validation of 1d model of the systemic arterial tree including the
advertisement
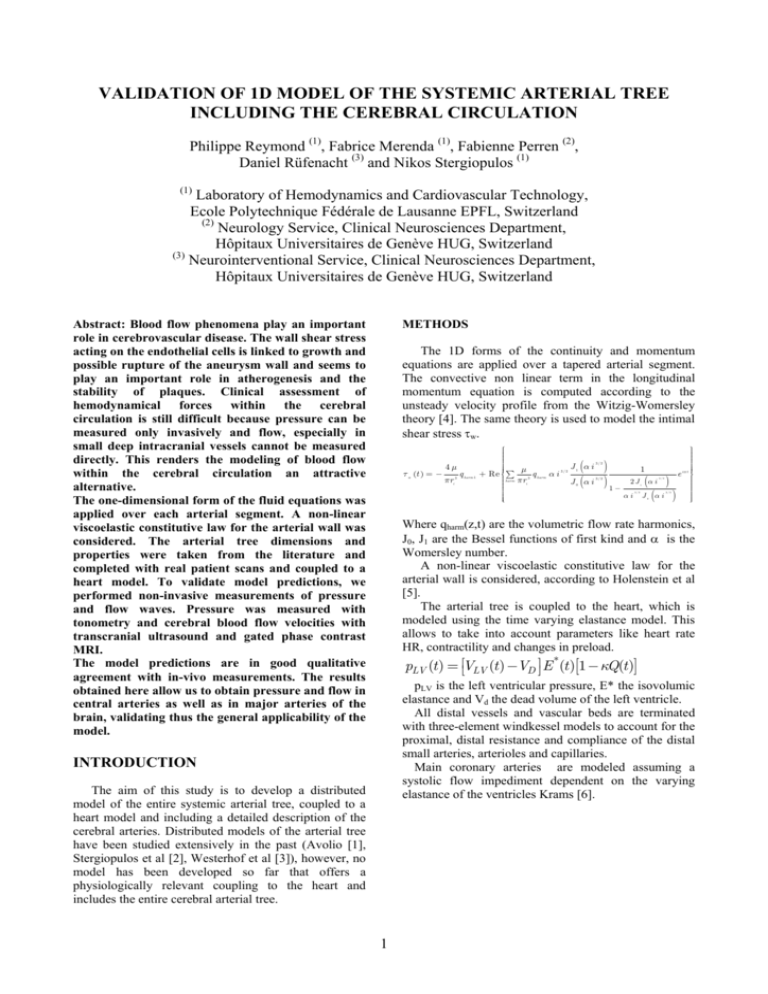
VALIDATION OF 1D MODEL OF THE SYSTEMIC ARTERIAL TREE INCLUDING THE CEREBRAL CIRCULATION Philippe Reymond (1), Fabrice Merenda (1), Fabienne Perren (2), Daniel Rüfenacht (3) and Nikos Stergiopulos (1) (1) Laboratory of Hemodynamics and Cardiovascular Technology, Ecole Polytechnique Fédérale de Lausanne EPFL, Switzerland (2) Neurology Service, Clinical Neurosciences Department, Hôpitaux Universitaires de Genève HUG, Switzerland (3) Neurointerventional Service, Clinical Neurosciences Department, Hôpitaux Universitaires de Genève HUG, Switzerland METHODS Abstract: Blood flow phenomena play an important role in cerebrovascular disease. The wall shear stress acting on the endothelial cells is linked to growth and possible rupture of the aneurysm wall and seems to play an important role in atherogenesis and the stability of plaques. Clinical assessment of hemodynamical forces within the cerebral circulation is still difficult because pressure can be measured only invasively and flow, especially in small deep intracranial vessels cannot be measured directly. This renders the modeling of blood flow within the cerebral circulation an attractive alternative. The one-dimensional form of the fluid equations was applied over each arterial segment. A non-linear viscoelastic constitutive law for the arterial wall was considered. The arterial tree dimensions and properties were taken from the literature and completed with real patient scans and coupled to a heart model. To validate model predictions, we performed non-invasive measurements of pressure and flow waves. Pressure was measured with tonometry and cerebral blood flow velocities with transcranial ultrasound and gated phase contrast MRI. The model predictions are in good qualitative agreement with in-vivo measurements. The results obtained here allow us to obtain pressure and flow in central arteries as well as in major arteries of the brain, validating thus the general applicability of the model. The 1D forms of the continuity and momentum equations are applied over a tapered arterial segment. The convective non linear term in the longitudinal momentum equation is computed according to the unsteady velocity profile from the Witzig-Womersley theory [4]. The same theory is used to model the intimal shear stress τw. τ w (t ) = − 4μ πri 3 q harm 1 ⎧ ⎫ ⎪ ⎪ ⎪ ⎪ ⎪ ⎪ 3/2 ⎪ ⎪ ⎪ ⎪ J α i 1 μ 1 ⎪ ⎪ 3/2 i ϖt ⎪ ⎪ + Re ⎨ ∑ e ⎬ q harm α i 3 3/2 ⎪ harm πri ⎪ 2 J (α i ) J0 αi ⎪ ⎪ ⎪ ⎪ 1− ⎪ ⎪ ⎪ ⎪ α i J (α i ) ⎪ ⎪ ⎪ ⎪ ⎩ ⎭ ( ( ) ) 3/2 1 3/2 3/2 0 Where qharm(z,t) are the volumetric flow rate harmonics, J0, J1 are the Bessel functions of first kind and α is the Womersley number. A non-linear viscoelastic constitutive law for the arterial wall is considered, according to Holenstein et al [5]. The arterial tree is coupled to the heart, which is modeled using the time varying elastance model. This allows to take into account parameters like heart rate HR, contractility and changes in preload. pLV (t ) = ⎡⎣VLV (t ) −VD ⎤⎦ E *(t )[1 − κQ(t )] pLV is the left ventricular pressure, E* the isovolumic elastance and Vd the dead volume of the left ventricle. All distal vessels and vascular beds are terminated with three-element windkessel models to account for the proximal, distal resistance and compliance of the distal small arteries, arterioles and capillaries. Main coronary arteries are modeled assuming a systolic flow impediment dependent on the varying elastance of the ventricles Krams [6]. INTRODUCTION The aim of this study is to develop a distributed model of the entire systemic arterial tree, coupled to a heart model and including a detailed