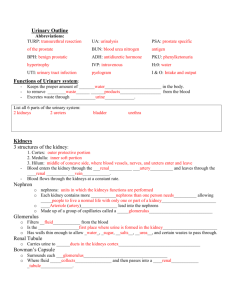
Anatomy of the Urinary System
advertisement

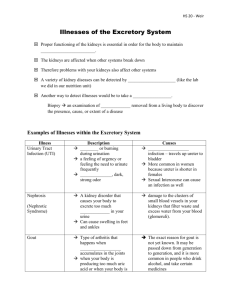
Anatomy of the Urinary System The kidneys are major homeostatic organs of the body. They function to remove nitrogenous wastes (from the breakdown of proteins), but they also maintain the electrolyte, acid-base, and fluid balances of the blood and, therefore, the interstitial and intracellular fluids indirectly. If functioning properly, the kidney must be able to get rid of urea, other metabolic wastes, and excess ions while hanging on to the water and other important molecules such as glucose. In this lab activity we will examine the kidneys of a pig, sheep, or cat to get a sense for what human kidneys are like. We will also look at some of the properties of urine and discover how medical laboratories test urine samples to help determine the level of health in patients. Part I - Gross Internal Anatomy of a Cat Kidney 1. The pair of kidneys is fairly easy to find in a preserved cat. The cat’s left kidney can be located by moving the spleen, stomach and intestine ventrally and medially to reveal the large beanshaped structure near the spinal column or by completely removing the digestive system of the cat. If the digestive system is not removed, the cat’s right kidney can be located by moving the liver and intestines ventrally and medially as well. Examine the location of the kidney. Notice the position of the peritoneum. The kidneys are positioned behind the peritoneum while most of the other abdominal organs are located within this lining. 2. Find the ureters on both sides and follow both of the tubes until they connect with the urinary bladder. The urinary bladder is often difficult to identify because it is empty. If possible, cut open the urinary bladder and look within it. See if you can find the 2 small ureteral openings and the opening to the urethra. 3. Return to the kidneys. Examine the surface of the kidney. You may see blood vessels that branch over the entire surface of the kidney. Recall that the kidney filters over 20% of the blood coming from the heart, so it is FULL of blood vessels. This is a major reason why a blow to the kidneys needs to be carefully watched. 4. Identify the hilus. This is the part of the kidney where the major blood vessels and the ureter enter or leave the kidney. Now identify the renal artery, the renal vein, and the ureter. The renal vein has the thinnest wall (collapsed) and joins with the posterior vena cava (inferior vena cava) in the cat. The ureter is the largest of the three and has the thickest wall. The renal artery branches off of the abdominal aorta. 5. Carefully cut the renal artery, the renal vein, and the ureter and remove the kidney from the cat. Make a longitudinal cut through the kidney with a sharp scalpel. The kidney of a cat does not contain clearly delineated pyramids like the human kidney. Identify the renal pelvis, medulla, cortex, calyces (singular = calyx) and capsule. a. The kidney cortex is lighter in color and should contain red and blue latex specks in this region. b. The medulla is darker and may have a somewhat striped appearance. c. The renal pelvis is a basin-like cavity can be found emptying into the ureter in the hilus region. d. The fingerlike extensions of the renal pelvis are called calyces. The calyces collect the urine that drains from the collecting tubules in the medulla. e. The renal capsule is a thin, tough layer found on the outside of the kidney. 6. If you were to look at the cortex under the microscope, it might look something like this (right). Identify some parts of the nephron such as the glomeruli and renal tubules. Part II - Urinalysis IMPORTANT! PLEASE READ! We will be testing and recording the characteristics of urine in this section of the lab. Because these are bodily fluids, it is important that you wear gloves and handle the urine specimens carefully. The equipment that comes in contact with the urine must be sterilized with 10% bleach solution when we are finished using it and all testing strips should be disposed of in the 10% solution as well. At the end of the lab, the remaining urine should be carefully poured down the drain by the person whose urine it is. The container is then to be put into the 10% bleach solution. In addition, all lab stations should be wiped down with 10% bleach solution at the end of this lab. There are multiple urine tests that are frequently run in hospital labs and clinics to help diagnose various conditions. For instance, you may be asked to give a urine sample if you have the symptoms for a bladder infection or if diabetes runs in your family. Some of these tests can even be done at home by purchasing testing strips at your local pharmacy. Normal urine samples should contain water (97%), urea, sodium ions, potassium ions, phosphate ions, sulfate ions, creatinine, and uric acid. Traces of calcium, magnesium, and bicarbonate ions should also be present. Substances that are not normally found in the urine are called abnormal urinary constituents and are indicators of a variety of ailments. The chart below lists the common abnormal urinary constituents and their possible causes. Abnormal Urinary Constituents Substance Glucose Name of Condition Glycosuria Ketone bodies Ketonuria Proteins Proteinuria or albuminuria Pus (WBCs and bacteria) RBCs Pyuria Hematuria Hemoglobin Bile pigments Hemoglobinuria Bilirubinuria Possible Causes Diabetes mellitus or possibly just an excessive intake of sugary foods Starvation; low carbohydrate diet; diabetes mellitus when couple with glycosuria Damage to glomeruli; hypertension; possibly even pregnancy or physical exertion Urinary tract infection Trauma, kidney stones, or infection in the urinary tract Hemolytic anemia; blood transfusion reaction Liver disease (hepatitis) Obtain a urine