Down's Syndrome/Trisomy 21
advertisement
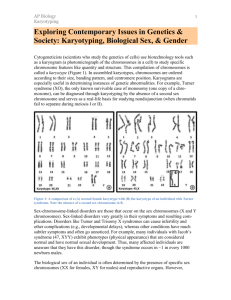
Down’s Syndrome/Trisomy 21 Down syndrome or trisomy 21 (or Down's syndrome in British English[1] and WHO ICD) is a chromosomal disorder caused by the presence of all or part of an extra 21st chromosome. It is named after John Langdon Down, the British doctor who described the syndrome in 1866. The disorder was identified as a chromosome 21 trisomy by Jérôme Lejeune in 1959. The condition is characterized by a combination of major and minor differences in structure. Often Down syndrome is associated with some impairment of cognitive ability and physical growth as well as facial appearance. Down syndrome can be identified during pregnancy or at birth. Cognitive development Cognitive development in children with Down syndrome is quite variable. It is not currently possible at birth to predict the capabilities of any individual reliably, nor are the number or appearance of physical features predictive of future ability. The identification of the best methods of teaching each particular child ideally begins soon after birth through early intervention programs. [32] Since children with Down syndrome have a wide range of abilities, success at school can vary greatly, which underlines the importance of evaluating children individually. The cognitive problems that are found among children with Down syndrome can also be found among typical children. Therefore, parents can use general programs that are offered through the schools or other means. Language skills show a difference between understanding speech and expressing speech. It is not uncommon for children with Down Syndrome to have a speech delay, although it is common for them to need speech therapy to help with expressive language. [33] Fine motor skills are delayed[34] and often lag behind gross motor skills and can interfere with cognitive development. Gross Motor Skills can be affected anywhere from minor to major. Some children will walk at around 2 while others around 4. A physical therapist or APE will help a child with this. [35] Individuals with Down syndrome differ considerably in their language and communication skills. It is routine to screen for middle ear problems and hearing loss; low gain hearing aids or other amplification devices can be useful for language learning. Early communication intervention fosters linguistic skills. Language assessments can help profile strengths and weaknesses; for example, it is common for receptive language skills to exceed expressive skills. Individualized speech therapy can target specific speech errors, increase speech intelligibility, and in some cases encourage advanced language and literacy. Augmentative and alternative communication (AAC) methods, such as pointing, body language, objects, or graphics are often used to aid communication. Relatively little research has focused on the effectiveness of communications intervention strategies.[36] Early childhood intervention, screening for common problems, medical treatment where indicated, a conducive family environment, and vocational training can improve the overall development of children with Down syndrome. Although some of the physical genetic limitations of Down syndrome cannot be overcome, education and proper care will improve quality of life. [2] Characteristics Individuals with Down syndrome may have some or all of the following physical characteristics: oblique eye fissures with epicanthic skin folds on the inner corner of the eyes, muscle hypotonia (poor muscle tone), a flat nasal bridge, a single palmar fold, a protruding tongue (due to small oral cavity, and an enlarged tongue near the tonsils), a short neck, white spots on the iris known as Brushfield spots,[3] excessive joint laxity including atlanto-axial instability, congenital heart defects, excessive space between large toe and second toe, a single flexion furrow of the fifth finger, and a higher number of ulnar loop dermatoglyphs. Most individuals with Down syndrome have mental retardation in the mild (IQ 50–70) to moderate (IQ 35–50) range,[4] with individuals having Mosaic Down syndrome (explained below) typically 10–30 points higher.[5] In addition, individuals with Down syndrome can have serious abnormalities affecting any body system. They also may have a broad head and a very round face. Genetics Down syndrome is a chromosomal abnormality characterized by the presence of an extra copy of genetic material on the 21st chromosome, either in whole (trisomy 21) or part (such as due to translocations). The effects of the extra copy vary greatly among people, depending on the extent of the extra copy, genetic history, and pure chance. Down syndrome occurs in all human populations, and analogous effects have been found in other species such as chimpanzees [6] and mice. Recently, researchers have created transgenic mice with most of human chromosome 21 (in addition to the normal mouse chromosomes). [7] The extra chromosomal material can come about in several distinct ways. A typical human karyotype is designated as 46,XX or 46,XY, indicating 46 chromosomes with an XX arrangement typical of females and 46 chromosomes with an XY arrangement typical of males. [8] Trisomy 21 Trisomy 21 (47,XX,+21) is caused by a meiotic nondisjunction event. With nondisjunction, a gamete (i.e., a sperm or egg cell) is produced with an extra copy of chromosome 21; the gamete thus has 24 chromosomes. When combined with a normal gamete from the other parent, the embryo now has 47 chromosomes, with three copies of chromosome 21. Trisomy 21 is the cause of approximately 95% of observed Down syndromes, with 88% coming from nondisjunction in the maternal gamete and 8% coming from nondisjunction in the paternal gamete.[9] Mosaicism Trisomy 21 is caused prior to conception, and all cells in the body are affected. However, when some of the cells in the body are normal and other cells have trisomy 21, it is called Mosaic Down syndrome (46,XX/47,XX,+21).[10] [11]This can occur in one of two ways: A nondisjunction event during an early cell division in a normal embryo leads to a fraction of the cells with trisomy 21; or a Down syndrome embryo undergoes nondisjunction and some of the cells in the embryo revert to the normal chromosomal arrangement. There is considerable variability in the fraction of trisomy 21, both as a whole and among tissues. This is the cause of 1–2% of the observed Down syndromes.