification when in doubt. 3. Develops original and/or appropriate solutions to clinical problems. 4. Improves and learns as a result of experience and from supervisory suggestions. 5. Demonstrates careful planning and consideration of consequences. 6. Receives constructive suggestions without resistance. 7. Conducts on-going self-analysis to meet personal goals. 8. Demonstrates appropriate organizational skills. 9. Identifies areas of competencies and areas that need improvement (e.g., selfawareness) Comments:____________________________________________________________________________________________________________ _________________________________________________________________________________________________________________________ _________________________________________________________________________________________________________________________ _________________________________________________________________________________________________________________________ Writing Skills Student Supervisor Initial Midterm Mid-term Final 1. Prepares complete, well-organized reports and progress notes. 2. Submits written assignments in a timely manner. 3. Uses correct and appropriate grammar, form, style, and spelling in written reports. 4. Writes reports in a style appropriate to the reader. Comments:____________________________________________________________________________________________________________ _________________________________________________________________________________________________________________________ _________________________________________________________________________________________________________________________ _________________________________________________________________________________________________________________________ Professionalism & Ethics Student Supervisor Initial Midterm Mid-term Final 1. Communicates effectively using appropriate levels with a variety of individuals. 2. Establishes and maintains rapport with clients and professionals. 3. Complies with established clinic or on-site procedures. 4. Demonstrates knowledge of ASHA’s Code of Ethics by applying ethical standards in all professional settings 5. Maintains a professional appearance. 6. Attends and is on time for all meetings. 7. Treats all people with respect and safeguards confidentiality. 8. Demonstrates clinical confidence and independence. Comments:____________________________________________________________________________________________________________ _________________________________________________________________________________________________________________________ _________________________________________________________________________________________________________________________ _________________________________________________________________________________________________________________________ RECOMMENDED GRADE:___________ Supervisor Signature:_____________________________________________________ Date:_________________________________ Adapted from California State University-Fresno, Speech, Language, & Hearing Clinic’s Student Practicum Evaluation form Page Intentionally left blank Appendix Q Internship Site Evaluation Form & Exit Questionnaire (Enter info. and send to Internship Coordinator at end of internship) INSTRUCTIONS: Please answer all items below. All responses will be kept confidential. Evaluate your Clinical Supervisor on his/her ability. Please do this with careful thought. Future Interns will be placed with Clinical Supervisors based, in part, on your evaluation. Be careful not to let your relationship with the supervisor, either positive or negative, cloud your judgment as to his/her ability. Student’s Name: Name of Internship Site Primary Supervisor Did your supervisor meet the minimum guidelines for supervision established by ASHA (direct supervision of at least 25% of treatment sessions and 50% of evaluation sessions)? Yes No Yes No Yes No Would you recommend this Internship Site for another Intern? Would you recommend this Supervisor for another Intern? INSTRUCTIONS: Use the following ratings to indicate the degree to which your supervisor impacted your learning. Place an “X” in the appropriate column. 4 3 2 1 NA Very Helpful Helpful Neutral Detrimental Not applicable 4 3 2 1 NA Very Helpful Helpful Neutral Detrimental Not applicable Coordinated the Graduate Intern's clinical experiences by preparing a plan of observation and experiences to move the Graduate Intern from entry-level proficiency to a higher level. Introduced the Graduate Intern to the specific type of employment setting and to the specific Internship site. Explain the lines of communication and the administrative organization of the facility. Provided appropriate guidance and direction for improvement of the performance of the Graduate Intern. Served as a resource person to the Graduate Intern. Helped the Graduate Intern become familiar with policies regarding data collection, criteria, and other relevant information INSTRUCTIONS: Use the following ratings to indicate the degree to which your supervisor impacted your learning. Place an “X” in the appropriate column. Reviewed procedures and format for