sample. Ideally this is done by first wiping the urethral opening with an alcohol wipe and then collecting urine while in mid-stream. Close your specimen jar and DISCRETELY carry your sample back to class. To determine specific gravity, carefully pour the urine into a urinometer until it is about 2/3 full. Insert the float and make sure it is freely floating. Read the stem of the float to three decimal places at the lower edge of the meniscus formed by the urine - air border. Following the directions for the test strips EXACTLY as they read, determine the levels of proteins, glucose, and ketones in your urine along with the pH. Record the results in the chart below. The normal values are also on the chart to compare your results to. Sources: Functional Anatomy of the Urinary System pp. 233-234 COLOR: Freshly voided urine is usually clear and pale to deep yellow in color. This normal yellow color is due to urochrome, a pigment arising from the body’s breakdown of hemoglobin. As a rule, the greater the solute concentration, the deeper the yellow color. Abnormal urine color may be due to certain foods, such as beets, various drugs, bile, blood, or other causes. Abnormal Appearance of Urine Color Likely cause yellow-green to brownish green bilirubin from obstructive jaundice red to red-brown hemoglobinuria smokey red unhemolyzed RBCs from urinary tract dark wine color hemolytic jaundice brown-black melanin pigment from melanoma dark brown liver infections, pernicious anemia, malaria green bacterial infection (Pseudomonas aeruginosa) ODOR: The odor of freshly voided urine is slightly aromatic, but bacterial action gives it an ammonia-like odor when left standing. Certain diseases may alter the characteristic odor of urine. For example, the urine of a person with uncontrolled diabetes mellitus (an elevated level of ketones) smells fruity, like acetone. pH: The pH of urine ranges from 4.5 to 8.0, but its average value, 6.0, is slightly acidic. Diet may markedly influence the pH of the urine. For example, a high-protein diet increases the acidity of urine, while a vegetarian diet increases the alkalinity of the urine. A bacterial infection of the urinary tract may also result in urine with a high pH. SPECIFIC GRAVITY: Specific gravity is the relative weight of a specific volume of liquid compared with an equal volume of distilled water. The specific gravity of distilled water is 1.000, because 1 ml weighs 1 g. Because urine contains dissolved solutes, it weighs more than water, and its customary specific gravity ranges from 1.001 to 1.030. Urine with a specific gravity of 1.001 contains few solutes and is very dilute. Dilute urine is common when a person drinks large amounts of water, uses diuretics, of suffers from chronic renal failure. Conditions that produce urine with a high specific gravity include limited fluid intake, fever, and kidney inflammation, called pyelonephritis. If urine becomes excessively concentrated, some of the solutes begin to precipitate or crystallize, forming kidney stones, or renal calculi. PROTEINS: Since proteins are very large molecules, they are not normally present in urine. The presence of protein in the urine may therefore indicate that the permeability of the glomerulus is abnormally increased. In other words, large molecules that are not normally supposed to get through the glomerulus are getting through. This may be caused by renal (kidney) infections or by other diseases that secondarily affect the kidneys, such as diabetes mellitus, jaundice, or hyperthyroidism. GLUCOSE: Although glucose is easily filtered by the glomerulus, it is not normally present in the urine because all of the filtered glucose should be reabsorbed from the renal tubules into the blood. This reabsorption process is possible due to the active transport of the glucose out of the proximal convoluted tubule and back into the peritubular capillaries. When the concentration of glucose in the blood is within normal limits (70-110 milligrams per 100 milliliters), there are enough transport proteins to carry all of the glucose within the proximal convoluted tubule back into the blood. However, if the blood glucose level exceeds a certain limit (renal plasma threshold), the glucose molecules will not all be reabsorbed and some of the glucose will stay in the urine. The presence of glucose in the urine is called glycosuria. The chief cause of glycosuria is diabetes mellitus, but other conditions, such as hyperthyroidism, hyperpituitarism, and liver disease may also have this affect. KETONES: When there is carbohydrate deprivation, such as in starvation or high-protein diets, the body relies increasingly on the metabolism of fat for energy. This pattern is also seen in people with the disease diabetes mellitus, where lack of insulin prevents the body cells from utilizing the large amounts of glucose available in the blood. This occurs because insulin is necessary for the transport of glucose from the blood into the body cells. The metabolism of fat proceeds in a stepwise manner: (1) triglycerides are hydrolyzed to fatty acids and glycerol; (2) fatty acids are converted into smaller intermediate compounds; and (3) these intermediates are used in aerobic respiration within the cells of the body. When the production of the intermediate compounds (collectively known as ketone bodies) exceeds the body’s need for them, these ketone bodies accumulate in the blood and spill over into the urine. The presence of ketones in the urine is called ketonuria. Observation or Test Normal values Urine specimen Unknown Color pale yellow clear - pale - medium - dark clear - pale - medium - dark Transparency transparent clear – cloudy - slightly cloudy clear – cloudy - slightly cloudy pH 6.0 normal range 4.5 – 8.0 Specific gravity 1.001 – 1.030 Glucose negative Albumin (protein) negative Ketone bodies negative