© 2004 WebMD, Inc. All rights reserved.
ACS Surgery: Principles and Practice
5 GASTROINTESTINAL TRACT AND ABDOMEN
11
11 CROHN DISEASE — 1
CROHN DISEASE
Susan Galandiuk, M.D., F.A.C.S., F.A.S.C.R.S.
The role of surgery in the management of Crohn disease has
undergone a dramatic evolution over the past 50 years.
Currently, surgical treatment of Crohn disease is seldom performed in the emergency setting; it is nearly always performed
after failed medical therapy.The decision to proceed with operative management is based on careful patient evaluation, with full
awareness of the potential complications and ramifications of
treatment. In particular, attention must be paid to the risk of
recurrent disease, the possible surgical sequelae, and the side
effects of medical therapy.
Classification
There are many systems for classifying Crohn disease. One of
the simplest is the classification developed by Farmer and associates,1 which categorizes the disease on the basis of disease location
alone (ileocolic, purely colonic, small bowel, and perianal). A more
elaborate system is the Vienna classification, which categorizes the
disease on the basis not only of location but also of age of onset
and disease behavior.2 In this system, there are four categories for
disease location: terminal ileum (L1), colon (L2), terminal ileum
and colon (L3), and any location proximal to the terminal ileum
(L4). There are two categories for age of onset: less than 40 years
of age (A1) and 40 years of age or older (A2). Finally, there are
three categories for disease behavior: nonstricturing and nonpenetrating (B1), stricturing (B2), and penetrating (B3).
Given that there are as many types and combinations of Crohn
disease as there are patients with this condition, the most sensible
approach is probably to use some combination of these two classification schemes. Careful evaluation of the specifics of each case
will yield the best treatment results; however, general classification
of the disease can help guide therapy. Broadly speaking, Crohn
disease of the small bowel has the highest recurrence rate. Because
of the important function of the small bowel in digestion, surgeons
tend to emphasize conserving small bowel length during operative
treatment of Crohn disease. Currently, however, there is an increasing focus on colon conservation with the aims of maintaining
water absorption in patients and delaying (or perhaps eliminating)
the need for a stoma.
the known risk of disease recurrence after surgical treatment of
Crohn disease and the significant associated operative morbidity. In
one single-center study, the reoperation rate for Crohn disease was
34% at 10 years.3 The agents used to treat Crohn disease can be divided into several broad groups: probiotics, antibiotics, anti-inflammatory drugs, immunosuppressive drugs, and biologic agents.These
can be used alone or in combination to treat disease, as well as to
maintain remission [see Table 1].
Few good studies have been done on the cost-effectiveness of
medical or surgical therapy4,5 versus that of timely surgery followed by maintenance medical therapy.There is clearly a need for
such studies.The use of potent and expensive immunomodulator
therapy (e.g., maintenance infliximab) for simple ileocolic disease
is questionable, especially in the light of studies indicating that
such treatment is not at all innocuous.6,7
CHANGING CONCEPTS IN SURGERY FOR CROHN DISEASE
Although first described in the beginning of the 19th century,
Crohn disease was not recognized as a discrete clinical entity until
the first part of the 20th century.8 At one point, it was treated surgically in much the same way as cancer, with frozen-section margins obtained at the time of resection.This approach did not yield
any substantial reduction in the recurrence rate.9 In fact, overzealous resections often resulted in Crohn patients’ requiring lifelong
parenteral nutritional support.10 Accordingly, conservative surgery
