1 TITLE PAGE Title : CT BRAIN OF STROKE IN EVOLUTION – A

TITLE PAGE
Title : CT BRAIN OF STROKE IN EVOLUTION – A CASE REPORT
Authors:
First - Dr. Kurien John (Specialist Registrar)
Second - Dr. Parag Singhal Consultant Physician
Third - Dr. Chris Cook Consutant Radiologist
Weston General Hospital, Weston-super-mare, Somerset BS23 4TQ
1
ABSTRACT
Stroke is a common and important condition in medicine. A 63 year old gentleman presented to the A&E department, with a history of collapse and progressive right sided weakness. Clinically this was a cerebrovascular accident affecting the left hemisphere of the brain causing right hemiplegia. The middle cerebral artery (MCA) sign was missed on the admission computed tomography (CT) of the brain which delayed commencement of treatment. This is an interesting case of stroke in evolution. The authors would like to enlighten health professionals the importance of clinical examination and its interpretation in the light of ambiguous results from investigations.
2
CASE REPORT
Introduction
A 63-year-old gentleman presented to the A&E department, with a history of collapse and progressive right sided weakness. He was on Bendrofluazide and Atenolol for hypertension which was controlled.
On examination, he was fully conscious and haemodynamically stable with a blood pressure of 105/72. Systemic examination was normal. Power was 3/5 in the right arm and leg with the right plantar reflex up-going. This progressed to 0/5 in 24 hours.
The ECG confirmed sinus rhythm at 60 beats per minute. The chest X-ray was unremarkable.
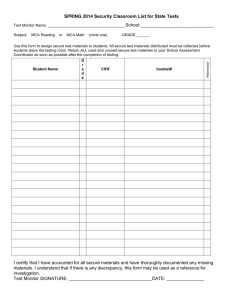
The patient was assumed to have had a cerebrovascular accident (CVA) and underwent computed tomography (CT) of the brain. Initial CT (Fig A) was done within 6 hours of collapse.
However, it was not thought that the CT appearances reflected the patient’s clinical state. Consequently, a repeat CT brain was performed 3 days after admission (Fig B).
Discussion
CT of the brain is invariably performed in the evaluation of patients presenting with clinical signs of cerebrovascular accident. The Royal College of Radiologists guidelines now suggest that such scans should be performed within the initial 48 hours of presentation.
The CT scanning of such patients is performed without the use of intravenous contrast
(unenhanced) thus avoiding potential confusion with subarachnoid haemorrhage.
Below, we summarise the findings and analysis of CT scanning of the brain.
Normal Brain and Fundamentals of CT Interpretation
The brain normal grey/white matter differentiation should be examined; remembering that the fatty content of the myelin containing white matter appears to be of lower density (darker) than the overlying grey matter. The cerebrospinal fluid(CSF) spaces are reviewed for symmetry and it should be ensured that the midline remains central.
Areas of abnormal calcification (white) may be seen within the choroid plexus and occasionally within the basal ganglia.
Acute haemorrhage appears as an area of high density(white). There is often surrounding low density oedema with associated mass effect. Over the subsequent 7
3
to 10 days this high density changes in appearance to become isodense with brain and ultimately (at least a month) to appear as an area of low density.
In cases of acute infarction, the area of infarct is seen as low density within the vascular territory involved. There may be secondary oedema causing mass effect in the acute phase of infarction. However, an immediate CT brain in such cases may initially appear normal. On close examination however, high density within the middle cerebral artery(MCA) may occasionally be seen.[1] This is due to thrombus within this vessel and indicates the likely development of an extensive MCA infarction before it is detected clinically.[2] Similarly, the normal grey-white matter differential pattern may not be apparent due to cerebral anoxia causing tissue oedema.
This patient’s initial scan demonstrated high density within basal ganglia on the right side (not visible in Figure A as the scan slice is few millimetres above, but is seen in
Figure B). This is not in keeping with the patient’s clinical signs (right sided weakness) and is too dense to represent blood and shows no surrounding oedema. It is therefore more typical of incidental calcification within the basal ganglia. Close review of this scan (Figure A) however does demonstrate increased density within the left MCA. This is the “MCA hyper dense sign” and suggests that this patient is developing complete infarction of his left MCA territory. These appearances are in keeping with the patient’s clinical presentation.
The second scan (Figure B) three days later confirms there is now extensive low density throughout the left MCA territory. These are the appearances of established complete infarction. As expected, there has been no change to the probable longstanding calcification within the right basal ganglia.
Final diagnosis
The appearances are those of extensive left MCA infarction.[3] Although the first scan would initially appear to be normal, hyper density due to thrombus is seen within the left MCA.[4] The dense calcification within the basal ganglia on the right side is entirely incidental.
Conclusion
Consideration for thrombolytic therapy is usually within 3 hours of presentation but it should be administered only in experienced specialised units with specific protocols in place.[5]
Due to the suspicion of basal ganglia bleed, aspirin was withheld in this patient until after the second scan. He was then treated with aspirin 300 mg for 2 weeks and thereafter continued on 75 mg.[6] Following 8 months of physiotherapy and rehabilitation he was fully independent.
According to the new stroke guidelines, aspirin and antiplatelet agents should be initiated as soon as haemorrhage is ruled out by confirmatory CT scan.
This case illustrates the significance of a rare radiological sign of evolving stroke, the importance of correlating signs on clinical examination in the presence of ambiguous results from investigations.
4
References
1. Petitti N. The hyper dense middle cerebral artery sign. Radiology
1998;208:687-688
2. Koo C.K. et al What constitutes a true hyper dense middle cerebral artery sign. Cerebrovasc Dis 2000;10:419-423
3. Manno E.M. et al Computed Tomography determinants of neurological deterioration in patients with large middle cerebral artery infarctions. Mayo
Clinic Proc 2003 Feb;78(2):156-60
4. Barber P.A. et al Hyper dense sylvian fissure middle cerebral artery dot sign:
A CT marker of acute ischemia. Stroke 2001 Jan;32(1):84-88
5. Burger K.M. et al Antithrombotic trials in acute ischemic stroke: a selective review. Expert Opin Emerg Drugs 2004 Nov; 9(2):303-12
6. The International Stroke Trial Collaborative Group 1997 A randomised trial of aspirin, subcutaneous heparin, both or neither among 19,435 patients with acute ischemic stroke. Lancet 1997;349:1569-81
Legends
Figure A – CT brain
Figure B – CT brain
Consent
Written consent obtained from patient
Competing interest
The authors declare that they have no competing interests.
Contribution
Dr. Kurien John - Preparation of the manuscript
Dr. Parag Singhal - Physician with inpatient care for the patient while in hospital.
Dr. Chris Cook - Radiologist reported the scan.
5
Figure 1
Figure 2