MECHINICAL VENTILATION Spontaneous respiration vs
advertisement

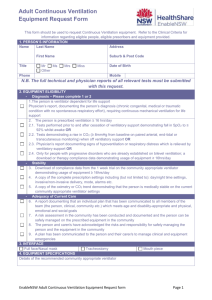
MECHINICAL VENTILATION S. Kache, MD Spontaneous respiration vs. Mechanical ventilation Natural spontaneous ventilation occurs when the respiratory muscles, diaphragm and intercostal muscles pull on the rib cage open, creating a negative inspiratory pressure. This leads to lung expansion and the pulling of air into the alveoli allowing gas exchange to occur. Therefore, spontaneous respiration occurs by negative inspiratory force. Once a patient is intubated, the endo-tracheal tube (ETT) is connected to the ventilator. Depending on the type of ventilator, positive pressure ventilation is provided either by a pneumatic or electric device. The compressed air entering at the alveolar level allows for gas exchange. The significant difference between spontaneous respiration and mechanical ventilation is that during spontaneous respiration, air is pulled into the lungs where as during mechanical ventilation, air is pushed into the lungs. This difference impacts cardio-pulmonary dynamics, as well as the integrity of lung tissue with the potential for long-term injury. Initiating Mechanical Ventilation (See previous chapter for specifics of intubating a patient.) There are essentially three reasons patients require endo-tracheal intubation and initiation of mechanical ventilation • Hypoxia • Hypercarbia • Inability to protect their airway • (To decrease the demand created by the work of breathing in patients with poor cardiac output – e.g. cardiomyopathy. Note that this is the only non-respiratory reason to intubate a patient.) Pulmonary Compliance Compliance = Volume Pressure This simple formula is worth memorizing since it provides the basis of understanding pulmonary and ventilator interactions. By tracking some simple ventilator parameters, this equation allows the physician to monitor patient progression or recovery from the primary disease process. Mechanical Ventialtion 1 Conventional Ventilation Parameters of the Ventilator Important terms regarding conventional ventilation are listed below. Abbreviation Term PIP Peak inspiratory pressure PEEP Positive end expiratory pressure Delta Pressure ∆P Vt Tidal Volume It Et MAP Inspiratory time Expiratory time Mean airway pressure R Rate Definition Point of maximal airway pressure Pressure maintained in airways at end of exhalation Difference between PIP – PEEP Volume of gas entering patient’s lung during inspiration Duration of time in inspiration Duration of time in expiration An average of the airway pressure throughout the respiratory cycle Respiratory rate as set on the ventilator Modes of Ventilation There are several ways the modes of ventilation can be divided. One method is by assessing the amount of support the ventilator is providing for the patient. • Assist control (AC): This mode provides the maximal support for the patient. Every breath, whether mechanical or spontaneous, is fully supported. Each breath has the same PIP or Vt and It. Pressure support is unnecessary in this mode. • Synchronized intermittent mandatory ventilation (SIMV): This mode can provide minimal to moderate amounts of ventilatory support. The ventilator breaths as determined by the set respiratory rate are fully supported breaths. These ventilator breaths deliver the set PIP or Vt and the set It. All spontaneous breaths above the set ventilator rate only receive the set pressure support. As the set ventilator rate is weaned, the patient is forced to do more of the work of breathing. Should the patient tolerate a minimal rate without developing respiratory distress, s/he may be ready for extubation. • Continuous positive airway pressure (CPAP): In this mode, no ventilator breaths are provided; only the CPAP or PEEP and pressure support are set. Note that the amount of support provided is determined by the level at which the pressure support is set. With a minimal pressure support, Mechanical Ventialtion 2 this mode provides the minimal amount of support and the patient is forced to do all the work of breathing. This is an ideal mode to test for an adequate respiratory drive, particularly in patients with impaired neurologic status, either from an underlying disorder or from oversedation. A second method of dividing modes of ventilation is by the mechanism that the ventilator actually provides support for the patient. • Pressure Mode: In this mode, the operator sets the PIP and the machine determines the volume delivered to the patient based on the patient’s pulmonary compliance (Compliance = Volume / Pressure). As the patient’s compliance improves, the tidal volume delivered by the ventilator per breath will increase; conversely as compliance worsens the tidal volume delivered decreases. This mode can be used both in AC or SIMV. The greatest advantage of the pressure mode is that it provides greater ventilatory support by using a decelerating flow pattern, and for stiff, noncompliant lungs, this is the preferred mode of ventilation. The disadvantage is the minute ventilation is not guaranteed. • Volume Mode: The operator sets the tidal volume and the ventilator determines the pressure required based on the pulmonary compliance (Compliance = Volume / Pressure). As the compliance improves, the PIP required to deliver the set tidal volume decreases; conversely as the compliance worsens the PIP required increases. The volume mode can be used both in AC or SIMV. The advantage of the volume mode is that a minute volume is guaranteed. The drawbacks are that it cannot be used in a patient with a large leak around the ETT and it is not optimal for poorly compliant lungs. Hypoxia There are six major causes of poor oxygen delivery to tissues: • Decreased alveolar PaO2 • Shunts • Diffusion impairment • V/Q mismatch • Hemoglobin abnormalities • Poor cardiac output Decreased alveolar PaO2 can occur secondary to poor patient respiratory effort as seen in over-sedated patients with hypoventilation. It may also occur because of decreased ambient oxygen as observed at high altitudes (i.e. the top of Mt. Everest at 29,035ft has an oxygen level 33% of that at sea level due to