is now the rule: only gross macroscopic disease is resected into palpably normal margins (in particular, a palpably normal mesenteric
border of the bowel).
General Indications for Surgical Treatment
SIDE EFFECTS OF MEDICAL THERAPY
Significant side effects of medical therapy include those associated with failure to wean from prednisone (e.g., cataract forma-
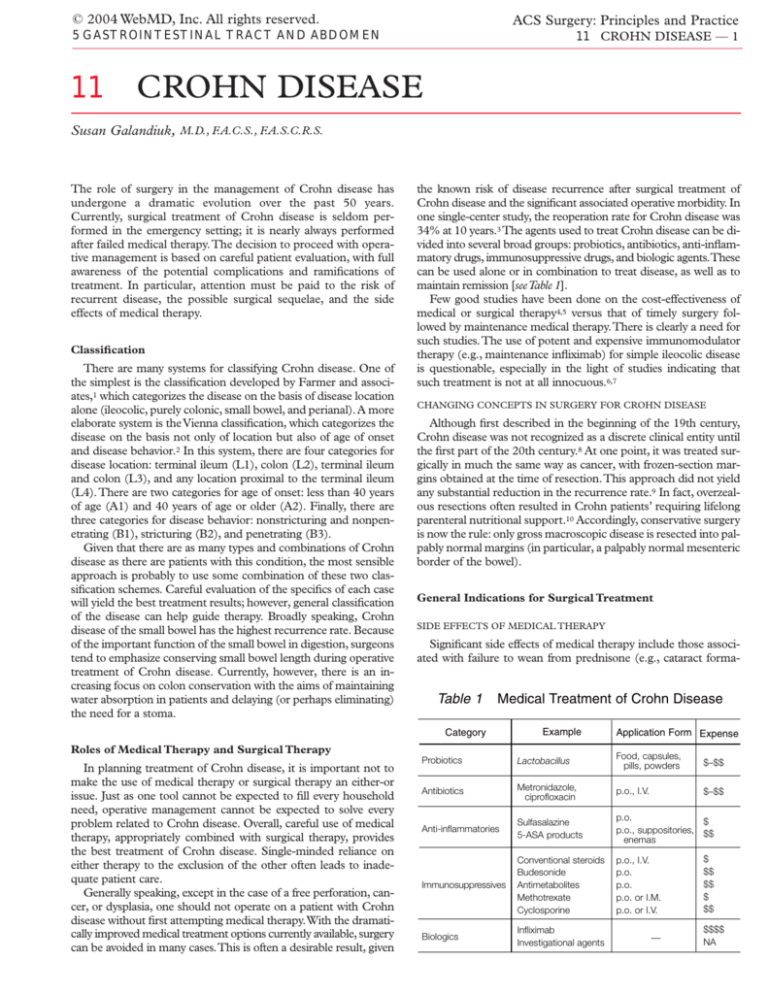
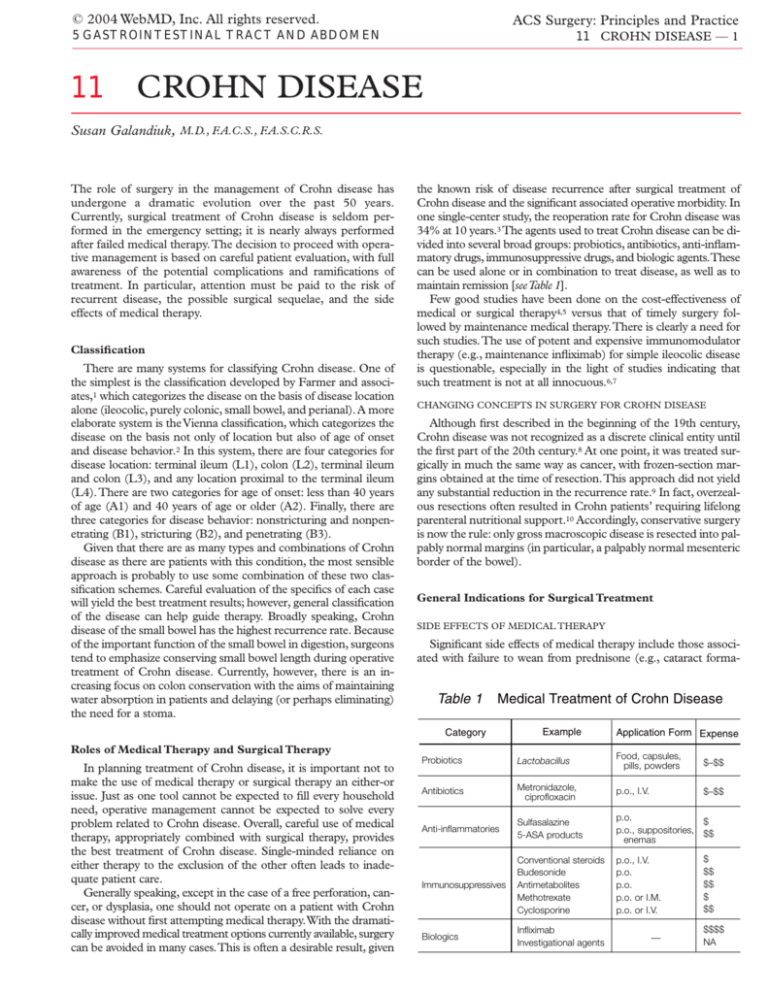
Table 1
Medical Treatment of Crohn Disease
Category
Example
Roles of Medical Therapy and Surgical Therapy
In planning treatment of Crohn disease, it is important not to
make the use of medical therapy or surgical therapy an either-or
issue. Just as one tool cannot be expected to fill every household
need, operative management cannot be expected to solve every
problem related to Crohn disease. Overall, careful use of medical
therapy, appropriately combined with surgical therapy, provides
the best treatment of Crohn disease. Single-minded reliance on
either therapy to the exclusion of the other often leads to inadequate patient care.
Generally speaking, except in the case of a free perforation, cancer, or dysplasia, one should not operate on a patient with Crohn
disease without first attempting medical therapy.With the dramatically improved medical treatment options currently available, surgery
can be avoided in many cases.This is often a desirable result, given
Application Form Expense
Probiotics
Lactobacillus
Food, capsules,
pills, powders
$–$$
Antibiotics
Metronidazole,
ciprofloxacin
p.o., I.V.
$–$$
Anti-inflammatories
Sulfasalazine
5-ASA products
p.o.
$
p.o., suppositories, $$
enemas
Immunosuppressives
Conventional steroids
Budesonide
Antimetabolites
Methotrexate
Cyclosporine
p.o., I.V.
p.o.
p.o.
p.o. or I.M.
p.o. or I.V.
Biologics
Infliximab
Investigational agents
—
$
$$
$$
$
$$
$$$$
NA
© 2004 WebMD, Inc. All rights reserved.
ACS Surgery: Principles and Practice
5 GASTROINTESTINAL TRACT AND ABDOMEN
11 CROHN DISEASE — 2
Abscess Formation
Abscesses are particularly common with ileocolic Crohn disease. If they cannot be controlled by means of computed tomography–guided drainage, surgical therapy may be indicated.
Cancer or Dysplasia
The risk of colorectal cancer is approximately three times higher
in patients with Crohn disease than in the general population.11-13
Failure to Grow
In children, failure to grow and develop normally is one of the
main indications that medical therapy for Crohn disease has been
unsuccessful.Timely surgical therapy will permit normal development. On occasion, when bone age lags significantly behind
chronological age, treatment with recombinant human growth hormone is required.
Figure 1 Shown is an example of stenotic ileocolic Crohn disease resulting in obstructive symptoms that were not relieved by
medical therapy.
tion, aseptic necrosis of the femoral head, and weight gain). Side
effects of antimetabolite therapy include pancreatitis, neutropenia, and opportunistic infections.
COMPLICATIONS OF DISEASE
Lack of Response to Medical Therapy
Many patients with so-called toxic colitis do not respond satisfactorily to medical treatment. In severe cases of refractory disease, if surgery is not performed, colonic perforation, peritonitis,
and multiple organ failure may ensue. Such cases are much less
frequent now than they once were.
Special Considerations
PREGNANCY
Persons who have Crohn disease may be less fertile than healthy
age-matched persons. One possible explanation for this difference is
that feeling ill may result in reduced sexual desire or decreased sexual activity. Another is that pelvic inflammation caused by Crohn disease or by scarring and adhesion formation resulting from surgery
may impair fertility.To reduce the chances of the latter, hyaluronic
acid sheets may be placed around the tubes and ovaries; alternatively, the ovaries may be tacked to the undersurface of the anterior abdominal wall with absorbable sutures and thereby prevented from
entering the pelvis.
