ACUTE ARTERIAL OCCLUSION
advertisement

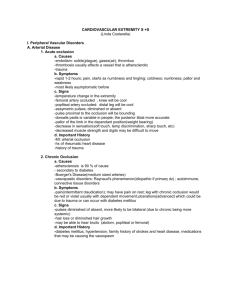
ACUTE ARTERIAL OCCLUSION Patrick Nee BACKGROUND Peripheral vascular disease (PVD) is a generalised disease, usually caused by atherosclerosis. The major vessels of the arterial system are usually affected, especially the superficial femoral artery. Diabetes, Buergher’s disease and the vasculitides cause narrowing of the smaller vessels. Ten per cent of males over 65 may report symptoms (intermittent claudication). Most patients also have coronary heart disease and cerebrovascular disease, leading to death in 20% of arteriopaths from MI or stroke within 5 years of diagnosis. HISTORY Determine the background history of claudication; duration and frequency and severity of attacks, walking distance, rest pain. Enquire about buttock pain, impotence (Leriche syndrome). Could lumbar spinal stenosis be contributing to symptoms? Enquire about associated cardiac, cerebral or intestinal symptoms. Family history, diabetes, hypertension, hyperlipidaemia, drugs (e.g. beta blockers) and smoking history should be noted. EXAMINATION Look for evidence of atherosclerosis (arcus, xanthelasmata, tendon xanthomata) and polycythaemia. General examination should include temperature, pulse (AF?) and BP in both arms. Evaluate for cardiac murmur, abdominal aneurysm. Specific examination of the limbs includes skin colour, temperature, loss of digit pulp and skin appendages, ulceration or gangrenous change. Determine for arterial pulses (diminished, or augmented by aneurysm) and record findings. Doppler ultrasound may be required to identify the femoral, popliteal, PTA and DP pulses. Ankle Doppler pressure may be compared to the brachial pressure. Record the ankle / brachial ratio. Raise the patient’s legs to 60 degrees and observe for pallor. Now allow the legs to hang down and note the time taken for the veins to fill. This should occur within 10 seconds. Order ECG and CXR. Draw bloods for FBC, U&E, PV. ACUTE ARTERIAL OCCLUSION DIAGNOSIS. A clinical diagnosis: Pain, pallor, pulselessness, paralysis, paraesthesia and perishing (cold). Sometimes due to embolus from the heart; MI, AF, valvular heart disease. Less commonly due to atheroma, infective endocarditis or trauma. Palpate for AAA TREATMENT. Treatment includes oxygen, IV fluids, morphine and the management of arrhythmias. Start IV Heparin; 5000 unit bolus over 5 minutes, followed by infusion1400 units(2.8ml) per hour (25000units /50ml). Adjust to maintain APTT 2-3. See emergency Prescribing handbook. Refer surgically for embolectomy.