report writing. Discussed specific expectations, frequency and type of reports and lesson plans at the beginning of the Internship. Approved and countersigned all reports done by the Graduate Intern. Instructed the student to be responsible for complying with procedures for legal, ethical, regulatory, and confidentiality aspects of professional practice. Explained the fees charged for services, billing procedures, and budget issues Assisted the Graduate Intern in developing and refining evaluation skills. Assisted the Graduate Intern in developing clinical goals and objectives for clients. Assisted the Graduate Intern in developing and refining clinical management skills. Assisted the Graduate Intern in observing and analyzing evaluation and treatment sessions Interacted with the Graduate Intern in planning, executing, and analyzing goal-setting and feedback conferences. Encouraged the student to consult and collaborate with other professionals Informed the student of required reading, special projects, or in-service requirements of the facility. Evaluated the Graduate Intern's clinical performance on an ongoing basis and kept the Graduate Intern informed about expectations and his/her performance. Assisted the Graduate Intern in self-evaluation of clinical performance. Assisted the Graduate Intern in developing skills of verbal reporting, writing, and editing. Shared information regarding clinical, legal, regulatory, and reimbursement aspects of professional practice. Modeled and facilitated effective clinical practice and professional conduct. Please add any additional comments you may have: Appendix R MSU/Communication Disorders Student Complaint Procedure As part of the program’s accreditation by the ASHA Council on Academic Accreditation, the Communication Disorders program is required to maintain a student complaint process. Students who wish to resolve a complaint are directed to follow the CDIS student complaint procedure that is illustrated on the attached flow chart. The following information is provided to assist students in the process. As an initial step, the student should determine with whom the complaint should be discussed first. The student should judge whether the issue is related to clinic, an individual course, or whether it is a program-related issue. Clinical Issues: These may include, but are not limited to client assignments, supervision problems, clock hour issues, clinic paperwork, etc. Course Issues: These may include, but are not limited to class assignments, tests, grades, availability of instructor, etc. Please note: If a student complaint involves grades, the student is advised to follow the university procedure for grade appeal which is outlined in each course schedule book. CDIS Program Issues: These may include, but are not limited to admission decisions, removal from the program, curricular requirements, problems with the physical facilities, etc. Complaints of another nature may be covered by other university policies including discrimination and harassment which are outlined in the Graduate and Undergraduate Bulletins. CDIS Students have the right to file a complaint with the ASHA Council on Academic Accreditation (CAA). The CAA can be reached at (301) 571-5700. Should you wish to file a complaint, the contact information for the CAA is listed below. Council on Academic Accreditation American Speech-Language-Hearing Association 10801 Rockville Pike, Rockville, MD 20852 301-571-5700 (voice/TTY) 301-571-0457 (fax). Appendix S Documents Relating to Medicare Part B Rulings CMS Clarifies Student Participation in Medicare Part B Services by Arlene Pietranton, ASHA While at the ASHA Convention in New Orleans, ASHA President John Bernthal received a letter dated November 9, 2001, from the Centers for Medicare and Medicaid Services (CMS) clarifying that speech-language pathology and audiology students can participate in providing Medicare covered services to Part B beneficiaries. The CMS letter is being mailed to all program directors and can be found in pdf format on ASHA’s Web site, www.professional.ash.org/ resources/reimbursement/student_participation.cfm. Feel free to share it with clinical practicum site supervisors. The letter from Terrence L. Kay, director of the Division of Practitioner and Ambulatory Care in the Center for Medicare Management, requires the qualified practitioner be “…in the room guiding the student in service delivery when the graduate student is participating in the provision of services, and the practitioner is not engaged in treating another patient or doing other tasks at the same time.” Mr. Kay’s letter also states, “The qualified practitioner is responsible for the services and as such, signs all documentation.” He adds parenthetically that the student may also sign the documentation if desired. All six points for ensuring coverage of Medicare Part B when a graduate student is involved with service delivery must be followed. Mr. Kay included two scenarios, one for speech-language pathology services and one for audiology services, to illustrate Medicare Part B billable services. They are: A speech-language pathologist is seeing a Medicare Part B beneficiary who