Obstruction
In many patients with Crohn disease, the behavior of the disease changes over time, from a more inflammatory and edematous process to one characterized more by fibrosis and scarring.
Whereas anti-inflammatory drugs are ideal for treating the former, surgery is frequently necessary for the latter. Failure to refer
for surgical treatment of obstruction is, unfortunately, a common
error among gastroenterologists. Severe abdominal pain is always
a warning sign of obstruction and should be taken seriously [see
5:1 Acute Abdominal Pain and 5:4 Intestinal Obstruction]. The importance of this point is illustrated by a case from my experience,
involving a patient who had obstructing ileocolic Crohn disease
with gross proximal distention of the terminal ileum [see Figure 1].
This patient lost 20 lb, was experiencing severe abdominal pain,
and was treated for more than a year with 6-mercaptopurine before
being referred for operative management. Ileocolic resection led
to rapid resolution of the symptoms.
Symptomatic Fistulas
Enteroenteric fistulas, by themselves, are no longer considered
an absolute indication for operation in the absence of other complicating factors. Symptomatic fistulas, such as those associated
with obstruction or those associated with disabling symptoms
(e.g., rectovaginal fistulas or enterocutaneous fistulas [see Figure
2]), may have to be treated surgically. Ileosigmoid fistulas, which
effectively bypass the entire colon, may be associated with profound and refractory diarrhea (i.e., ≥ 20 bowel movements/day)
and may also have to be treated operatively.
Figure 2 Shown is an enterocutaneous fistula that persisted for
more than 1 year after an ileocolic resection (arrow). The choice
of parallel incisions by the previous surgeon made selection of a
temporary stoma site much more difficult.
© 2004 WebMD, Inc. All rights reserved.
ACS Surgery: Principles and Practice
5 GASTROINTESTINAL TRACT AND ABDOMEN
There is no evidence that pregnancy exacerbates Crohn disease;
however, there are some specific concerns that apply to pregnant
patients with this condition. Because patients with Crohn disease
often have more-liquid bowel movements, they have a particular
need for a well-functioning anal sphincter. If there is any chance of
an obstetrics-related injury (e.g., from a large baby in a primagravida or from a breech presentation), a cesarean section is advisable to minimize the risk of sphincter trauma.The same is true in
the presence of severe perianal Crohn disease. During pregnancy,
prednisone and 5-aminosalicylic acid (5-ASA) medications are
safe, whereas drugs such as metronidazole are not. If imaging
studies are needed, magnetic resonance imaging and ultrasonography are the modalities of choice.
MARKING OF STOMA SITES AND CHOICE OF INCISION
When a patient with Crohn disease is expected to need an
ileostomy [see 5:30 Intestinal Stomas], it is extremely important to
mark the site preoperatively.What looks flat when the patient is on
the operating table may not be flat when he or she is upright.The
patient must be asked to sit and lean over to confirm that the
marked stoma site is in an area without folds, creases, or previous
incisions. Stoma appliances do not adhere well to areas of previous scarring, and these should be avoided whenever possible.
Patients with Crohn disease do not react to intra-abdominal
infection in a typical fashion. It is not unusual to find unsuspected abscesses that were not revealed by preoperative CT scans and
other imaging studies. If there is even a remote chance of an
unsuspected abscess (particularly in cases of obstructing ileocolic
Crohn disease), the possibility of a temporary stoma should be
raised with the patient and the proposed stoma site marked preoperatively.
A key point is the necessity of planning for the future. Many
patients with Crohn disease will eventually require a stoma. Operating through a midline abdominal incision preserves all four quadrants for possible future stoma sites (if needed).
LAPAROSCOPY
Laparoscopic surgical techniques have gained acceptance in the
treatment of Crohn disease. In performing a laparoscopic operation for Crohn disease, it is essential to adhere to the same technical standards that apply to corresponding open procedures.
Careful intraoperative exploration of the abdomen is important, in
that many patients have multifocal disease. Without such exploration, patients may experience persistent postoperative symptoms
as a consequence of persistent proximal pathologic states that were
not addressed. As with other treatment modalities, there are some
circumstances in which laparoscopy is particularly useful and others in which it should not be used. For example, a laparoscopic
approach is ideal for fecal diversion in patients with perianal
Crohn disease.
Ileocolic resection for Crohn disease also lends itself well to a
laparoscopic-assisted approach; compared with open resection,
laparoscopic resection has been reported to result in shorter hospital stays and reduced costs.14,15 The ileocolic vessels originate
centrally, and they only lie over the retroperitoneum. Once the lateral peritoneal attachments are divided, the colon and the small
bowel mesentery can be exteriorized, and the mesentery can be
divided and the anastomosis performed extracorporeally.
Many studies have shown that even fistulizing Crohn disease
can be safely addressed laparoscopically, depending on the skill of
the surgeon. A hand-assisted approach is often useful with cases of
dense fixation, in which fistulas are common and finger dissection
may facilitate definition of the anatomy. If in doubt, one should
11 CROHN DISEASE — 3
not hesitate to convert to an open procedure.Typically, most areas
that feel fibrotic or contain fibrotic adhesions are actually areas of
fistulizing disease and should be treated as such until proved otherwise. In one study, patients with recurrent disease, those older
than 40 years, and those with an abdominal mass were more likely to require conversion to an open procedure.16
Surgical Management of Crohn Disease at Specific Sites
ESOPHAGEAL, GASTRIC, AND DUODENAL DISEASE
Crohn disease of the upper alimentary tract can be difficult to
diagnose, largely because it is relatively uncommon. Obstructing
strictures due to Crohn disease in this area are unusual; the unsuspected finding of noncaseating granulomas in biopsies of erythematous areas in a patient with Crohn disease in other locations is
diagnostic.