description of the cerebral arteries. Distributed models of the arterial tree have been studied extensively in the past (Avolio [1], Stergiopulos et al [2], Westerhof et al [3]), however, no model has been developed so far that offers a physiologically relevant coupling to the heart and includes the entire cerebral arterial tree. 1 A B Figure 1. Arterial tree of major systemic arteries, based of the Stergiopulos et al. [2] tree (A) connected to a detailed cerebral arterial tree added (B). The arterial tree dimensions and properties were taken from Stergiopulos [2] and extended to include a detailed description of the cerebral arterial tree (Fig. 1). Geometry of the cerebral arterial network was obtained from real patient scans, whereas their elastic properties were taken from values reported in the literature [7]. The set of equations with the boundary conditions described above are solved using an implicit finite difference scheme to yield pressure and flow waveforms over the entire arterial tree. To validate the model predictions for the main systemic arteries and cerebral circulation, we performed noninvasive measurements in young volunteers. Pressure waveforms were measured using applanation tonometry on carotid and superficial temporal arteries. Flow rate waveforms were measured in common, internal carotid and middle cerebral arteries using transcranial Doppler and in systemic arteries (Asc. ao., Thoracic ao., Abdominal Ao., Iliac a., Femoral a. and Common Carotid a.) using gated phase contrast MRI. Figure 2: Model predictions (bottom panels) compared to in vivo measurements of flow and pressure waves (top panels) at various systemic and cerebral arteries. Flow is measured with transcranial ultrasound in the MCA (A) and with MRI in the main systemic arteries (C, D, E and F). Pressure was measured with applanation tonometry in the superficial temporal artery (B). RESULTS AND DISCUSSION The model predicts pressure and flow waves which are in good qualitative agreement with in-vivo measurements (Fig. 2). The agreement is especially good for the shape and wave details of the flow wave, where all features are reproduced in a rather faithful manner. The results obtained here allow us to that model predictions of pressure and flow in central arteries as well as in major arteries of the brain are in good agreement with measurements, validating thus the general applicability of the 1D model to the entire systemic and cerebral circulation. 2 when the pressure gradient is known," The Journal of physiology, 127(3), pp. 553-563. 5. Holenstein, R., Niederer, P., and Anliker, M., 1980, "A viscoelastic model for use in predicting arterial pulse waves," Journal of biomechanical engineering, 102(4), pp. 318-325. 6. Krams, R., Sipkema, P., and Westerhof, N., 1989, "Varying elastance concept may explain coronary systolic flow impediment," The American journal of physiology, 257(5 Pt 2), pp. H1471-1479. 7. Hayashi, K., Handa, H., Nagasawa, S., Okumura, A., and Moritake, K., 1980, "Stiffness and elastic behavior of human intracranial and extracranial arteries," Journal of biomechanics, 13(2), pp. 175-184. REFERENCES 1. Avolio, A. P., 1980, "Multi-branched model of the human arterial system," Med Biol Eng Comput, 18(6), pp. 709-718. 2. Stergiopulos, N., Young, D. F., and Rogge, T. R., 1992, "Computer simulation of arterial flow with applications to arterial and aortic stenoses," Journal of biomechanics, 25(12), pp. 1477-1488. 3. Westerhof, N., Bosman, F., De Vries, C. J., and Noordergraaf, A., 1969, "Analog studies of the human systemic arterial tree," Journal of biomechanics, 2(2), pp. 121-143. 4. Womersley, J. R., 1955, "Method for the calculation of velocity, rate of flow and viscous drag in arteries 3