Cancer
advertisement

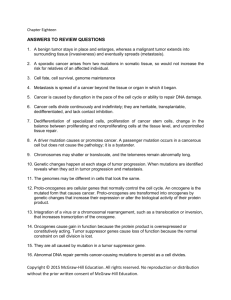
CANCER 1. Know the general characteristics that define cancerous cells and the differences between benign and malignant tumors. 2. Describe how a tumor evolves into an expanding population of cells through repeated rounds of mutation and natural selection. 3. Know the specific properties of cancer cells that are responsible for their uncontrolled proliferation. 4. Describe the altered glucose uptake and sugar metabolism (Warburg effect) that occurs in cancer cells. 5. Describe the steps involved in metastasis of cancer cells. Describe how mutations to cell adhesion molecules such as E-cadherin contribute to metastasis. 6. Know the major types of carcinogens and the relationship between carcinogens and mutagens. 7. Describe how epigenetic changes can contribute to cancer. 8. Describe how cancers can be organized in a hierarchal fashion with cancer stem cells and other cells that have a limited capacity for self-renewal. 9. Distinguish between how mutation of a proto-oncogene and mutation of a tumor suppressor gene contributes to cancer. 10. Describe how a proto-oncogene can be converted into an oncogene by deletion or point mutation in its coding sequence, by chromosomal translocation, or by gene amplification. 11. Distinguish between the genetic mechanisms underlying hereditary and nonhereditary retinoblastoma. 12. Understand how inactivation of the retinoblastoma protein effects cell cycle progression and how alteration of other proteins in the same pathway has equivalent effects. 13. Understand how Ras can be converted into an oncogene by a point mutation that abolishes its GTPase activity. 14. Describe how p53 functions as part of a checkpoint pathway for DNA damage and other cell stresses and how p53 inactivation contributes to formation of many cancers. 15. Describe the normal function of the Apc tumor suppressor gene and how its inactivation contributes to progression of colorectal cancer. 16. Describe how mutations to DNA repair genes increase susceptibility to developing cancer. 17. Describe how the chromosomal translocation that joins Bcr and Abl contributes to development of chronic myeloid leukemia. Describe the recently developed treatment that specifically targets the activated Bcr-Abl oncogene. CANCER 1. Definitions a. Defining characteristics Proliferate without normal restraints that regulate numbers of cells Invade and colonize in other areas of body b. Tumor- mass of cells exhibiting uncontrolled proliferation Benign- clustered together in single mass Malignant (cancer)- invade surrounding tissue, often form metastases (secondary tumors) at other parts of body c. Cancers traditionally classified according to tissue and cell type of origin Carcinomas- epithelia cells, about 80% of human cancers Sarcomas- connective tissue or muscle cells Others- leukemias, lymphomas, nervous system Many subdivisions within these categories 2. Tumor progression a. Derived from single abnormal cell b. Result from somatic mutations Shared DNA abnormalities found in cancer cells Most agents that cause cancer mutate DNA Inherited defects in DNA repair machinery predisposes individuals to cancer c. Single mutation not sufficient to cause cancer- must accumulate multiple mutations in a cell lineage to progress to cancer cell d. Involve evolution through multiple mutations Initially have slightly abnormal cells whose descendents may acquire additional mutations Natural selection process; cell acquiring further random mutation that enhances its proliferation will dominate tumor; successive rounds of random mutation and natural selection results in tumor cells that have increasing ability to proliferate As size of abnormal cell population grows, chance of additional mutation increases Genetic heterogeneity within tumor reflects continuing evolution e. Stages of progression can be classified by histopathology 3. Properties of cancer cells 1 a. Undergo cell division when they should not b. Failure to properly differentiate; cells committed to terminal differentiation typically undergo limited divisions and eventually stop dividing; blocking differentiation can result in these cells continuing to proliferate c. Survive when they should not; failure to undergo apoptosis d. Defective checkpoint control; normal cells respond to DNA damage by arresting cell cycle or undergoing apoptosis; defects in checkpoints allow cancer cells to replicate with DNA damage; promotes further mutations e. Genetic instability; mutations to genes that protect integrity of genome; facilitates accumulation of further mutations that may confer selective advantage f. Overcome replicative cell senescence; many human cells (but not stem cells) have inherent limit to number of divisions due to progressive shortening of telomeres; leads to loss of protective caps; cancer