Occasionally, a patient with Crohn disease of the distal esophagus requires dilatations, but this is uncommon. Surgical treatment
for Crohn disease of the upper alimentary tract is almost exclusively reserved for disease affecting the duodenum. Diagnosis of
duodenal Crohn disease can be difficult and requires a certain
amount of suspicion. Frequently, the diagnosis is not made until
relatively late, because diagnostic imaging tends to focus on
endoscopy and because the degree of duodenal obstruction is
often not evident except on barium studies.The rigidity and luminal narrowing of the second portion of the duodenum is typically
much more readily apparent on contrast studies than on endoscopy. Duodenal Crohn disease can lead to gastric outlet obstruction. In children, it can be mistaken for annular pancreas.
When duodenal Crohn disease does not respond to medical
therapy, gastrojejunostomy with vagotomy is the preferred surgical
treatment.17,18 Failure to perform a vagotomy may result in marginal ulcer formation and obstruction. Some surgeons have performed duodenal strictureplasty to treat duodenal Crohn disease.
The results have been conflicting19,20; the feasibility of this operative approach is limited by the pliability of the duodenum. Many
patients experience prompt and full recovery of normal gastric
emptying after operation, but some patients with long-standing
gastric outlet obstruction continue to experience impaired emptying. The latter may benefit from administration of a prokinetic
agent (e.g., metoclopramide or erythromycin).
JEJUNOILEAL DISEASE
Short Bowel Syndrome
Although Crohn disease of the small bowel is not common and
accounts for a relatively small proportion of all cases, disease in
this area is associated with one of the highest overall recurrence
rates. Resection of large portions of the small bowel can result in
short bowel syndrome. For this reason, before proceeding with any
type of small bowel or ileocolic resection, one should measure the
length of the existing small bowel to determine the patient’s
“bowel resource.” One naturally would more readily perform a
resection in a patient who has 400 cm of normal small bowel than
in one who has only 200 cm.
Resection versus Strictureplasty
The major advance in the surgical treatment of Crohn disease
over the past quarter-century has been the technique of small
bowel strictureplasty, first proposed by Lee and subsequently popularized by Williams, Fazio, and others.17,18 Currently, the two
most prevalent strictureplasty techniques are Heineke-Mikulicz
© 2004 WebMD, Inc. All rights reserved.
ACS Surgery: Principles and Practice
5 GASTROINTESTINAL TRACT AND ABDOMEN
strictureplasty [see Figure 3] and Finney strictureplasty [see Figure
4].The former is best suited for strictures up to 5 to 7 cm long [see
Figure 5], the latter for strictures up to 10 to 15 cm long.The sideto-side strictureplasty described by Michelassi21 is suitable for
longer areas of stricture; however, this technique involves longer
suture lines and is mainly considered for patients who already
have, or are at high risk for, short bowel syndrome.
The short, isolated strictures characteristic of diffuse jejunoileal
Crohn disease are more frequently described in patients with longstanding Crohn disease. It has been postulated that over time,
Crohn disease progresses from an edematous condition to a more
fibrotic, stricturing condition.22 It is the fibrotic strictures characteristic of the later stage of the disease that are amenable to treatment with strictureplasty. Patients with these short fibrotic strictures typically have obstructive symptoms and often are unable to
tolerate solid food, experiencing dramatic weight loss as a result.
Although strictureplasty leaves active disease in situ, it usually
leads to prompt resolution of obstructive symptoms, regaining of
lost body weight, and restoration of normal nutritional status.
a
11 CROHN DISEASE — 4
a
b
c
b
Figure 4 Finney strictureplasty. (a) This procedure is suitable
for longer areas of stricture (up to 10 to 15 cm). (b) The strictured
bowel is bent into the shape of an inverted U. Stay sutures are
placed at the apex of the U, which is at the midpoint of the stricture, and at the far ends, which lie 1 to 2 cm proximal and distal
to the stricture. A longitudinal enterotomy is made on the
antimesenteric border of the bowel with the electrocautery. A
side-to-side anastomosis is then performed, with the posterior
wall done first. (c) Shown is the completed anastomosis.
c
Figure 3 Heineke-Mikulicz strictureplasty. Stay sutures are
placed parallel to each other on the antimesenteric border of the
bowel over the area of the stricture. (a) The antimesenteric border of the bowel is then opened with the electrocautery over the
area of the stricture, and the opening is extended for approximately 1 to 2 cm on either side of the stricture. (b, c) Traction is
placed on the stay sutures, and the original longitudinal enterotomy is closed in a horizontal fashion in one or two layers.
A significant concern with strictureplasty is the possibility that
small bowel adenocarcinoma may develop; several cases have been
reported.23,24 I have treated a patient in whom a poorly differentiated jejunal adenocarcinoma developed at the site of a strictureplasty that had been performed 10 years earlier. Accordingly, many
surgeons advocate routine biopsy of the active ulcer on the mesenteric side of the bowel at the time of strictureplasty [see Figure 6].
Another concern has to do with the number of strictureplasties
that can safely be performed in a single patient in the course of a
single operation. As many as 19 strictureplasties have been performed during one procedure without increased morbidity.25
Strictureplasty can be performed with either a single-layer or a
double-layer anastomosis. It should not be performed in the presence of an abscess, a phlegmon, or a fistula; and like any other
anastomosis, it should not be performed proximal to an existing
obstruction that is not treated at the time of operation.
Areas of small bowel Crohn disease that are too long to be treated with strictureplasty can be treated with segmental resection.
© 2004 WebMD, Inc. All rights reserved.
ACS Surgery: Principles and Practice
5 GASTROINTESTINAL TRACT AND ABDOMEN
11 CROHN DISEASE — 5
erature to suggest that the postoperative recurrence rate may be lower with a wider anastomosis.27 The anastomosis can be performed in
either one or two layers. If the bowel is thicker, a handsewn anastomosis is preferred to a stapled one.
The incidence of reoperation for recurrent disease after ileocolic resection is high and increases with the number of resections.28
Postoperative chemoprophylaxis with mesalamine can significantly reduce the recurrence rate.29 Patients who smoke should be
strongly encouraged to stop: the rate and severity of recurrence are
increased in smokers.20
Special Circumstances
Figure 5 Shown is a short fibrotic stricture that is ideally suited
to treatment with Heineke-Mikulicz strictureplasty.