[9] Incidence The incidence of Down syndrome is estimated at 1 per 800 to 1 per 1000 births. [13] In 2006, the Center for Disease Control estimated the rate as 1 per 733 live births in the United States (5429 new cases per year). [14] Approximately 95% of these are trisomy 21. Down syndrome occurs in all ethnic groups and among all economic classes. Maternal age influences the chances of conceiving a baby with Down syndrome. At maternal age 20 to 24, the probability is 1/1562; at age 35 to 39 the probability is 1/214, and above age 45 the probability is 1/19. [15] Although the probability increases with maternal age, 80% of children with Down syndrome are born to women under the age of 35, [16] reflecting the overall fertility of that age group. Recent data also suggest that paternal age, especially beyond 42,[17] also increases the risk of Down Syndrome manifesting in pregnancies in older mothers.[18]Current research (as of 2-19-8) has shown that Down syndrome is due to a random event during the formation of sex cells or pregnancy. There has been no evidence that it is due to parental behavior or environmental factors. Health The medical consequences of the extra genetic material in Down syndrome are highly variable and may affect the function of any organ system or bodily process. The health aspects of Down syndrome encompass anticipating and preventing effects of the condition, recognizing complications of the disorder, managing individual symptoms, and assisting the individual and his/her family in coping and thriving with any related disability or illnesses.[4]Down syndrome can result from several different genetic mechanisms. This results in a wide variability in individual symptoms due to complex gene and environment interactions. Prior to birth, it is not possible to predict the symptoms that an individual with Down syndrome will develop. Some problems are present at birth, such as certain heart malformations. Others become apparent over time, such as epilepsy. The most common manifestations of Down syndrome are the characteristic facial features, cognitive impairment, congenital heart disease (typically a ventricular septal defect), hearing deficits (maybe due to sensory-neural factors, or chronic serous otitis media, also known as Glue-ear), short stature, thyroid disorders, and Alzheimer's disease. Other less common serious illnesses include leukemia, immune deficiencies, and epilepsy. However, health benefits of Down syndrome include greatly reduced incidence of many common malignancies except leukemia and testicular cancer[39] — although it is, as yet, unclear whether the reduced incidence of various fatal cancers among people with Down syndrome is as a direct result of tumor-suppressor genes on chromosome 21 (such as Ets2),[1] because of reduced exposure to environmental factors that contribute to cancer risk, or some other as-yet unspecified factor. In addition to a reduced risk of most kinds of cancer, people with Down syndrome also have a much lower risk of hardening of the arteries and diabetic retinopathy.[2] Life expectancy These factors can contribute to a shorter life expectancy for people with Down syndrome. One study, carried out in the United States in 2002, showed an average lifespan of 49 years, with considerable variations between different ethnic and socio-economic groups.[40] However, in recent decades, the life expectancy among persons with Down Syndrome has increased significantly up from 25 years in 1980. The causes of death have also changed, with chronic neurodegenerative diseases becoming more common as the population ages. amongst both males and females is reduced;[41] there have been only three recorded instances of males with Down syndrome fathering children Edward’s Syndrome/Trisomy 18 Trisomy 18 or Edwards Syndrome (named after John H. Edwards, who first described the syndrome in 1960) is a genetic disorder. It is the most common autosomal trisomy after Down Syndrome that carries to term. It is caused by the presence of three — instead of two — copies of chromosome 18 in a fetus or infant's cells. The additional chromosome usually occurs before conception. A healthy egg or sperm cell contains individual chromosomes - one to contribute to each of the 23 pairs of chromosomes needed to form a normal cell with 46 chromosomes. Numerical errors arise at either of the two meiotic divisions and cause the failure of segregation of a chromosome into the daughter cells (non-disjunction). This results in an extra chromosome making the haploid number 24 rather than 23. Fertilization of these eggs or sperm that contain an extra chromosome results in trisomy, or three copies of a chromosome rather than two. Definition Edwards' syndrome is caused by an extra copy of chromosome 18. For this reason, it is also called trisomy 18 syndrome. The extra chromosome is lethal for most babies born with this condition. It causes major physical abnormalities and severe mental retardation, and very few children afflicted with this disease survive beyond a year. Description Humans normally have 23 pairs of chromosomes. Chromosomes are numbered 1-22, and the 23rd pair is composed of the sex chromosomes, X and Y. A person inherits one set of 23 chromosomes from each parent. Occasionally, a genetic error occurs during egg or sperm cell formation. A child conceived with such an egg or sperm cell may inherit an incorrect number of chromosomes. In the case of Edwards' syndrome, the child inherits three, rather than two, copies of chromosome 18. Trisomy 18 occurs in approximately one in every 3,000 newborns and affects girls more often than boys. Women older than their early thirties have a greater risk of conceiving a child with trisomy 18, but it can occur in younger women. Causes and symptoms A third copy of chromosome 18 causes numerous abnormalities. Most children born with Edwards' syndrome appear weak and fragile, and they are often underweight. The head is unusually small and the back of the head is prominent. The ears are malformed and low-set, and the mouth and jaw are small. The baby may also have a cleft lip or cleft palate. Frequently, the hands are clenched into fists, and the index finger overlaps the other fingers. The child may have clubfeet and toes may be webbed or fused. Numerous problems involving the internal organs may be present. Abnormalities often occur in the lungs and diaphragm (the muscle that controls breathing), and heart defects and blood vessel malformations are common. The child may also have malformed kidneys and abnormalities of