the change in barometric pressure from 760 mm Hg to 253 mm Hg.) Mechanical Ventialtion 3 Shunts can be either intra-cardiac or intra-pulmonary. An intra-cardiac right-toleft shunt causes hypoxia that is unresponsive to oxygen therapy. An intrapulmonary shunt represents a portion of lung that has blood flow without air exchange, causing a right-to-left shunt of de-oxygenated blood. A diffusion impairment is an abnormality at the alveolar capillary level preventing oxygen from entering the blood stream. Examples include fibrotic thickening or interstitial edema. Large areas of lung with V/Q mismatch can also lead to hypoxia. Managing Hypoxia / Hypercarbia If an intubated patient should develop hypoxia, it can by treated by either increasing the mean airway pressure or the FiO2. Mean airway pressure is determined by PIP, PEEP, respiratory rate, I-time, and E-time. Of all these factors, increasing the PEEP is usually the most effective since it can re-recruit atelectatic areas. Caution should be taken to not over-distend the lungs while increasing the PEEP since it can convert normal West zone 2 areas of the lung to zone 1 areas with ventilation and no perfusion. Should the patient have non-compliant lungs, consider using a lung protective strategy (see section on ARDS). Increasing the FiO2 can also improve oxygenation. However, FiO2 greater than 60% can be toxic to the lungs due to increased oxygen free radicals. Short-term oxygen toxicity can lead to reversible pulmonary problems such as edema, which can worsen pulmonary compliance. Prolonged oxygen toxicity can cause irreversible pulmonary destruction. Therefore, other vent settings should be optimized to decrease FiO2 to less than 60% or lower oxygen saturations should be accepted. Hypercarbia Unlike hypoxia, hypercarbia has only a single causative agent: decreased minute ventilation. A patient’s minute ventilation is determined by the respiratory rate in a given minute and the tidal volume per breath. Be cautious of patients on excess carbohydrates since this will increase CO2 production and may prolong intubation or increase the amount of support required on the ventilator. Managing Hypercarbia Elevated CO2 in an intubated patient is treated by increasing minute ventilation, i.e. increasing the respiratory rate or the tidal volume. If the respiratory rate on the ventilator is increased, one should monitor for possible air trapping, i.e. not allowing adequate time to exhale. Air trapping will only amplify the hypercarbia rather than treating it. Although the tidal volume can be increased to treat hypercarbia, it should not be increased above 10ml/kg/breath due to the risk of volutrauma. Mechanical Ventialtion 4 Obstructive Pulmonary Disease An obstructive disease is defined as any process causing airway obstruction and increased resistance to airflow. The most common obstructive disease in the pediatric population is asthma. The obstructed airways make exhalation difficult; therefore, optimize expiratory time to allow for complete exhalation. The CO2 does not need to be normalized immediately after intubation. Allow for permissive hypercapnia if required; the CO2 will normalize as the patient’s primary disease process begins to resolve. At times patients will need an I:E ratio as high as 1:5. Also be sure to bag the patient slowly immediately after intubation if you are managing the patient until s/he is transferred to the PICU. Bagging at a high respiratory rate will exacerbate the air trapping and place the patient at risk of developing a pneumothorax. Restrictive Pulmonary Disease Compromised lung volume secondary to intrinsic lung disease or external compression is considered a restrictive pulmonary process. A pneumonic process, focal atelectasis, or a pleural effusion are all examples. Patients should be managed by optimizing V/Q matching. Assure that a lung protective strategy is followed particularly while managing a patient with a restrictive process (see section on ARDS). High Frequency Ventilation Theory of Functioning The lungs have a natural resonant frequency. High velocity inspiratory gas flow is used to overcome airway resistance in order to oxygenate and ventilate the patient. Some theories to explain gas exchange with this form of ventilation include conventional bulk flow, coaxial flow, Taylor dispersion, and the Pendelluft phenomenon. High frequency ventilation also differs from conventional ventilation in that it utilizes active exhalation as opposed to passive exhalation. Parameters of the Ventilator Some of the terms needed to understand high frequency ventilation are listed below. Abbreviation Term MAP Mean Airway Pressure Amp Amplitude Hz I-time Hertz Inspiratory time FiO2 Fraction of inspired oxygen Definition Pressure maintained throughout the respiratory cycle Rise and fall around MAP consisting of one cycle Number of cycles per second Amount of time spent in inspiration during a given cycle; usually set at 33% Can range from 21% to 100% Mechanical Ventialtion 5 Transitioning a patient to high frequency ventilation can be considered either for difficulty oxygenating or ventilating on conventional ventilation. The MAP usually is set 2-6 cm H2O above conventional ventilation on the high frequency ventilator. The amplitude should be based on the patient’s chest “wiggle.” The hertz can vary from 3 –12 cycles per second. In the PICU population, the hertz is usually set at 8 or below. If the patient is at 3Hz, a MAP of 20 or lower, and FiO2 at 50% or lower, transitioning back to conventional ventilation can be considered. Managing Hypoxia / Hypercarbia If a patient is hypoxic, either the MAP or FiO2 can be increased. Use the chest Xray to adjust the MAP. The patient should have a lung expansion of 7-9 ribs on X-ray. If the FiO2 is increased, be cautious of possible oxygen toxicity as discussed above. On very rare occasions, one can consider increasing the I-time. If the patient is hypercarbic, consider either increasing the amplitude or DECREASING the hertz. Although this seems counter-intuitive, decreasing the hertz actually treats hypercarbia for patients on high frequency ventilation. Mechanical Ventialtion 6