The area to be resected should be as short as possible.There is no
need to obtain frozen-section margins to determine the extent of
resection; doing so leads to unnecessary loss of small bowel
length.26 The resection should extend into palpably normal areas
of small bowel. The easiest way of determining the area to be
resected is to feel the mesenteric margin of the bowel until palpably normal tissue is reached. Because Crohn disease is generally
more severe on the mesenteric side of the bowel, palpation in this
area gives the most accurate impression of the intraluminal character of the bowel. Because it is not uncommon for patients to
have multifocal Crohn disease, the entire small bowel should always be inspected at the time of operation. Operating on one area
of disease while failing to treat a more proximal lesion is clearly not
in the patient’s interest.
Because of the high rate of recurrence in patients with isolated
small bowel disease, postoperative chemoprophylaxis should be
strongly considered. In these patients, I prefer to use a more potent
agent, such as an antimetabolite, rather than a 5-ASA agent.
Ileocolic Crohn disease is often associated with intra-abdominal
abscesses or fistulas. If an associated abscess is known to be present, CT-guided drainage should be done preoperatively so that a
single-stage procedure can then be performed. If an unsuspected
abscess is identified at the time of operation, the safest approach is
to proceed with bowel resection, perform the posterior wall of the
anastomosis, and exteriorize the anastomosis as a loop ileostomy.
This loop ileostomy can then be safely closed, often without a formal laparotomy, 8 weeks after operation if there are no signs of
ongoing sepsis. If the abscess or the terminal ileal loop is adherent
to the sigmoid colon, an ileosigmoid fistula may be present. The
decision whether to resect the sigmoid colon is dictated by the
appearance and feel of the sigmoid in the involved areas. If only a
portion of the anterior colon wall is involved, that portion can be
excised in a wedgelike fashion and the excision site closed primarily. If the entire circumference of the sigmoid colon at that point is
indurated and woody feeling, a short segmental resection with
anastomosis is the best option.
ILEOCOLIC DISEASE
Approximately half of those diagnosed with Crohn disease have
ileocolic disease. Ileocolic resection is, in fact, the operation most
frequently performed to treat Crohn disease. Currently, there is a
trend toward more aggressive medical management of Crohn disease; at the same time, surgeons are seeing more complicated disease at the time of operation. These developments have implications for management. An easy ileocolic resection is an experience
that a patient generally tolerates well and recovers from very quickly; however, delaying operative management with years of aggressive medical therapy can lead to more complicated disease associated with enteroenteric fistulas, which can be difficult to treat.
Ileosigmoid fistulas are among the most common fistulas associated with ileocolic Crohn disease, along with fistulas between the
terminal ileum and the ascending colon and fistulas between the
terminal ileum and adjacent loops of small bowel.
Disease recurrence is common after ileocolic resection. Colonoscopy is the most accurate modality for postoperative surveillance and
the easiest to use; it is more sensitive than either small bowel followthrough or air-contrast barium enema. For this reason, I favor an
end-to-end anastomosis after ileocolic resection. In the event of recurrent disease, an end-to-side, side-to-end, or side-to-side anastomosis may be difficult to intubate.There is some evidence in the lit-
Figure 6 A large ulcer is nearly always present on the
mesenteric luminal border of small bowel strictures.
© 2004 WebMD, Inc. All rights reserved.
ACS Surgery: Principles and Practice
5 GASTROINTESTINAL TRACT AND ABDOMEN
COLONIC DISEASE
Colonic involvement is present in 29% to 44% of patients with
Crohn disease.30 One of the challenges in treating colonic Crohn
disease is obtaining the correct diagnosis. Whereas Crohn disease
of the small bowel is fairly easy to diagnose, colonic disease often
is not. Because granulomas are not present in most cases of
colonic Crohn disease and because this condition can look very
similar to ulcerative colitis both endoscopically and macroscopically, differentiation between Crohn colitis and ulcerative colitis
can be difficult in the absence of small bowel or anal disease.
Colonic Crohn disease appears to be more frequently associated
with cutaneous manifestations (e.g., pyoderma gangrenosum) [see
Figure 7].
Indications for Surgical Treatment
The main indications for operative management of colonic
Crohn disease are stricture [see Figure 8], malignancy, side effects
of medical therapy, and failure of medical therapy. In children, failure to recognize and treat this condition promptly may result in
growth retardation. It is important to monitor both bone age and
insulinlike growth factor–1 levels. If these are abnormal, timely
institution of human growth hormone therapy, operative management of inflammatory bowel disease, or both may still permit normal growth and development.
Side effects of medical therapy can be substantial. They may include such varied complications as aseptic necrosis of the femoral
head and cataract formation (both related to steroid use), as well as
an increased incidence of opportunistic infections (from immunosuppression secondary to antimetabolite therapy).
Failure of medical therapy can refer to continuing severe disease
activity or, at worst, to so-called toxic megacolon. The term toxic
megacolon is actually a misnomer, in that not all patients with this
condition actually have a true megacolon [see Figure 9a]. In common usage, the term toxic megacolon refers to any condition associated with colitis that is severe enough to result in sloughing of the
a
11 CROHN DISEASE — 6
colonic mucosa; such sloughing permits endotoxins to enter the
circulatory system and evoke a septic response. The signs and
symptoms of toxic megacolon include those characteristic of sepsis—leukocytosis, fever, tachycardia, and hypoalbuminemia.These
patients are very ill and often manifest ileus, which is an ominous
development that frequently signals impending perforation. Emergency surgical intervention is required. At operation, the colon is
often distended, and when the specimen is opened, the colon may
appear almost autolytic [see Figure 9b]. In this state, the bowel frequently does not hold staples well; accordingly, it is often helpful
to sew the distal Hartmann stump between the left and right
halves of the anterior inferior rectus fascia at the lower abdominal
incision and then to close the skin over it.31 Thus, if the staple line
is disrupted, the result is essentially a surgical site infection that
can be opened and drained, rather than the pelvic abscess [see
Figure 9c] that could develop if the rectal stump were located deep
within the pelvis.