the urogenital system. Diagnosis Physical abnormalities point to Edwards' syndrome, but definitive diagnosis relies on karyotyping. Karyotyping involves drawing the baby's blood or bone marrow for a microscopic examination of the chromosomes. Using special stains and microscopy, individual chromosomes are identified, and the presence of an extra chromosome 18 is revealed. Trisomy 18 can be detected before birth. If a pregnant woman is older than 35, has a family history of genetic abnormalities, has previously conceived a child with a genetic abnormality, or has suffered earlier miscarriages, she may undergo tests to determine whether her child carries genetic abnormalities. Potential tests include maternal serum analysis or screening, ultrasonography, amniocentesis, and chorionic villus sampling. Treatment There is no cure for Edwards' syndrome. Since trisomy 18 babies frequently have major physical abnormalities, doctors and parents face difficult choices regarding treatment. Abnormalities can be treated to a certain degree with surgery, but extreme invasive procedures may not be in the best interests of an infant whose lifespan is measured in days or weeks. Medical therapy often consists of supportive care with the goal of making the infant comfortable, rather than prolonging life. Prognosis The survival rate of Edwards Syndrome is very low. About half die in utero. Of liveborn infants, only 50% live to 2 months, and only 5–10% will survive their first year of life. Major causes of death include apnea and heart abnormalities. It is impossible to predict the exact prognosis of an Edwards Syndrome child during pregnancy or the neonatal period. Because major medical interventions are routinely withheld from these children, it is difficult to determine what the survival rate or prognosis would be with aggressive medical treatment. Incidence/prevalence The rate of occurrence for Edwards Syndrome is ~ 1:3000 conceptions and 1:6000 live births, as 50% of those diagnosed prenatally with the condition will not survive the prenatal period. Although women in their 20s and 30s may conceive Edwards Syndrome babies, there is an increased risk of conceiving a child with Edwards Syndrome as a woman's age increases, with the average age for this disorder being 32½.[1] Variations A small percentage of cases occur when only some of the body's cells have an extra copy of chromosome 18, resulting in a mixed population of cells with a differing number of chromosomes. Such cases are sometimes called mosaic Edwards syndrome. Very rarely, a piece of chromosome 18 becomes attached to another chromosome (translocated) before or after conception. Affected people have two copies of chromosome 18, plus extra material from chromosome 18 attached to another chromosome. With a translocation, the person has a partial trisomy for chromosome 18 and the abnormalities are often less than for the typical Edwards syndrome. Features and Characteristic Symptoms and findings may be extremely variable from case to case. However, in many affected infants, the following may be found: Growth deficiency Feeding difficulties Breathing difficulties Developmental delays Mental Retardation Undescended testicles in males Prominent back portion of the head Small head (microcephaly) Low-set, malformed ears Abnormally small jaw (micrognathia) Small mouth Cleft lip/palate Upturned nose Narrow eyelid folds (palpebral fissures) Widely-spaced eyes (ocular hypertelorism) Dropping of the upper eyelids (ptosis) Overlapped, flexed fingers Underdeveloped or absent thumbs Underdeveloped nails Webbing of the second and third toes Clubfeet Small pelvis with limited movements of the hips Short breastbone Kidney malformations Structural heart defects at birth (i.e., ventricular septal defect, atrial septal defect, patent ductus arteriosus) Patau Syndrome/ Trisomy 13 Patau syndrome, also known as trisomy 13, is a chromosomal abnormality, a syndrome in which a patient has an additional chromosome 13 due to a non-disjunction of chromosomes during meiosis. Some are caused by robertsonian translocations. The extra chromosome 13 disrupts the normal course of development, causing the characteristic features of Patau syndrome. Like all nondisjunction diseases (Down syndrome, Edwards syndrome, etc...), the risk of disease in the offspring increases with maternal age at pregnancy, with about 31 years being the average.[1] Patau syndrome affects approximately 1 in 12,000 live births. Description Children normally inherit 23 chromosomes from each parent, for a total of 46 chromosomes. A typical human being has 46 chromosomes: 22 pairs of non-sex linked chromosomes and one pair of sex-linked chromosomes, that determine that child's sex. Sometimes a child may end up with more than 46 chromosomes because of problems with the father's sperm or the mother's egg; or, because of mutations that occurred after the sperm and the egg fused to form the embryo (conception). Normally, there are two copies of each of the 23 chromosomes: one from each parent. A condition called trisomy occurs when three, instead of two, copies of a chromosome are present in a developing human embryo. An extra copy of a particular chromosome can come either from the egg or sperm, or because of mutations that occur after conception. The best-known trisomy-related disorder is Down syndrome (trisomy 21), in which the developing embryo has an extra copy of chromosome 21. Patau syndrome is trisomy 13, in which the developing embryo has three copies of chromosome 13. An extra copy of chromosome 13 is not the only cause of Patau syndrome. Other changes in chromosome 13, such as mispositioning (translocation), can also result in the characteristics classified as Patau syndrome. In these cases, an error occurs that causes a portion of chromosome 13 to be exchanged for a portion of another chromosome. There is no production of extra chromosomes, but a portion of each affected chromosome is "misplaced" (translocated) to another chromosome. Patau syndrome causes serious physical and mental abnormalities including: heart defects; incomplete brain development; such unusual facial features as a sloping forehead, a smaller than average head (microcephaly), small or missing eyes, low-set ears, and cleft palate or hare lip; extra fingers and toes (polydactyly); abnormal genitalia; spinal defects; seizures; gastrointestinal hernias, particularly at the navel (omphalocele); and mental retardation. Due to the severity of these conditions, fewer