Chapter 28
advertisement
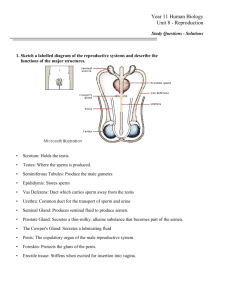
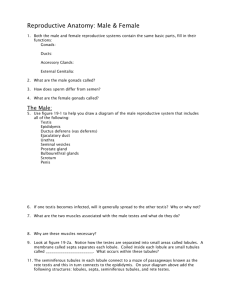
Chapter 28 Introduction to the Reproductive System ▪The reproductive system includes the following components: -Gonads -Ducts that receive and transport gametes -Accessory glands and organs -External genitalia (perineal structures) The Reproductive System of the Male ▪The Testes ▫Descent of the testes usually occurs in the 7th month of gestation ▫Spermatic cords contain nerves and blood vessels that serve the testes ▫Scrotum is separated into two chambers, keeps infection or inflammation from spreading from one testis to the other. -Contains a thin layer of skin and underlying superficial fascia -Dartos muscle-Cremaster muscle▫Tunical albuginea▫Septa divide the testes into lobules, seminiferous tubules are distributed among the lobules ▫Each semiferous tubule is about 80 cm in length, sperm production occurs in these tubules. ▫Rete testis▫Interstitial cells- 1 ▪Spermatogenesis- process of producing spermatozoa, involves three integrated processes: 1) mitosis2) meiosis3) Spermiogenesis*Use figure 28-6 and 28-7 to familiarize yourself with the processes of spermatogenesis and spermiogenesis.* ▫Nurse cells play a key role in spermatogenesis, 6 important functions: 1. 2. 3. 4. 5. 6. ▪The Anatomy of a Spermatozoon- Each spermatozoon has three distinct regions ▫Head▫Middlepiece▫Tail▫Mature spermatozoon lacks ER, Golgi, Lysosomes, and Peroxisomes, must absorb nutrients from surrounding fluid. ▪The Male Reproductive Tract- testes produce physically mature spermatozoa, but they are not functionally mature. ▫Epididymis- the start of the male reproductive tract, almost 23 feet long. 2 -Has three main functions: 1. 2. 3. ▫Ductus Deferens- about 16-18 inches long, begins at the tail of the epididymis and continues on to the ejaculatory duct. ▫Urethra- ductus deferens empties into the urethra, made of three regions. ▪The Accessory Glands- provide nutrients for spermatozoa, activates spermatozoa, propels spermatozoa, and produces buffers to protect against urine and vaginal acids. ▫Seminal Vesicles- glands embedded in CT on either side of the midline ▫Prostate Gland- small, muscular, round gland that surrounds the initial portion of the urethra. ▫Bulbourethral Glands- small gland embedded in the urogenital diaphragm ▪Semen- also called ejaculate, usually 2-5 mL per ejaculation, contains: ▫Spermatozoa▫Seminal Fluid▫Enzymes- 3 ▪External Genitalia- consists of the scrotum and the penis ▫Penis- a tubular organ through which conducts urine to the exterior, and introduces semen into the female’s vagina during sexual intercourse. Divided into three regions: 1) The root2) The body3) The glans-Surrounding the internal structures of the penis are three regions of erectile tissue; corpora cavernosa (2) and corpus spongiosum. ▪Hormones and Male Reproductive Function- The major hormones of the male reproductive system are FSH, LH, GnRH, inhibin, and testosterone. ▫FSH and Spermatogenesis- FSH targets primarily nurse cells of the seminiferous tubules. ▫LH and Androgen Production- LH causes the secretion of testosterone and other androgens by the interstitial cells of the testes. *see figure 28-12 to see these mechanisms* The Reproductive System of the Female ▪The Ovaries- paired, small, lumpy organs located near the lateral walls of the pelvic cavity. Perform three main functions: 1) 2) 3) 4 ▫Can be divided into the outer cortex and inner medulla, gametes are produced in the cortex. ▫Oogenesis- ovum production begins before a woman’s birth, accelerates during puberty, and ends at menopause. -Differ from meiosis in males in that: 1) 2) *See figure 28-15 to understand the process of oogenesis* ▫The Ovarian Cycle- can be divided into the follicular phase and the luteal phase. Can be summarized by the following steps: 1) 2) 3) 4) 5) 6) ▪The Uterine Tubes- hollow muscular tube, roughly 13 cm long, divided into three segments: ▫Infundibulum▫The Ampulla▫Isthmus▪The Uterus- provides mechanical protection, nutritional support, and waste removal for the developing embryo and fetus. Also contractions of the muscular wall of the uterus is important for ejecting the fetus at the time of birth. ▫Composed of two main regions, the body and the cervix 5 -The superior part of the body is called the fundus, body ends at the uterine isthmus -Cervix extends from uterine isthmus to the vagina. ▫The uterine wall is composed of three layers, endometrium, myometrium, and perimetrium. -Endometrium-Myometrium-Perimetrium- ▫The endometrium can be divided into a functional zone and a basilar zone. -The functional zone -The basilar zone ▫The structure of the basilar zone remains consistent over time, while that of the functional zone changes during the uterine cycle. -This is mostly due to the types of blood vessels found in the zones ▫The uterine cycle (menstrual cycle)- averages 28 days in length. Can be divided into three phases: 1) menses2) proliferative phase3) secretory phase▫Menarche and Menopause- menarche is the first uterine cycle. Menopause is the last uterine cycle. 6 ▪The Vagina- an elastic muscular tube extending between the cervix and the vestibule. Has three major functions: 1) 2) 3) ▫The lining of the vagina is moistened by the secretions of the cervical glands and by water movement ▫Vagina and vestibule are separated by the hymen, and epithelial fold that partially or completely blocks the entrance to the vagina before the initial sexual intercourse. ▫Bulbospongiosus muscles extend along either side of the vaginal entrance. ▫Lumen is lined by nonkeratinized stratified squamous epithelium ▫Vagina contains a normal population of bacteria that produce an acidic environment. ▪External Genitalia- contained within the vulva ▫Vestibule▫Clitoris▫Prepuce of clitoris▫Mons pubis▫Labia majora▪The Mammary Glands- used for nourishment of an infant, lactation occurs here. ▫Lactation- process of milk production ▫Mammary glands are specialized organs of the Integumentary system that are controlled mainly by hormones of the reproductive system and the placenta. 7 ▪Hormones and the Female Reproductive Cycle- coordinate the uterine cycle and the ovarian cycle to ensure proper reproductive function. ▫If these two cycles are not coordinated, infertility can result ▫GnRH regulates the release of FSH and LH by changing the pulse frequency and amplitude throughout the course of the ovarian cycle. ▫Changes in the GnRH pulse frequency are controlled by circulating levels of estrogens and progestins; estrogens increase GnRH pulse frequency while progestins decrease it. ▫Follicular development begins under FSH stimulation, primordial follicles begin to develop into primary follicles. -Thecal cells begin producing androstenedione, a precursor to most sex hormones. Converted to estrogens by granulose cells. -Small quantities of estrogens are released by interstitial cells scattered throughout the ovarian stroma -Circulating estrogens are bound primarily to albumins, lesser amount carried by gonadal steroid-binding globulin (GBG) ▫Three estrogens circulate in the bloodstream: 1) estradiol 2) estrone 3) estriol -Estradiol is the most abundant estrogen, the dominant hormone prior to ovulation. -Estrogens have multiple functions *See figure 28-24 to familiarize yourself with the hormonal regulation of ovarian activity, uterine cycle, and basal body temperature* 8