Types of Disease
Segmental disease In a 2003 review of 92 consecutive cases
of patients with Crohn colitis, the number of patients with segmental colonic Crohn disease and the number of those with pancolonic disease were nearly equal.30 Approximately 63% of those
with segmental colitis had other disease involvement as well (e.g.,
jejunoileal, ileocolic, or perianal), compared with only 12% of
those with pancolitis. The recurrence rate, however, was higher in
patients with segmental colitis than in those with pancolitis. In
addition, the risk of recurrence was higher in patients who had
granulomatous disease than in those who did not.
Pancolonic disease In cases of pancolonic Crohn disease
with associated perianal, jejunoileal, or ileocolic involvement, diagnosis is not difficult. However, most patients with Crohn pancolitis do not have other sites of disease involvement, nor do they have
granulomas.30 Consequently, differentiation of Crohn pancolitis
b
Figure 7 (a) Shown is pyoderma gangrenosum affecting the peristomal and incisional area 6 months after
creation of a loop ileostomy in a 16-year-old girl who had undergone colectomy with IPAA for a presumed
initial diagnosis of ulcerative colitis. (b) Shown is peristomal gangrenosum of the breast in an otherwise
asymptomatic patient with Crohn colitis and perianal Crohn disease who had a diverting loop ileostomy.
© 2004 WebMD, Inc. All rights reserved.
ACS Surgery: Principles and Practice
5 GASTROINTESTINAL TRACT AND ABDOMEN
11 CROHN DISEASE — 7
a
b
Figure 8 Shown is a sigmoid colon stricture secondary to Crohn
disease that caused obstructing symptoms refractory to medical
therapy.
from ulcerative colitis can be very difficult. Many patients with
Crohn disease have been inappropriately subjected to colectomy
with ileal pouch–anal anastomosis (IPAA) because they were initially presumed to have ulcerative colitis.
Operative Procedures
Total proctocolectomy with end ileostomy The traditional procedure for colonic Crohn disease is total proctocolectomy
with end ileostomy, which is associated with an 8% to 15% rate of
recurrence in the bowel proximal to the stoma.32-34 This operation
remains the best choice in patients with severe rectal and anal
Crohn disease (e.g., those with so-called watering-can perineum
[see Figure 10]) and carries the lowest risk of disease recurrence. In
contrast to the approach taken in patients with rectal cancer,
which involves excising the external anal sphincter and a large portion of the levator muscles, the approach taken in those with
colonic Crohn disease is intersphincteric, with dissection performed in the plane between the internal and external anal
sphincters to reduce the size of the perineal wound and facilitate
healing. Even with the intersphincteric approach, delayed healing
of the perineal wound is common, occurring in as many as 30%
of patients.
Subtotal colectomy with ileorectal or ileosigmoid anastomosis Because many patients with Crohn disease are young,
surgeons have long been interested in operations that do not
involve an ileostomy. In the absence of significant rectal and anal
disease, subtotal colectomy with ileorectal or ileosigmoid anastomosis is an option. Unfortunately, this operation is associated with
high recurrence rates (up to 70%)35; however, with the advent of
more effective immunosuppressive and biologic therapy, it is hoped
that these rates can be reduced. As much palpably normal distal
rectum and colon as possible should be spared. The anastomosis
can be stapled, though if the bowel wall is thickened, many surgeons would feel more secure with a handsewn anastomosis in
either one or two layers.
c
Figure 9 (a) Shown is toxic megacolon in a 17-year-old girl with
Crohn colitis. The colon is massively distended and near perforation
at the time of operation. (b) When the specimen is opened, it is
apparent that large segments of the mucosa have sloughed off, leaving denuded muscle wall. (c) The distal rectosigmoid is incorporated
between the left and right halves of the anterior inferior rectus fasSegmental resection Currently, more surgeons are advocia at the lower abdominal incision and placed underneath the skin,
cating colon-sparing procedures [see 5:34 Segmental Colon Resection] which is then closed over it. Thus, in the event of disruption of the
distal stump, the contents drain harmlessly through the wound.
for Crohn disease. Although this is a relatively new approach,
© 2004 WebMD, Inc. All rights reserved.
ACS Surgery: Principles and Practice
5 GASTROINTESTINAL TRACT AND ABDOMEN
11 CROHN DISEASE — 8
would knowingly perform in a patient with Crohn disease, every
year there are many such patients who undergo this procedure as
treatment of colonic inflammatory bowel disease that initially is
incorrectly presumed to be ulcerative colitis but later is diagnosed as Crohn disease (on the basis of either final pathologic
analysis of the resected specimen or the disease’s clinical behavior). Generally speaking, in the absence of fistulizing disease,
most of these patients are able to maintain their pouch, but they
require medical therapy for disease control.30,37-40
ANAL DISEASE
Types of Disease
Figure 10 Shown is so-called watering-can perineum secondary
to severe perianal Crohn disease.
there have already been some reports documenting the safety of
segmental resection in cases of limited disease.36 In patients with
colonic strictures resulting in obstruction, segmental resection into
palpably normal areas of the bowel yields prompt resolution of
symptoms. Because the colon performs an important water-absorbing function, many patients with a limited amount of small bowel
can still live without intravenous supplementation if a significant
segment of the colon is left in situ. However, patients with segmental Crohn disease appear to have a higher recurrence rate than
those with pancolitis, as do patients with granulomas.30 Surgical
treatment of Crohn disease continues to undergo reevaluation and
reassessment of results on the basis of the availability of newer
medical therapies.
Colectomy with IPAA Although colectomy with IPAA [see
5:33 Procedures for Ulcerative Colitis] is not an operation that one
With stenosis For patients with anal strictures that are not regularly dilated, the outlook is poor. Such strictures pose functional obstructions and typically lead to continuing problems with fistulas and
suppurative disease.They frequently become more and more fibrotic over time and often extend proximally. Most of these patients
eventually require fecal diversion. Management generally involves
self-dilation, which can often be done with Hegar dilators. If the
stenosis is not dealt with, all other treatment of the Crohn disease is
doomed to failure; obstruction at the level of the anal canal inevitably
results in the persistence of anorectal disease.