than 20% of those affected with Patau syndrome survive beyond infancy. Most infants with the syndrome die within the first three months of life; the average life expectancy of the survivors is about 10 years. Causes Most cases of Patau's syndrome result from trisomy 13, which means each cell in the body has three copies of chromosome 13 instead of the usual two copies. A small percentage of cases occur when only some of the body's cells have an extra copy of chromosome 13, resulting in a mixed population of cells with a differing number of chromosomes, such cases are called mosaic Patau. Patau syndrome can also occur when part of chromosome 13 becomes attached to another chromosome (translocated) before or at conception. Affected people have two copies of chromosome 13, plus extra material from chromosome 13 attached to another chromosome. With a translocation, the person has a partial trisomy for chromosome 13 and often the physical signs of the syndrome differ from the typical Patau syndrome. Most cases of Patau syndrome are not inherited, but occur as random events during the formation of reproductive cells (eggs and sperm). An error in cell division called non-disjunction can result in reproductive cells with an abnormal number of chromosomes. For example, an egg or sperm cell may gain an extra copy of chromosome 13. If one of these atypical reproductive cells contributes to the genetic makeup of a child, the child will have an extra chromosome 13 in each of the body's cells. Mosaic Patau syndrome is also not inherited. It occurs as a random error during cell division early in fetal development. As a result, some of the body's cells have the usual two copies of chromosome 13, and other cells have three copies of the chromosome. Patau syndrome due to a translocation can be inherited. An unaffected person can carry a rearrangement of genetic material between chromosome 13 and another chromosome. This rearrangement is called a balanced translocation because there is no extra material from chromosome 13. Although they do not have signs of Patau syndrome, people who carry this type of balanced translocation are at an increased risk of having children with the condition. Prognosis Most embryos with trisomy 13 do not survive gestation and are spontaneously aborted. Of those surviving to term gestation, approximately 82-85% do not survive past 1 month of age, and 85% do not survive past 1 year of age. [2] Certain malformations, especially holoprosencephaly and other central nervous system malformations, yield a more grave prognosis. Of those infants that survive past 1 year, most have few major malformations, but the prognosis remains poor, owing to multiple factors including long term neurological disability, feeding difficulty, and frequent pneumonia and other respiratory infections. Presently there are reports of over 70 children around the world living with Trisomy 13 - Patau Syndrome. Manifestations and physical findings Of those embryos that do survive to gestation and subsequent birth, common anomalies include: mental & motor retardation polydactyly (extra digits) microcephaly low-set ears holoprosencephaly (failure of the forebrain to divide properly). heart defects structural eye defects, including microphthalmia, Peters anomaly, cataract, iris and/or fundus (coloboma), retinal dysplasia or retinal detachment, sensory nystagmus, cortical visual loss, and optic nerve hypoplasia cleft palate or hare lip meningomyelocele (a spinal defect) omphalocele (abdominal defect) abnormal genitalia abnormal palm pattern overlapping of fingers over thumb. cutis aplasia (missing portion of the skin/hair) Recurrence risk Unless one of the parents are carriers of a translocation the chances of a couple having another trisomy 13 affected child is less than 1% (less than that of Down Syndrome). History Trisomy 13 was first observed by Erasmus Bartholin in 1657,[3] but the chromosomal nature of the disease was ascertained by Dr. Klaus Patau in 1960.[4] The disease is named in his honor. Patau syndrome was also described in Pacific island tribes. These reports were thought to have been caused by radiation from atomic bomb tests. The tribes were temporarily moved before and during the test by an x amount of distance. They were then put back where they had been taken; all of this occurred before it was known how long, or even if, radiation still lingered on after a nuclear explosion. Turner’s Syndrome/ XO Turner syndrome or Ullrich-Turner syndrome encompasses several conditions, of which monosomy X is the most common. It occurs in about 1 out of every 2500 female births. [1] Instead of the normal XX sex chromosomes for a female, only one X chromosome is present and fully functional; in rarer cases a second X chromosome is present but abnormal, while others with the condition have some cells with a second X and other cells without it (mosaicism). A normal female karyotype is labeled 46,XX; individuals with Turner syndrome are 45,X. In Turner syndrome, female sexual characteristics are present but generally underdeveloped. Symptoms Common symptoms of Turner syndrome include: Short stature Lymphoedema (swelling) of the hands and feet Broad chest (shield chest) and widely-spaced nipples Low hairline Low-set ears Reproductive sterility Rudimentary ovaries Gonadal Streak (underdeveloped gonadal structures) Amenorrhea, or the absence of a menstrual period Increased weight, obesity Shield shaped thorax of heart Shortened metacarpal IV (of hand) Small fingernails Characteristic facial features Webbing of the neck (webbed neck) Coarctation of the aorta Poor Breast Development Horseshoe kidney Visual Impairments sclera, cornea, Glaucoma, etc. Ear infections and hearing loss. Other symptoms may include a small lower jaw (micrognathia), cubitus valgus (turned-out elbows), soft upturned nails, palmar crease and drooping eyelids. Less common are pigmented moles, hearing loss, and a high-arch palate (narrow maxilla). Turner syndrome manifests itself differently in each female affected by the condition, and no two individuals will share the same symptoms. Risk factors Risk factors for Turner syndrome are not well known. Nondisjunctions increase with maternal age, such as for Down syndrome, but that effect is not clear for Turner syndrome. It is also unknown if there is a genetic predisposition present that causes the abnormality, though most researchers and doctors treating Turners women agree that this is highly unlikely. There is currently no known