has aphasia. The speech-language pathologist, with the graduate student’s participation, develop a treatment plan for the session and both see the patient with the speech-language pathologist controlling the services rendered. The speech-language pathologist is in the room and engaged only in that patient’s treatment at all times. An audiologist is assessing the hearing of a Medicare Part B beneficiary who was referred because of hearing loss and vertigo. The graduate student participates in conducting the pure tone and speech audiometry. The audiologist is in the room and engaged only in that patient’s assessment at all times. ASHA is pleased that CMS has removed any doubt that speech-language pathology and audiology graduate students can participate in covered services rendered to Medicare Part B beneficiaries. For further or additional information, contact Mark Hobratschk through the Action Center at 800/498-2071, ext. 4482, or e-mail to mhobratschk@asha.org. DEPARTMENT OF HEALTH & HUMAN SERVICES Centers for Medicare and Medicaid Services 7500 Security Blvd., C4-03-06 Baltimore, MD 21244-1850 __________________________________________________________________________________________ John E. Bernthal, Ph.D. President American Speech-Language Hearing Association 10801 Rockville Pike Rockville, MD 20852 Dear Dr. Bernthal: This letter is a follow-up to recent discussions held with representatives of the American Speech-Language Association (ASHA) regarding Medicare physician payment policy for services involving students. Specifically, ASHA representatives asked for assurance that speech-language pathology and audiology graduate students can participate in providing covered services to Medicare Part B beneficiaries. More specifically, the following is a summary of our understanding of the typical scenario involving students for which speech-language pathologists and audiologists seek payment: Medicare Part B services are provided by practitioners who are acting within the scope of their state licensure requirements. Services are provided by an individual who is licensed in the state as a speech-language pathologist or audiologist or is certified by ASHA if there is no licensure in the state. The qualified practitioner (i.e., speech-language pathologist or audiologist) is recognized by the Medicare Part B beneficiary as the responsible professional within any session when services are delivered. The qualified practitioner is present and in the room for the entire session. The student participates in the delivery of services when the qualified practitioner is directing the service, making the skilled judgment, and is responsible for the assessment and treatment. The qualified practitioner is present in the room guiding the student in service delivery when the graduate student is participating in the provision of services, and the practitioner is not engaged in treating another patient or doing other tasks at the same time. The qualified practitioner is responsible for the services and as such, signs all documentation. (A student may, of course, also sign but it is not necessary since the Part B payment is for the clinician's services, not for the student's services). Appendix T MN State University-Mankato Speech-Language Pathology Internship Expectations The following checklist provides some loose guidelines of expectations for student interns as they progress through their internship experience. It is meant to give you a rough idea of the types of tasks and level of independence that is expected at each week of the internship. Please feel free to adjust these expectations according to your intern’s skill level. Student interns are still in the learning process and benefit from frequent feedback on their performance on a regular basis. We suggest at least one weekly meeting for this purpose with formal mid-term and final evaluations using the given evaluation rubric. We feel this is critical to the intern’s growth and success. Please remember that although it is the goal of the intern to conduct treatment sessions independently, there continue to be supervision requirements per ASHA, i.e., interns are expected to be directly supervised according to ASHA guidelines at all times. Week 1 Submit site required paperwork. Tour Site. Meet staff members and introduce yourself, as appropriate. Begin reviewing patient/client files (as appropriate) and take notes for treatment planning. Take notes while observing sessions (e.g., cues/materials used, skills/objectives addressed, behavior management strategies, etc.) and during conversations with SLP. Start reviewing diagnostic and treatment resources. Observe lesson planning done by the SLP. Participate in D2L discussion. Begin co-clinicianing sessions with the SLP towards the end of the week (begin counting clock hours NOW and keep current every day). Obtain at least 2 clinical hours by the end of the week. Week 2 Lead approximately 5 sessions selected the previous week (co-planned with the SLP). Continue to accompany SLP to the classroom to get students. Continue observing sessions lead by the SLP. Continue to co-clinician, participating in more and more sessions throughout the