Without stenosis Anal Crohn disease without stenosis is
much easier to treat medically. Long-term oral metronidazole therapy is often helpful; other medications (e.g., anti–tumor necrosis
factor antibody) may be useful as well. Broad fissures are usually
asymptomatic. Surgical treatment should be avoided unless the
lesions are causing symptoms. Because they tend to have more liquid bowel movements, patients with Crohn disease need an optimally functioning anal sphincter; hence, fistulotomies, which
divide portions of the sphincter, should be avoided if at all possible. Placement of setons through fistula tracts can often prevent
abscess formation, provide drainage, and thereby prevent perianal
pain while minimizing sphincter trauma. Silk sutures, vessel loops,
or Penrose drains also can be used as setons [see Figure 11]. Rectovaginal fistulas pose a particular challenge. In the presence of
active Crohn disease, advancement flap repair of such fistulas has
a low success rate.41 Laparoscopic-assisted loop ileostomy improves
the success rate, but unfortunately, the fistulas may recur when
intestinal continuity is reestablished.
Postoperative Management
CHEMOPROPHYLAXIS
Figure 11 Vessel loops can be used as setons for drainage of
abscesses caused by perianal Crohn disease. They can be left in as
long as necessary and help prevent recurrent abscess formation.
In 1995, a prospective, randomized study showed that patients
who underwent ileocolic resection and were given mesalamine
postoperatively had a significant reduction in both the symptomatic and the endoscopic rate of recurrence.29 Not all of the work
done since then has confirmed these results, but several studies
and a meta-analysis have indicated that mesalamine does reduce
the postoperative recurrence rate of Crohn disease.42 Many patients undergoing surgical treatment of Crohn disease are advised to take some type of postoperative preventive medical therapy—either a 5-ASA derivative (e.g., mesalamine) or a stronger
immunosuppressive agent (e.g., 6-mercaptopurine or azathioprine). Better studies are required to document the efficacy of
the latter agents in preventing recurrence. It is hoped that
chemoprophylaxis will reduce the anticipated recurrence rates
by 30% to 40%.
© 2004 WebMD, Inc. All rights reserved.
ACS Surgery: Principles and Practice
5 GASTROINTESTINAL TRACT AND ABDOMEN
11 CROHN DISEASE — 9
SURVEILLANCE
BEHAVIORAL MODIFICATION
At present, there are no clear guidelines for surveillance after
operative treatment of Crohn disease. In my opinion, however,
given the increased risk of colorectal cancer in this setting,
patients with Crohn disease who retain some colon should
undergo colonoscopy every 2 years, not only to detect any
development of colonic neoplasia but also to identify any recurrence of disease in a timely manner. If recurrent Crohn disease
is detected, appropriate medical therapy should be promptly
instituted, with the aim of avoiding subsequent operation if
possible.
Exposure to cigarette smoke is known to exacerbate the symptoms of Crohn disease. Smoking has been reported to affect the
overall severity of the disease, with smokers having a 34% higher
recurrence rate and a higher rate of reoperation than nonsmokers.43-45 A 1999 study of 141 Crohn disease patients who had
undergone ileocolic resection, of whom 79 were nonsmokers and
the remainder were smokers, found that the respective 5- and 10year recurrence-free rates were 65% and 45% in smokers and 81%
and 64% in nonsmokers. The recurrence rates were higher in
heavy smokers (≥ 15 cigarettes/day) than in moderate smokers.46
References
1. Farmer RG, Hawk WA, Turnbull RB Jr: Clinical
patterns in Crohn’s disease: a statistical study of
615 cases. Gastroenterology 68:627, 1975
2. Gasche C, Scholmerich J, Brynskov J, et al: A
simple classification of Crohn’s disease: report of
the Working Party for the World Congresses of
Gastroenterology, Vienna 1998. Inflamm Bowel
Dis 6:8, 2000
3. Michelassi F, Balestracci T, Chappell R, et al:
Primary and recurrent Crohn’s disease: experience with 1379 patients. Ann Surg 214:230,
1991
4. Bodger K: Cost of illness of Crohn’s disease.
Pharmacoeconomics 20:639, 2002
5. Feagan BG, Vreeland MG, Larson LR, et al:
Annual cost of care for Crohn’s disease: a payor
perspective. Am J Gastroenterol 95:1955, 2000
6. Colombel JF, Loftus EV Jr, Tremaine WJ, et al:
The safety profile of infliximab in patients with
Crohn’s disease: the Mayo clinic experience in
500 patients. Gastroenterology 126:19, 2004
7. Ljung T, Karlen P, Schmidt D, et al: Infliximab in
inflammatory bowel disease: clinical outcome in
a population based cohort from Stockholm
County. Gut 53:849, 2004
8. Crohn BB, Ginzburg L, Oppenheimer GD:
Landmark article Oct 15, 1932. Regional ileitis:
a pathological and clinical entity. By Burril B.