cause for Turner syndrome, though there are several theories surrounding the subject. Incidence Approximately 98% of all fetuses with Turner syndrome spontaneously abort. Turner syndrome accounts for about 10% of the total number of spontaneous abortions in the United States. The incidence of Turner syndrome in live female births is believed to be 1 in 2500. Diagnosis Turner syndrome may be diagnosed by amniocentesis during pregnancy. Sometimes, fetuses with Turner syndrome are identified by abnormal ultrasound findings (i.e. heart defect, kidney abnormality, cystic hygroma, ascites). Although the recurrence risk is not increased, genetic counseling is often recommended for families who have had a pregnancy or child with Turner syndrome. A blood test, called a karyotype, analyzes the chromosomal composition of the individual. This is the test of choice to diagnose Turner syndrome. Prognosis While most of the physical findings in Turner syndrome are harmless, there can be significant medical problems associated with the syndrome. Cardiovascular Price et al. (1986 study of 156 female patients with Turner syndrome) showed a significantly greater number of deaths from diseases of the circulatory system than expected, half of them due to congenital heart disease--mostly postductal coarctation of the aorta. When patients with congenital heart disease were omitted from the sample of the study, the mortality from circulatory disorders was not significantly increased. Cardiovascular malformations are a serious concern as it is the most common cause of death in adults with Turner syndrome. It takes an important part in the 3-fold increase in overall mortality and the reduced life expectancy (up to 13 years) associated with Turner syndrome. Skeletal Normal skeletal development is inhibited due to a large variety of factors, mostly hormonal. The average height of a woman with Turner syndrome, in the absence of growth hormone treatment, is 4'7", about 140 cm.The fourth metacarpal bone (fourth toe and ring finger) may be unusually short, as may the fifth.Due to inadequate production of estrogen, many of those with Turner syndrome develop osteoporosis. This can decrease height further, as well as exacerbate the curvature of the spine, possibly leading to scoliosis. It is also associated with an increased risk of bone fractures. Kidney Approximately one-third of all women with Turner syndrome have one of three kidney abnormalities: 1. 2. 3. A single, horseshoe-shaped kidney on one side of the body. An abnormal urine-collecting system. Poor blood flow to the kidneys. Some of these conditions can be corrected surgically. Even with these abnormalities, the kidneys of most women with Turner syndrome function normally. However, as noted above, kidney problems may be associated with hypertension. Diabetes Women with Turner syndrome are at a moderately increased risk of developing type 1 diabetes in childhood and a substantially increased risk of developing type 2 diabetes by adult years. The risk of developing type 2 diabetes can be substantially reduced by maintaining a normal weight. Cognitive Turner syndrome does not typically cause mental retardation or impair cognition. However, learning difficulties are common among women with Turner syndrome, particularly a specific difficulty in perceiving spatial relationships, such as Nonverbal Learning Disorder. This may also manifest itself as a difficulty with motor control or with mathematics. While it is non-correctable, in most cases it does not cause difficulty in daily living. Treatment As a chromosomal condition, there is no "cure" for Turner syndrome. However, much can be done to minimize the symptoms. For example: Growth hormones, Estrogen replacement therapy, and reproductive technologies for reproduction. Klinefelter’s Syndrome/ XXY Klinefelter's syndrome, 47, XXY or XXY syndrome is a condition caused by a chromosome aneuploidy. Affected males have an extra X sex chromosome. The principal effects are development of small testicles and reduced fertility. A variety of other physical and behavioral differences and problems are common, though severity varies and many boys and men with the condition have few detectable symptoms. The second most common extra chromosome condition, it is named after Dr. Harry Klinefelter, an endocrinologist at Massachusetts General Hospital, Boston, Massachusetts, who first described it in 1942.[1] The condition exists in roughly 1 out of every 500 males.[2] Because of the extra chromosome, individuals with the condition are usually referred to as "XXY Males", or "47, XXY Males".[3] Signs and symptoms Affected males are almost always effectively sterile, although advanced reproductive assistance is sometimes possible. [4] Some degree of language learning impairment may be present,[5] and neuropsychological testing often reveals deficits in executive functions[6]. In adults, possible characteristics vary widely and include little to no signs of affectedness, a lanky, youthful build and facial appearance, or a rounded body type with some degree of gynecomastia (increased breast tissue).[7] Gynecomastia is present to some extent in about a third of affected individuals, a slightly higher percentage than in the XY population, but only about 10% of XXY males' gynecomastia is noticeable enough to require surgery.[8] The term "hypogonadism" in XXY symptoms is often misinterpreted to mean "small testicles" or "small penis". In fact, it means decreased testicular hormone/endocrine function. Because of this hypogonadism, patients will often have a low serum testosterone level but high serum follicle-stimulating hormone (FSH) and luteinizing hormone (LH) levels.