week. Continue reviewing files, reviewing materials, taking notes while observing sessions and while having conversations about students with the SLP. Participate in and observe planning done by the SLP. Select approximately 5 sessions to lead independently for the following week (however, the SLP may still assist with planning. Participate in D2L discussion. Have at least 10 hours accrued by the end of the 2 nd week. Week 3 . Lead the 5-10 sessions selected in the previous week (75-100% direct supervision suggested). Continue to co-clinician sessions Select approximately 50% of the SLP’s caseload to lead for the following week (SLP may continue to participate equally in the planning of these sessions). Indendently get students from classrooms for their assigned treatment sessions. Participate in D2L discussion. Continue to participate in and observe planning done by the SLP. Meet formally with the SLP and discuss your performance. Have at least 20 hours accrued by the end of the week. Week 4 Lead the sessions selected the previous week (75-100% direct supervision suggested). Continue to co-clinician sessions. Select approximately 50% of the clinician’s caseload to plan independently and lead for the following week. Work independently with approximately 75% of the caseload (although the SLP may still participate in planning some of the sessions. Participate in D2L discussion. Meet formally with the SLP to discuss your performance Have 30 hours accrued by the end of the week. Week 5 Select approximately 75% of the SLP’s caseload to plan independently and lead for the following week. Work independently with 75-100% of the caseload (although the SLP may still participate in planning some of these sessions (50-75% direct supervision suggested, as appropriate to intern’s skill level) Meet formally with the SLP to discuss your performance. Participate in D2L discussion. Have 40 hours accrued by the end of the week. Week 6 Lead the sessions selected the previous week (50-75% direct supervision suggested, as appropriate to the intern’s skills level). Select approximately 75-100% of the SLP’s caseload to plan independently and lead for the following week. Work independently with 100& of the caseload. Participate in D2L discussion. Meet formally with the SLP to discuss your performance. Meet formally with the SLP to discuss mid-term evaluation of performance using Student Internship Skills Evaluation form. Have 60 hours accrued by the end of the week. Week 7 Lead the sessions selected the previous week (25-50% direct supervision suggested, as appropriate to the intern’s skills level). Plan 100% of the treatment sessions for the following week. Meet formally with the SLP to discuss your performance. Participate in D2L discussion. Have 80 hours accrued by the end of the week. Week 8 Lead the sessions selected the previous week (25-50% direct supervision suggested, as appropriate to the intern’s skills level). Plan 100% of the treatment sessions for the following week. Participate in D2L discussion. Meet formally with the SLP to discuss your performance. Have 100 hours accrued by the end of the week. Week 9 Lead the sessions selected the previous week (25-50% direct supervision suggested, as appropriate to the intern’s skills level). Plan 100% of the treatment sessions for the following week. Participate in D2L discussion. Meet formally with the SLP to discuss your performance. Have 120 hours accrued by the end of the week. Week 10 Lead the sessions selected the previous week (25% direct supervision, as appropriate to the intern’s skills level). Plan 100% of the treatment sessions for the following week. Participate in D2L discussion. Meet formally with the SLP to discuss your performance. Have 140 hours accrued by the end of the week. Week 11 Lead the sessions selected the previous week (25% direct supervision, as appropriate to the intern’s skills level). Plan 100% of the treatment sessions for the following week. Participate in D2L discussion. Meet formally with the SLP to discuss your performance. Have 140 hours accrued by the end of the week. Week 12 Lead the sessions selected the previous week (25% direct supervision, as appropriate to the intern’s skills. Plan 100% of the treatment sessions for the following week. Participate in D2L discussion. Meet formally with the SLP to discuss your performance. Have 160 hours accrued by the end of the week. Final Week Lead the sessions selected the previous week. Say good-bye to students/staff Find a moment to express your thanks to the administrator for sponsoring your internship Participate in D2L discussion. Meet formally with the SLP to discuss final evaluation of performance using Student Internship Skills Evaluation form. Have SLP sign your Clock Hour Documentation form. Complete the Internship Site Evaluation Form and Exit Questionnaire. Request letters of recommendation (as appropriate). Send the following forms to the Director of Clinical and Internship Experiences: Student Internship Skills Evaluation form Clock Hour Documentation form Internship Site Evaluation and Exit Questionnaire Adapted from University of Wisconsin-Eau Claire, Sample Orientation and Practicum Expectations form