cells either activate telomerase so ends do not shorten or develop alternative mechanism for elongating chromosome ends g. Undergo cell growth through biosynthesis when they should not, aided by altered glucose uptake and sugar metabolism (Warburg effect) Cancer cells import vastly more glucose Only small fraction used to produce ATP by oxidative phosphorylation Many carbon atoms derived from glucose used as building blocks for macromolecules High glucose uptake allows imaging of tumors using PET scan h. Metastasize, by a multi-step process Invade neighboring tissue; epithelial cells break through basal lamina Penetrate blood or lymphatic vessels, exit from circulation, proliferate in new location 4. Carcinogens- agents that cause cancer; most are mutagens a. Mutagens cause DNA damage; include many chemical carcinogens, UV light, ionizing radiation, certain viruses b. Some chemical carcinogens act directly on DNA; many act only after converted to reactive form by metabolic processes 5. Epigenetic changes a. Localized changes to histone modification pattern and DNA methylation can cause heritable inactivation of specific genes that could otherwise function to block tumor growth b. Many cancer-causing mutations alter proteins that determine chromatin structure 2 6. Cancer stem cells a. Many cancers have a hierarchal organization; stem cells comprise a small proportion of cells which are capable of indefinite self-renewal; can give rise to rapidly dividing transit amplifying cells that have limited capacity for selfrenewal and eventually stop dividing b. Cancer stem cells might arise from a normal stem cell or from transit amplifying cells that acquires ability to divide indefinitely c. Effective cancer therapies would need to kill stem cells; might be particularly difficult to kill, which could be reason why cancer often recurs following substantial initial therapeutic effect 7. Genes that contribute to cancer a. Categories Proto-oncogenes - Too much activity of gene product contributes to cancer - Act in dominant manner; gain-of-function mutation in single allele drives tumor progression - Mutant, overactive forms called oncogenes Tumor suppressor genes - Loss of gene product contributes to cancer - Act in recessive mannner; need loss-of-function mutations in both alleles to drive tumor progression b. Mutations that convert proto-oncogene to oncogene Deletion or point mutation in coding sequence; can result in hyperactive protein Chromosomal translocation - In protein coding region can result in hyperactive protein - In adjacent regulatory sequences can result in overexpression of protein Gene amplification; result in overexpression of protein c. Mutations that inactivate tumor suppressor genes Deletions, point mutations, chromosomal rearrangements Both alleles can undergo separate inactivating somatic mutations Individual can inherit one inactive allele; increased susceptibility to cancer because single somatic mutation of other allele can drive tumor progression Can also be inactivated hereditably within cell lineage by epigenetic mechanisms d. Normal cellular functions Internal regulators of cell cycle progression and apoptosis Molecules involved in cell adhesion and movements 3 Components of signaling pathways that allow cells to communicate with environment including secreted proteins, transmembrane receptors, GTPbinding proteins, protein kinases, gene regulatory proteins e. About 300 genes strongly suspected of contributing to cancer; typical cancer has about 10 critical genetic and epigenetic changes that drive cancer Several key pathways commonly disrupted Key pathways include common core components and components feeding into the core that vary by cell type Each biochemical pathway whose disruption contributes to cancer includes multiple oncogenes and tumor suppressor genes; usually only one component of the pathway defective in a particular cancer 8. Retinoblastoma (Rb) protein and its pathway a. Rb is tumor suppressor gene; Rb protein functions to block cell cycle progression b. Retinoblastoma Inactivation of both copies of Rb gene in neural retinal precursor cells sufficient to cause this cancer Hereditary form- inherit one inactive Rb allele; disease occurs frequently because a few cells likely to have other allele inactivated by somatic mutation Nonhereditary form- rare; both alleles inactivated by somatic mutation in same cell c. Rb gene contributes to other cancers, which require additional genetic changes d. Other alterations to Rb pathway Unphosphorylated Rb protein blocks cell cycle progression In normal cell, activation of cyclin D/Cdk4 under appropriate conditions phosphorylates Rb protein to release E2F and stimulate cell cycle progression; p16 inhibits cyclin D/cdk4 complex Mutations causing overactivation of cyclin D or Cdk4 (proto-oncogenes) or inactivation of p16 (tumor