[9] Despite this misunderstanding of the term, however, it is true that XXY men often also have "microorchidism" (i.e. small testicles). [9] The more severe end of the spectrum of symptom expression is also associated with an increased risk of germ cell tumors, breast cancer,[10] and osteoporosis,[2] risks shared to varying degrees[11] with females. Additionally, extant medical literature shows some individual case studies of Klinefelter's syndrome coexisting with other disorders, such as pulmonary disease, varicose veins, diabetes mellitus, and rheumatoid arthritis, but the etiologies (understanding of any potential causation relationship) between Klinefelter's and these other conditions are not well characterized or understood. In contrast to these potentially increased risks, it is currently thought that rare X-linked recessive conditions occur even less frequently in XXY males than in normal XY males, since these conditions are transmitted by genes on the X chromosome, and people with two X chromosomes are typically only carriers rather than affected by these X-linked recessive conditions. There are many variances within the XXY population, just as in the most common 46,XY population. While it is possible to characterise 47,XXY males with certain body types, that in itself should not be the method of identification as to whether or not someone has 47,XXY. The only reliable method of identification is karyotype testing. Not all males with the condition have the same symptoms or to the same degree. Symptoms depend on how many XXY cells a man has, how much testosterone is in his body, and his age when the condition is diagnosed. The XXY condition can affect three main areas of development: Physical development: As babies, many XXY males have weak muscles and reduced strength. They may sit up, crawl, and walk later than other infants. After about age four, XXY males tend to be taller and may have less muscle control and coordination than other boys their age. As XXY males enter puberty, they often don’t make as much testosterone as other boys. This can lead to a taller, less muscular body, less facial and body hair, and broader hips than other boys. As teens, XXY males may have larger breasts, weaker bones, and a lower energy level than other boys. By adulthood, XXY males look similar to males without the condition, although they are often taller. They are also more likely than other men to have certain health problems, such as autoimmune disorders, breast cancer, vein diseases, osteoporosis, and tooth decay. XXY males can have normal sex lives, but they usually make little or no sperm. Between 95 percent and 99 percent of XXY males are infertile because their bodies don’t make a lot of sperm. Language development: As boys, between 25 percent and 85 percent of XXY males have some kind of language problem, such as learning to talk late, trouble using language to express thoughts and needs, problems reading, and trouble processing what they hear. As adults, XXY males may have a harder time doing work that involves reading and writing, but most hold jobs and have successful careers. Social development: As babies, XXY males tend to be quiet and undemanding. As they get older, they are usually quieter, less self-confident, less active, and more helpful and obedient than other boys. As teens, XXY males tend to be quiet and shy. They may struggle in school and sports, meaning they may have more trouble “fitting in” with other kids. However, as adults, XXY males live lives similar to men without the condition; they have friends, families, and normal social relationships. Diagnosis A karyotype is used to confirm the diagnosis. In this procedure, a small blood sample is drawn. White blood cells are then separated from the sample, mixed with tissue culture medium, incubated, and checked for chromosomal abnormalities, such as an extra X chromosome. Cause The extra X chromosome is retained because of a nondisjunction event during meiosis (sex cell division). The XXY chromosome arrangement is one of the most common genetic variations from the XY karyotype, occurring in about 1 in 500 live male births. [2]In mammals with more than one X chromosome, the genes on all but one X chromosome are not expressed; this is known as X inactivation. This happens in XXY males as well as normal XX females.[12] A few genes located in the pseudoautosomal regions, however, have corresponding genes on the Y chromosome and are capable of being expressed.[13] These triploid genes in XXY males may be responsible for symptoms associated with Klinefelter's syndrome. [citation needed] The first published report of a man with a 47,XXY karyotype was by Patricia A. Jacobs and Dr. J.A. Strong at Western General Hospital in Edinburgh, Scotland in 1959.[14] This karyotype was found in a 24-year-old man who had signs of Klinefelter's syndrome. Dr. Jacobs described her discovery of this first reported human or mammalian chromosome aneuploidy in her 1981 William Allan Memorial Award address.[15] Treatment The genetic variation is irreversible, but its symptoms can be altered or treated in a number of ways, including the use of testosterone treatment. [16]The XXY chromosome pattern can not be changed. But, there are a variety of ways to treat the symptoms of the XXY condition. Educational treatments – As children, many XXY males qualify for special services to help them in school. Teachers can also help by using certain methods in the classroom, such as breaking bigger tasks into small steps. Therapeutic options – A variety of therapists, such as physical, speech, occupational, behavioral, mental health, and family therapists, can often help reduce or eliminate some of the symptoms of the XXY condition, such as poor muscle tone, speech or language problems, or low self-confidence. Medical treatments – Testosterone replacement therapy (TRT) can greatly help XXY males get their testosterone levels into normal range. Having a more normal testosterone level can help develop bigger muscles, deepen the voice, and grow facial and body hair. TRT often starts when a boy reaches puberty. Some XXY males can also benefit from fertility treatment to help them father children. Inadequately treated hypogonadism in Klinefelter syndrome increases recognized psychosocial morbidity.[17] At least one study indicates that planned and timed support should be provided for young men with Klinefelter syndrome, to ameliorate current poor psychosocial outcomes.[17] One of the most important factors for all types of treatment is starting it as early in life as possible. Variations The 48, XXYY (male) syndrome occurs 1 in 17,000 births and has traditionally been considered to be a variation of Klinefelter's syndrome. XXYY is no longer generally considered a variation of KS, although it has not yet been assigned an ICD-10 code. Males with Klinefelter syndrome may have a mosaic 47,XXY/46,XY constitutional karyotype and varying degrees of spermatogenic failure. Mosaicism 47,XXY/46,XX with clinical features suggestive of Klinefelter syndrome is very rare. Thus far, only about 10 cases have been described in literature.