Crohn, Leon Ginzburg, and Gordon D. Oppenheimer. JAMA 251:73, 1984
9. Fazio VW, Marchetti F, Church M, et al: Effect
of resection margins on the recurrence of
Crohn’s disease in the small bowel: a randomized
controlled trial. Ann Surg 224:563, 1996
10. Galandiuk S, O’Neill M, McDonald P, et al: A
century of home parenteral nutrition for Crohn’s
disease. Am J Surg 159:540, 1990
11. Greenstein AJ: Cancer in inflammatory bowel
disease. Mt Sinai J Med 67:227, 2000
12. Rhodes JM, Campbell BJ: Inflammation and colorectal cancer: IBD-associated and sporadic cancer compared. Trends Mol Med 8:10, 2002
13. Gillen CD, Walmsley RS, Prior P, et al: Ulcerative colitis and Crohn’s disease: a comparison of
the colorectal cancer risk in extensive colitis. Gut
35:1590, 1994
14. Milsom JW, Hammerhofer KA, Bohm B, et al:
Prospective, randomized trial comparing laparoscopic vs. conventional surgery for refractory
ileocolic Crohn’s disease. Dis Colon Rectum
44:1, 2001
15. Young-Fadok TM, HallLong K, McConnell EJ,
et al: Advantages of laparoscopic resection for
ileocolic Crohn’s disease: improved outcomes
and reduced costs. Surg Endosc 15:450, 2001
16. Moorthy K, Shaul T, Foley RJ: Factors that predict conversion in patients undergoing laparoscopic surgery for Crohn’s disease. Am J Surg
187:47, 2004
17. Murray JJ, Schoetz DJ Jr, Nugent FW, et al:
Surgical management of Crohn’s disease involving the duodenum. Am J Surg 147:58, 1984
18. Ross TM, Fazio VW, Farmer RG: Long-term
results of surgical treatment for Crohn’s disease
of the duodenum. Ann Surg 197:399, 1983
19. Worsey MJ, Hull T, Ryland L, et al: Strictureplasty is an effective option in the operative management of duodenal Crohn’s disease. Dis Colon
Rectum 42:596, 1999
20. Yamamoto T, Bain IM, Connolly AB, et al:
Outcome of strictureplasty for duodenal Crohn’s
disease. Br J Surg 86:259, 1999
21. Michelassi F, Hurst RD, Melis M, et al: Side-toside isoperistaltic strictureplasty in extensive Crohn’s
disease: a prospective longitudinal study. Ann Surg
232:401, 2000
22. Marshak RH, Wolf BS: Chronic ulcerative granulomatous jejunitis and ileojejunitis. AJR 70:93,
1953
23. Jaskowiak NT, Michelassi F: Adenocarcinoma at
a strictureplasty site in Crohn’s disease: report of
a case. Dis Colon Rectum 44:284, 2001
24. Marchetti F, Fazio VW, Ozuner G: Adenocarcinoma arising from a strictureplasty site in Crohn’s
disease: report of a case. Dis Colon Rectum
39:1315, 1996
25. Dietz DW, Laureti S, Strong SA, et al: Safety and
long-term efficacy of strictureplasty in 314
patients with obstructing small bowel Crohn’s
disease. J Am Coll Surg 192:330, 2001
26. Hamilton SR, Reese J, Pennington L, et al: The
role of resection margin frozen section in the surgical management of Crohn’s disease. Surg
Gynecol Obstet 160:57, 1985
27. Munoz-Juarez M, Yamamoto T, Wolff BG, et al:
Wide-lumen stapled anastomosis vs. conventional end-to-end anastomosis in the treatment of
Crohn’s disease. Dis Colon Rectum 44:20, 2001
28. Greenstein AJ, Sachar DB, Pasternack BS, et al:
Reoperation and recurrence in Crohn’s colitis
and ileocolitis: crude and cumulative rates. N
Engl J Med 293:685, 1975
29. McLeod RS, Wolff BG, Steinhart AH, et al: Prophylactic mesalamine treatment decreases postoperative recurrence of Crohn’s disease. Gastroenterology 109:404, 1995
30. Morpurgo E, Petras R, Kimberling J, et al: Characterization and clinical behavior of Crohn’s disease initially presenting predominantly as colitis.
Dis Colon Rectum 46:918, 2003
tions for primary and recurrent Crohn’s disease
of the large intestine. Surg Gynecol Obstet 148:1,
1979
33. Ritchie JK, Lockhart-Mummery HE: Nonrestorative surgery in the treatment of Crohn’s
disease of the large bowel. Gut 14:263, 1973
34. Goligher JC: The long-term results of excisional
surgery for primary and recurrent Crohn’s disease of the large intestine. Dis Colon Rectum
28:51, 1985
35. Goligher JC: Surgical treatment of Crohn’s disease affecting mainly or entirely the large bowel.
World J Surg 12:186, 1988
36. Allan A, Andrews H, Hilton CJ, et al: Segmental
colonic resection is an appropriate operation for
short skip lesions due to Crohn’s disease in the
colon. World J Surg 13:611, 1989
37. Hyman NH, Fazio VW, Tuckson WB, et al: Consequences of ileal pouch-anal anastomosis for
Crohn’s colitis. Dis Colon Rectum 34:653, 1991
38. Galandiuk S, Scott NA, Dozois RR, et al: Ileal
pouch-anal anastomosis. Reoperation for pouchrelated complications. Ann Surg 212:446, 1990
39. PanisY, Poupard B, Nemeth J, et al: Ileal pouch/anal
anastomosis for Crohn’s disease. Lancet 347:854,
1996
40. Ricart E, Panaccione R, Loftus EV, et al: Successful management of Crohn’s disease of the
ileoanal pouch with infliximab. Gastroenterology
117:429, 1999
41. Sonoda T, Hull T, Piedmonte MR, et al: Outcomes of primary repair of anorectal and rectovaginal fistulas using the endorectal advancement flap. Dis Colon Rectum 45:1622, 2002
42. Achkar JP, Hanauer SB: Medical therapy to
reduce postoperative Crohn’s disease recurrence.
Am J Gastroenterol 95:1139, 2000
43. Duffy LC, Zielezny MA, Marshall JR, et al:
Cigarette smoking and risk of clinical relapse in
patients with Crohn’s disease. Am J Prev Med
6:161, 1990
44. Sutherland LR, Ramcharan S, Bryant H, et al:
Effect of cigarette smoking on recurrence of
Crohn’s disease. Gastroenterology 98:1123, 1990
45. Cottone M, Rosselli M, Orlando A, et al: Smoking habits and recurrence in Crohn’s disease.
Gastroenterology 106:643, 1994
46. Yamamoto T, Keighley MR: The association of
cigarette smoking with a high risk of recurrence
after ileocolonic resection for ileocecal Crohn’s
disease. Surg Today 29:579, 1999
31. Hull T, Fazio VW: Surgery for toxic megacolon.
Mastery of Surgery, 3rd ed. Nyhus LM, Baker
RJ, Frischer JE, Eds. Little Brown & Co, Boston,
1996, p 1437
32. Goligher JC: The outcome of excisional opera-
Acknowledgment
Figures 3 and 4
Tom Moore.