suppressor) have similar effect on stimulating cell cycle progression as Rb inactivation 9. Ras proto-oncogene a. Intracellular signaling protein that mediates division or differentiation in many cells in response to growth factors b. Monomeric G protein; acts downstream of receptor tyrosine kinases; converted to active GTP-bound form following receptor stimulation c. GTPase activity causes Ras to remain in inactive GDP-bound form when receptor not stimulated 4 d. Converted to oncogene by point mutation that abolishes GTPase activity; constitutively active Ras; downstream effects mediated by Ras occur independently of growth factor stimulation 10. p53 tumor suppressor gene a. Contributes to nearly all human cancers; p53 or another component of its pathway almost always mutated b. Functions as part of checkpoint pathway that responds to DNA damage or other cell stresses including hyperproliferative condition due to oncogene activation c. Levels rise when cells exposed to DNA damage or other cell stresses d. Can either induce apoptosis or block cell cycle progression e. Transcription factor; turns on p21, which inhibits Cdk complexes required for S phase; turns on pro-apoptotic bcl-2 family proteins f. Inactivation of both copies of p53 allows cells to survive and proliferate despite DNA damage, leading to further genetic alterations 11. Bcl-2 proto-oncogene a. Protein that blocks apoptosis b. Overexpression can contribute to cancer c. Discovered from chromosomal translocation found in B-cell lymphoma that places gene under regulatory sequences that drives its overexpression 12. Genes contributing to metastasis a. Genetic or epigenetic changes that promote metastasis largely unknown, although some genes have been implicated b. Rho-family GTPases: control actin polymerization and actin-based cell motility; oncogene in some cancers, activation by overexpression promotes metastasis c. E-cadherin: cell adhesion at adherens junctions in epithelium; acquiring invasiveness resembles normal developmental process epithelial-mesenchymal transition, in which cells turn off E-cadherin and become more migratory; tumor suppressor for some cancers; loss might promote cancer by increasing local invasiveness 13. Colorectal Cancer- example of how series of genetic alterations effects tumor progression a. Arise from epithelium lining colon; usually begin as small, benign adenoma that forms protruding mass called polyp and slowly progress to more aggressive and eventually malignant tumorMost commonly mutated genes: Apc (adenomatous polyposis coli), p53, K-Ras c. Apc tumor suppressor gene Identified from hereditary condition familial adenomatous polyposis coli (FAP); individuals develop hundreds or thousands of polyps in colon of early adult, some almost always progress to malignancy if not removed 5 FAP inherit one inactive copy of Apc gene in all cells, inactivation of other copy by somatic mutation in cells that form polyps Most colorectal cancer not caused by hereditary condition; >80% of colorectal cancer has both copies of Apc inactivated by somatic mutation Apc protein functions as inhibitory component within Wnt signaling pathway Wnt activates this pathway; regulates maintenance of stem cell state -catenin functions as transcriptional activator in response to Wnt Apc protein part of complex involved in degradation of -catenin in cells not stimulated by Wnt Loss of Apc causes -catenin to activate transcription in absence of Wnt stimulation; uncontrolled expansion of stem cell population d. Common mutations in colorectal cancer often occur in characteristic order that influences tumor progression 14. DNA repair genes a. Inactivation of both copies contributes to cancer because unrepaired DNA damage can lead to further mutations b. Some individuals have increased susceptibility to cancer from inheriting one inactive allele; single somatic mutation of other allele promotes further mutations Hereditary nonpolyposis colon cancer (HNPCC); defective mismatch repair Xeroderma pigmentosum (XP); susceptibility to skin cancer; defective nucleotide excision repair BRCA-1, BRCA-2 mutations; susceptibility to breast cancer; defective repair by homologous recombination 15. Treatment of chronic myeloid leukemia (CML) that targets oncogenic protein a. CML usually involves chromosomal translocation that joins Bcr gene on chromosome 22 with Abl proto-oncogene on chromosome 9; karyotype abnormality known as Philadelphia chromosome b. Results in Bcr-Abl hybrid protein in which N terminal fragment of Bcr joined to C-terminal fragment of Abl c. Abl is tyrosine kinase involved in cell signaling; replacement of N-terminal region in Bcr-Abl results in hyperactive Abl kinase that drives proliferation d. Small molecule drug known as Gleevec inhibits kinase activity of Bcr-Abl; remarkably effective in treating early stage of disease 6