[18] XYY Syndrome XYY syndrome is an aneuploidy of the sex chromosomes in which a human male receives an extra Y chromosome, producing a 47,XYY karyotype. Some medical geneticists question whether the term "syndrome" is appropriate for this condition because its phenotype is normal and the vast majority (an estimated 97% in the UK) of 47,XYY males do not know their karyotype.[1][2] Physical traits Most often, the extra Y chromosome causes no unusual physical features or medical problems. 47,XYY boys have an increased growth velocity during earliest childhood, with an average final height approximately 7 cm above expected final height. [3] Severe acne was noted in a very few early case reports, but dermatologists specializing in acne now doubt the existence of a relationship with 47,XYY.[4] Testosterone levels (prenatally and postnatally) are normal in 47,XYY males. [5] Most 47,XYY males have normal sexual development and usually have normal fertility. Since XYY is not characterized by distinct physical features, the condition is usually detected only during genetic analysis for another reason. Behavioral characteristics 47,XYY boys have an increased risk of learning difficulties (in up to 50%) and delayed speech and language skills.[1][6][7][8][9][10][11][12] In contrast, a national survey of US children conducted in 2004 for the CDC found that 10% of 47,XYY boys had a learning disability. [13] As with 47,XXY boys and 47,XXX girls, IQ scores of 47,XYY boys average 10–15 points below their siblings.[6][8][9][11] It is important to realize that this amount of variation — an average difference of 12 IQ points — occurs naturally between children in the same family.[6] In 14 prenatally diagnosed 47,XYY boys from high socioeconomic status families, IQ scores available for 6 boys ranged from 100–147 with a mean of 120. For 11 boys with siblings, in 9 instances their siblings were stronger academically, but in one case they were performing equal to and in another case superior to their brothers and sisters. [14] Developmental delays and behavioral problems are also possible, but these characteristics vary widely among affected boys and men, are not unique to 47,XYY and are managed no differently than in 46,XY males.[8][12] Aggression is not seen more frequently in 47,XYY males.[1][6][8][9][10] Cause 47,XYY is not inherited, but usually occurs as a random event during the formation of sperm cells. An error in chromosome separation during metaphase I or metaphase II called nondisjunction can result in sperm cells with an extra copy of the Y chromosome. If one of these atypical sperm cells contributes to the genetic makeup of a child, the child will have an extra Y chromosome in each of the body's cells.[12][15] In some cases, the addition of an extra Y chromosome results from nondisjunction during cell division during a post-zygotic mitosis in early embryonic development. This can produce 46,XY/47,XYY mosaics.[12][15] Incidence About 1 in 1,000 boys are born with a 47,XYY karyotype. The incidence of 47,XYY is not affected by advanced paternal or maternal age.[1][8][11] First case The first published report of a man with a 47,XYY karyotype was by Avery A. Sandberg and colleagues at Roswell Park Memorial Institute in Buffalo, New York in 1961. It was an incidental finding in a normal 44-year-old, 6 ft. [183 cm] tall man of average intelligence who was karyotyped because he had a daughter with Down syndrome.[16][17] 47,XYY was the last of the common sex chromosome aneuploidies to be discovered, two years after the discoveries of 47,XXY, 45,X, and 47,XXX in 1959. Even the much less common 48,XXYY had been discovered in 1960, a year before 47,XYY. Screening for these X chromosome aneuploidies was possible by noting the presence or absence of "female" sex chromatin bodies (Barr bodies) in the nuclei of interphase cells in buccal smears, a technique developed a decade before the first reported sex chromosome aneuploidy.[18] An analogous technique to screen for Y chromosome aneuploidies by noting supernumerary "male" sex chromatin bodies was not developed until 1970, a decade after the first reported sex chromosome aneuploidy.[19][20] In December 1969, Lore Zech at the Karolinska Institute in Stockholm first reported intense fluorescence of the AT-rich distal half of the long arm of the Y chromosome in the nuclei of metaphase cells treated with quinacrine mustard.[21] Four months later, in April 1970, Peter L. Pearson and Martin Bobrow at the MRC Population Genetics Unit in Oxford and Canino G. Vosa at the University of Oxford reported fluorescent "male" sex chromatin bodies in the nuclei of interphase cells in buccal smears treated with quinacrine dihdyrochloride. [22] Fictional depictions A popular misconception in the 1960s and 1970s that XYY males were more prone to criminal behavior led to several novels and TV series which exploited the idea with little regard to the science. Robin Chapman's 1971 episode of the BBC television science fiction series Doomwatch (titled 'By The Pricking Of My Thumbs ...') portrayed the tragic results of this misconception being taken as fact by authority figures. Less sympathetically, Kenneth Royce's series of novels about The XYY Man partially played up to the stereotype, with an anti-hero figure William 'Spider' Scott, whose extra Y chromosome is seen in part to be responsible for his career as a highly skilled (though nonviolent) cat-burglar. Royce's books were turned into a TV series in the UK which ran 3 episodes in the summer of 1976 and 10 episodes in the summer of 1977. In the film Alien 3 (1992) the protagonist lands on a prison planet populated by XYY criminals, with the implication that they are more prone to commit assault, rape or molestation. The short story "The Procrustean Petard," a Star Trek-based short story by Sondra Marshak and Myrna Culbreath, depicted a story where the crew of the Enterprise had their genders reversed, all but Spock who'd instead been given an extra Y chromosome. McCoy was concerned whether Spock's emotional control could handle the "hyper masculinity" the extra Y would cause, worried that he might become prone to emotional outbursts, even violence. In the episode "Born Bad" of the show Law & Order the defense strategy for Chris Paulit, a young boy accused of beating to death another boy, is his extra Y chromosome. Experts are called to testify that the XYY syndrome is more common among the prison population. XXX Syndrome Triple X syndrome is a form of chromosomal variation characterized by the presence of an extra X chromosome in each cell of a human female. The condition is also known as triplo-X, trisomy X, XXX syndrome, and 47,XXX aneuploidy. Triple X results during division of a parent's reproductive cells, which occurs about once in every 1,000 births. Women with trisomy X do not exhibit any symptoms and cannot be distinguished from normal XX females unless karyotyping is performed. Many girls and women with Triple X have no signs or symptoms. Signs and symptoms vary a lot between individuals, but can include: Physical: o Tall stature (height) o Possible mild facial characteristics: increased width between eyes, skin fold at inner eyelid (epicanthal fold), proportionately smaller head size Developmental: o Learning disabilities (70%): Normal IQ, but may be 10-15 points below siblings o Speech and language delays (50%) o Delayed motor skills: poor coordination, awkwardness, clumsiness Behavioral: introverted, difficulty with interpersonal relationships Cause Triple X syndrome is not inherited, but usually occurs as a quite random event during the formation of reproductive cells (ovum and sperm). An error in cell division called nondisjunction can result in reproductive cells with additional chromosomes. For example, an oocyte or sperm cell may gain an extra copy of the X chromosome as a result of the nondisjunction. If one of these cells contributes to the genetic makeup of a child, the child will have an extra X chromosome in each of her cells. In some cases, trisomy X occurs during cell division in early embryonic development. Some females with triple X syndrome have an extra X chromosome in only some of their cells. These cases are called 46,XX/47,XXX mosaics. Symptoms Due to inactivation and formation of a Barr body in all female cells, only one X chromosome is active at any time in a female cell. Thus, triple X syndrome most often causes no unusual physical features or medical problems. Females with the condition are usually taller than average, and their weight may be low in comparison to their height. They may have menstrual irregularities,and, although rarely exhibiting severe mental impairments, have an increased risk of learning disabilities, delayed speech, and language skills. A similar range of body types and characteristics are present in both triple X and Klinefelter's syndrome. These include a lanky/youthful appearance, non-affectedness, or varying degrees of androgyny. The additional X chromosome can come from either the maternal or paternal side. Although body types and characteristics are distinguishable in triple X, the condition is verified only by karyotype testing. Most women with triple X have normal sexual development and are able to conceive children. A few may experience an early onset of menstruation. Triple X women are rarely diagnosed, apart from pre-natal testing methods, such as amniocentesis. Most medical professionals do not regard the condition a disability. However, such status can be sought by parents for early intervention treatment if mild delays are present. Birth to 1 year old. Those children who were 47, XXX weighed less, but tended to be taller. The article states that all of the children “appeared physically normal at birth.” The most abnormal finding was that motor development was delayed (see gross motor on developmental milestones). 1 to 3 years old. Delays in speech and language in addition to gross motor skills became more prominent. 4 to 7 years old. Testing showed the girls to be behind others of their age in language skills. 8/11 of the girls were described by their parents as shy whereas none of the girls who were “controls” were described as such. 6 to 12 years old. The girls with 47, XXX continued to be taller than their female peers, and continued to experience delays in motor and language skills. They were described by the developmental pediatrician as “awkward, clumsy, or poorly coordinated.” 8/11 were described as behaviorally immature. 13 to 20 years old. 10/11 girls studied were above the 80th percentile for height. All of the girls had normal menstrual cycles. 4/11 became pregnant. Neuromotor and language deficits persisted. 7/11 of the girls were given a psychiatric diagnosis including depression, conduct disorders, undersocialization, and psychosomatism. 3 of the 11 girls graduated high school whereas 6/7 of the control subjects over 17 graduated high school. 9/11 of the 47, XXX girls were placed in special education classes. Cognitive The average IQ of children with an extra X chromosome was 11 points lower than normal children. 18% of the 47, XXX girls showed some amount of reading impairment. Of these, 3% showed severe impairment. On a bright note, 3% showed above average reading performance. Likewise, 30% of these girls had a poor arithmetic performance. Of these 4.5% showed severe impairment with an equal amount of girls performing above average. This represents a 2-fold increase in the risk of impairment. Overall, this study remarked on increased rates of grade failure and special education placement. These girls were more likely to fail a grade (42%) than be put in special education (25%). This study also found women with 47, XXX scored lower on an IQ test compared to normal females in the control group. The study also found that these females scored lower on the Global Assessment of Functioning – a measure of their ability to adapt in their family and social relationships, to respond to life’s stresses, and deal with their personal weaknesses and strengths. Both the women and psychiatrists found that “social adjustment” was decreased in 47, XXX women. 5 out of 11 of these women completed high school, 2 attended college and obtained a bachelor’s degree. 8 of these women became pregnant also. Incidence Triple X syndrome occurs in around 1 in 1,000 girls. On average, five to ten girls with triple X syndrome are born in the United States each day.[1] Mosaics This describes a chromosome study that shows a mixture of normal cells and cells with an extra X chromosome. A girl with mosaicism will usually have fewer effects of the extra chromosome, because not all of her cells have this extra genetic material. She will probably not be much different than she would be if her chromosome study showed all normal cells. First case The first published report of a woman with a 47,XXX karyotype was by Patricia A. Jacobs, et al. at Western General Hospital in Edinburgh, Scotland, in 1959. It was found in a 35-year-old, 5 ft. 9 in. (176 cm) tall, 128 lb. (58.2 kg) woman who had premature ovarian failure at age 19; her mother was age 41 and her father was 40 at the time of her conception. [2]